| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 2012年第26期——宫颈刮出物(已点评)
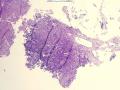
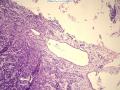
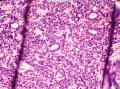
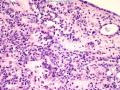
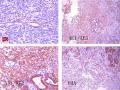
- 图1
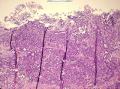
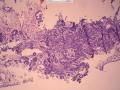
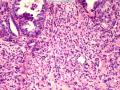
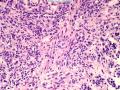
- 图2
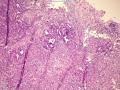
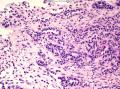
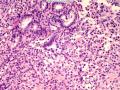
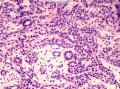
- 图3
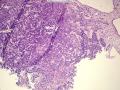
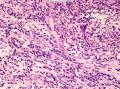
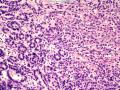
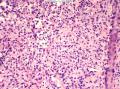
- 图4
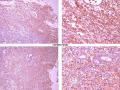
- 图5
- 图6
- 图7
- 图8
- 图9
- 图10
- 图11
- 图12
- 图13
- 图14
- 图15
- 图16
- 图17
- 图18
- 图19
- 图20
- 图21
- 图22
- 图23
- 图24
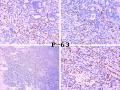
- 图25
- 图26
- 图27
- 图28
| 性别 | 女 | 年龄 | 63岁 | 临床诊断 | 子宫内膜病变? |
|---|---|---|---|---|---|
| 临床症状 | 绝经4年后阴道流血 | ||||
| 标本名称 | 宫颈刮出物(内膜刮出物呈增生反应) | ||||
| 大体所见 | 灰红色碎组织1堆,0.5cm。 | ||||
本例图片采用麦克奥迪MoticBA410显微镜+MoticamPro285A摄像头采集制作。
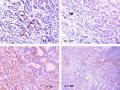
2012-7-11 附免疫组化图片:
点评专家:笪冀平(60楼 链接:>>点击查看<< )
获奖名单:无(59楼 链接:>>点击查看<< )
-
本帖最后由 筷子 于 2012-08-31 16:06:26 编辑

知之者不如好之者,好之者不如乐之者。(语出幽梦影)
本例可能为罕见病例。个人意见考虑神经内分泌肿瘤,可能为分化较好的类癌(虽然典型类癌在宫颈几乎不见)。
依据:老年女性,绝经后出血;镜下见肿瘤呈器官样结构排列,腺管状、实性片状、小梁状及条索状,部分区域可见不典型“菊形团”样结构;细胞形态相对温和,核染色质细腻。
免疫组化:神经内分泌标记物,cgA、NSE、syn等。
鉴别诊断:
1、宫颈子宫内膜间质肉瘤。本例特征性血管结构不明显。
2、混合性上皮和间叶肿瘤:腺肉瘤、肾外wilms瘤。本例上皮组成及“间质”表现可以与前者鉴别;本例虽有小管状结构,但缺乏胚胎性成分,与后者鉴别。
3、中肾管残件腺体非典型增生/腺癌。本例缺乏“管腔”内的嗜伊红物质,小管状结构上皮增生不显著。
4、其它及转移性肿瘤:恶黑、小细胞癌、乳腺癌转移等。
您的考虑很全面,也和本例的形态很相关,厉害。本例我看了很久之后并查阅了好几本资料才下决定,非典型类癌我差点考虑为第一诊断,关于非典型类癌WHO上面有图有真相 ,但总感觉血管形态不够神经内分泌肿瘤。本例间质成分看上去有点界限不清,所以腺肉瘤/癌肉瘤,Wilm‘s瘤都有符合的一些形态特征,总之,您的考虑我个人认为很全面
,但总感觉血管形态不够神经内分泌肿瘤。本例间质成分看上去有点界限不清,所以腺肉瘤/癌肉瘤,Wilm‘s瘤都有符合的一些形态特征,总之,您的考虑我个人认为很全面
本例可能为罕见病例。个人意见考虑神经内分泌肿瘤,可能为分化较好的类癌(虽然典型类癌在宫颈几乎不见)。
依据:老年女性,绝经后出血;镜下见肿瘤呈器官样结构排列,腺管状、实性片状、小梁状及条索状,部分区域可见不典型“菊形团”样结构;细胞形态相对温和,核染色质细腻。
免疫组化:神经内分泌标记物,cgA、NSE、syn等。
鉴别诊断:
1、宫颈子宫内膜间质肉瘤。本例特征性血管结构不明显。
2、混合性上皮和间叶肿瘤:腺肉瘤、肾外wilms瘤。本例上皮组成及“间质”表现可以与前者鉴别;本例虽有小管状结构,但缺乏胚胎性成分,与后者鉴别。
3、中肾管残件腺体非典型增生/腺癌。本例缺乏“管腔”内的嗜伊红物质,小管状结构上皮增生不显著。
4、其它及转移性肿瘤:恶黑、小细胞癌、乳腺癌转移等。

- 当你有选择的时候,不是选择正确的,而是选择不让你后悔的!
