| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 2013年第27期(总第79期)——左侧乳腺肿块(已点评)
| 性别 | 女 | 年龄 | 36 | 临床诊断 | 乳腺纤维腺瘤 |
|---|---|---|---|---|---|
| 一般病史 | 体检发现左侧乳房肿块,活动可,影像学未见钙化影,提示纤维腺瘤。 | ||||
| 标本名称 | 乳腺肿块切除标本 | ||||
| 大体所见 | 灰白灰红色不规则组织一块,2.5cm×2cm×1.5cm,切面大部呈亮白色,质地韧。 | ||||
点评专家:薛德彬(181、182楼 链接:>>点击查看<< )
-
本帖最后由 草原 于 2014-05-07 09:29:58 编辑

知之者不如好之者,好之者不如乐之者。(语出幽梦影)

- 26
-

zhouyanx.. -

周淑霞 -

liuzixua.. -

我佛慈悲 -

shixiaop.. -

Eliend -

大雪素 -

sfh -

huocheng.. -

shuchao -

真诚 -

zhangxl -

爱飞的芦.. -

喀什市人.. -
病理芯片 -

熊猫骑士 -

糊涂散人 -
QQ小丽 -
connie -

12422676..
-
www810910: 病理工作者应该感谢华夏病理给病理工作者这样一个很好的学习平台!2013-09-29 10:29
-
suoyanlee: 是的,感谢各位老师辛勤的工作。2013-10-01 12:27
-
zhouyanxia: 真诚说一声:谢谢!2013-10-09 11:55
-
学海无涯123: 乳腺大部分小叶呈腺病改变,小叶周边间质内可见高度异性的细胞,可见疑似小管样,偶可见单个细胞形成的小管样,管内似红细胞,考虑血管内皮肿瘤。2013-10-14 19:26
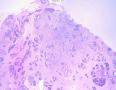
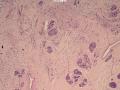
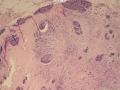
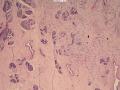
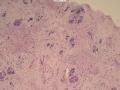
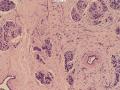
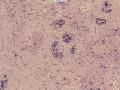
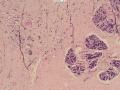
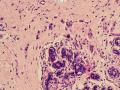
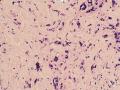
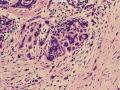
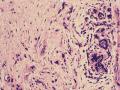
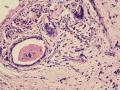
(左侧)乳腺组织,乳腺大部分区域呈小叶增生性腺病改变,部分区域乳腺小叶周边可见增生的单个或列兵样排列细胞索在小叶间或围小叶穿插围管状浸润生长;细胞学呈浆细胞样、蝌蚪样、不规则索性、部分呈小管样,胞核大而浓染,核浆比例大,异型性明显。
诊断:(左侧)乳腺恶性肿瘤,浸润性小叶癌可能性大,建议做免疫组化,进一步诊断。
鉴别诊断:1、特殊类型的导管癌或导管小叶来源。2、乳腺间叶肿瘤。
诊断:“左侧”乳腺:浸润性乳腺癌, 浸润性导管癌可能性大。
诊断依据:增生性小叶间及乳腺小叶内可见增生的单个、腺管样或条索样排列瘤细胞浸润生长。 瘤细胞异型性明显。并可见导管内癌成分。间质增生。
鉴别诊断:1、浸润性小叶癌,瘤细胞可见散在或“靶形”分布,但瘤细胞可见明显腺管样结构及小片状分布;可行免疫组化进一步鉴别。
2、乳腺恶性间叶肿瘤,肿瘤细胞散在分布,异形明显,部分呈梭形,但瘤细胞明显腺管样、小片样分布,考虑为上皮源性,可行免疫组化进一步鉴别。
免疫组化:P63、Calponin、ER、PR、C-erbB2、Ki-67、desmin、vimentin、EMA、S-100。
-
zyyzwangjin 离线
- 帖子:1220
- 粉蓝豆:262
- 经验:1873
- 注册时间:2013-08-19
- 加关注 | 发消息
-
本帖最后由 duoduo 于 2013-10-12 17:28:31 编辑
诊断:(左乳)血管源性肿瘤,考虑上皮样血管肉瘤
依据:低倍镜下,乳腺小叶结构存在,小叶外间质见内见异型细胞浸润,弥散分布,裂隙状及条索状,内衬上皮样细胞;高倍镜下,肿瘤细胞似形成大小不等的血管腔样结构,肿瘤细胞大,异型性明显,圆形或多边形,胞浆丰富嗜酸性,核大,核染色质粗糙,未见明显核仁(核仁常常很明显,这应该是上皮样血管内皮的一个特征,包括上皮样血管内皮细胞瘤),局部可见“三个一”,一个管腔,一个内皮细胞,一个红细胞。廖老师曾说过,一个腔内只有一个肿瘤细胞,是血管源性肿瘤的线索,免疫组化:CD31,CD34,第八因子,Fli-1等阳性可支持诊断。
鉴别诊断:1、上皮样血管内皮瘤:瘤细胞异型性不明显,介于良恶性血管肿瘤之间
2、乳腺浸润性小叶癌:瘤细胞黏附性差,列兵样或靶环样排列,ER/PR等阳性
3、乳腺浸润性小管癌:形态温和,管状,肌上皮缺乏,血管源性标记物阴性
4、转移性癌:结合病史及免疫组化结果
-
hanxiangchun 离线
- 帖子:68
- 粉蓝豆:709
- 经验:660
- 注册时间:2007-06-28
- 加关注 | 发消息
-
zhangmy99880 离线
- 帖子:144
- 粉蓝豆:64
- 经验:602
- 注册时间:2013-01-05
- 加关注 | 发消息
诊断:(左乳)血管源性肿瘤,考虑上皮样血管肉瘤
依据:低倍镜下,乳腺小叶结构存在,小叶外间质见内见异型细胞浸润,弥散分布,裂隙状及条索状,内衬上皮样细胞;高倍镜下,肿瘤细胞似形成大小不等的血管腔样结构,肿瘤细胞大,异型性明显,圆形或多边形,胞浆丰富嗜酸性,核大,核染色质粗糙,未见明显核仁(核仁常常很明显,这应该是上皮样血管内皮的一个特征,包括上皮样血管内皮细胞瘤),局部可见“三个一”,一个管腔,一个内皮细胞,一个红细胞。廖老师曾说过,一个腔内只有一个肿瘤细胞,是血管源性肿瘤的线索,免疫组化:CD31,CD34,第八因子,Fli-1等阳性可支持诊断。
鉴别诊断:1、上皮样血管内皮瘤:瘤细胞异型性不明显,介于良恶性血管肿瘤之间
2、乳腺浸润性小叶癌:瘤细胞黏附性差,列兵样或靶环样排列,ER/PR等阳性
3、乳腺浸润性小管癌:形态温和,管状,肌上皮缺乏,血管源性标记物阴性
4、转移性癌:结合病史及免疫组化结果

- 自己选择的路,爬也要爬完。
诊断:小管小叶癌,相当于小管癌样小管+线性或条索状小叶癌成分组合而成
低倍见很多小叶结构,小叶未见明确肿瘤样变(可有LCIS和或DCIS,不影响诊断),小叶结构之间可见很多索状和有微小腺腔和或有不易察觉腺腔的小管浸润生长,很像浸润性小叶癌,但小管样结构和小管癌不一样之处在于无明显成角,似乎开窗也太小了。免疫组化介于导管癌和小叶癌之间,主要是表达高分子量CK‘和E-cadherin。预后比小管癌差些,可有淋巴结转移。
原先认为这个是小叶癌的变异型,最近的免疫组化和其它研究证实这个病变仍是导管分化的肿瘤
The ductal phenotypic expression of the E-cadherin/catenin complex in tubulolobular carcinoma of the breast: an immunohistochemical and clinicopathologic study.
Source
Department of Pathology, University of Pittsburgh Medical Center, Pittsburgh, PA 15261, USA. espositonc@upmc.edu
Abstract
Tubulolobular carcinoma is a type of mammary carcinoma that displays an admixture of invasive tubules and lobular-like cells. Previous reports have shown it to share clinical similarities to lobular carcinoma, whereas more recent studies have shown it to be E-cadherin positive. The aim of the current study was to further explore the immunophenotype of tubulolobular carcinoma, and to document its natural behavior. Nineteen cases of tubulolobular carcinoma and 10 cases each of tubular and lobular carcinoma were retrieved for comparison analysis. Immunohistochemistry was performed with antibodies against estrogen receptor, progesterone receptor, HER2/neu, 34betaE12, E-cadherin, and the catenins. Twenty-five percent of patients with tubulolobular carcinoma presented with greater than stage I disease, compared to 0 and 60% of patients with tubular and lobular carcinoma, respectively. Two patients with tubulolobular carcinoma had tumor recurrence, one of whom also developed metastasis. The majority of all carcinomas were estrogen and progesterone receptor positive. E-cadherin displayed membranous staining in all tubular and tubulolobular carcinomas, and was negative in all lobular carcinomas. Half of each carcinoma subtype displayed granular cytoplasmic 34betaE12 immunoreactivity. alpha-Catenin exhibited partial or complete membranous staining in all tubulolobular and tubular carcinomas, and was negative in all lobular carcinomas. beta-Catenin displayed membranous staining in tubulolobular and tubular carcinomas, whereas all lobular carcinomas had coarse cytoplasmic immunoreactivity. p120 and gamma-catenin displayed membranous staining in 100% of tubulolobular and tubular carcinomas and cytoplasmic staining in 100% of lobular carcinomas. Tubulolobular carcinoma of the breast is thus a distinct type of mammary carcinoma that displays both tubular and lobular patterns histologically but displays the membranous E-cadherin/catenin complex characteristic of the ductal immunophenotype. Tubulolobular carcinoma appears to be more aggressive than tubular carcinoma, as 16% of patients had lymph node metastases, although all were alive at a mean follow-up of 40 months.
In conclusion, tubulolobular carcinoma of the breast is a distinct type of mammary carcinoma that displays both tubular and lobular patterns histologically but displays the membranous E-cadherin/catenin complex characteristic of the ductal immunophenotype. It may thus be better termed 'ductal carcinoma, tubulolobular subtype', or 'ductal carcinoma with a tubulolobular pattern'. Even in this small group of patients, tubulolobular carcinoma appears to be more aggressive than tubular carcinoma, as 16% of patients had lymph node metastases, although it carries an overall good prognosis, as all patients were alive at a mean follow-up time of 40 months