-
wangdingding 离线
- 帖子:1474
- 粉蓝豆:98
- 经验:6042
- 注册时间:2006-10-19
- 加关注 | 发消息
-
本帖最后由 TK1905 于 2012-06-29 23:03:18 编辑
考虑:中肾管腺癌
依据:临床为老年女性,绝经后阴道流血,镜下:低倍宫颈管粘膜及粘膜下弥漫小管或梁状、实性结构腺上皮浸润生长,中高倍可见肿瘤细胞为立方、低柱状上皮,无胞浆内粘液,无明显腺腔内嗜酸性分泌物(本来这个是良性的中肾管诊断线索,本例真的不明显),核轻度异形性,核分裂不易见,结构为小管、大管、性索样梁状浸润间质,或实性,间质有反应性增生,提示恶性可能
IHC:PAX2、CD10、CR、CK7、vim、Ki-67
引:
Mesonephric adenocarcinoma of cervix
Very rare; <50 cases reported
Arise from remnants of mesonephric (Wolffian) ducts, which form epididymis and vas deferens in males and persist in females as rete ovarii, paraoophoron and Gartner’s duct
Mean age 52 years, range 35 to 72 years
Usually presents with abnormal vaginal bleeding, stage IB disease; some are higher stage and aggressive
Adjacent to areas of mesonephric hyperplasia
Appears to arise from “lower zone” of Wolffian system, in contrast to female adnexal tumors of probable Wolffian origin (upper zone)
Immunophenotype resembles mesonephric remnants of cervix and vagina (EMA+, CK7+, ER-, PR-, AJSP 2001;25:379)
May have better prognosis than mullerian counterparts (AJSP 2004;28:601)
Gross: often along lateral cervix within fibromuscular stroma
Micro: small tubules or ducts (most common), also retiform, solid, sex-cord like and spindled; glands may be endometrioid; may have eosinophilic secretions seen in mesonephric rests; often lined by cuboidal or low columnar cells with malignant nuclei but no intracytoplasmic mucin; mild to moderate nuclear atypia; usually adjacent hyperplastic mesonephric remnants; surface epithelium is not involved; desmoplastic stroma is not prominent
Positive stains: AE1/AE3, CAM5.2, CK1, CK7, EMA (100%), calretinin (88%), vimentin (70%), CD10 (AJSP 2003;27:178), androgen receptor (33%), inhibin (30%, focal), Ki-67 (15%)
Negative stains: CK20, ER, PR, CEA
DD:
mesonephric hyperplasia - usually incidental finding with lobular and noninfiltrative patterns, minimal atypia, minimal mitotic activity, no solid/ductal patterns, no angiolymphatic invasion, no necrotic luminal debris
endometrioid adenocarcinoma - usually high grade, involves surface epithelium and deep cervical stroma, no mesonephric hyperplasia, ER+, PR+, CEA+, vimentin-
malignant mixed mullerian tumor - high grade atypia, distinct demarcation between glandular and stromal components
clear cell carcinoma of mullerian origin - often associated with DES exposure; tubulocytic or papillary pattern with clear and hobnail cells