| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B1046Breast tubular leisons, MGA and differential diagnosis (cqz 2)
| 姓 名: | ××× | 性别: | F | 年龄: | 49 |
| 标本名称: | Breast excisional biopsy (乳腺切除活检) | ||||
| 简要病史: | |||||
| 肉眼检查: | |||||
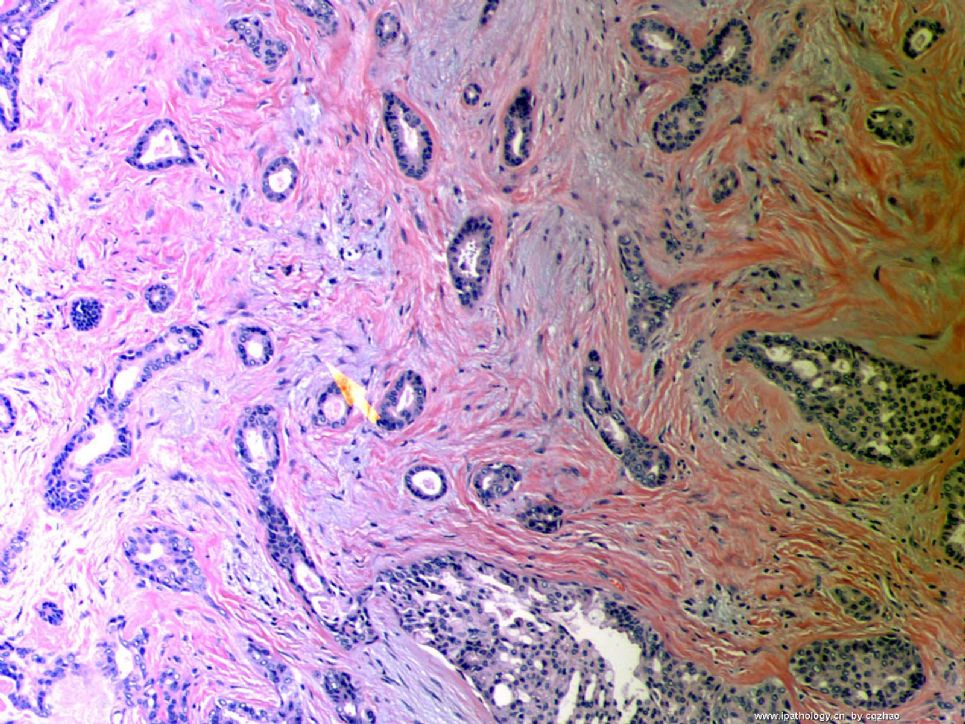
Microscopically it is a 0.8 cm lesion as photo.
Your diagnosis and differential diagnosis.
(镜下病变直径0.8cm,如图。请诊断和鉴别诊断)
名称:图1
描述:图1
-
本帖最后由 于 2010-05-16 23:38:00 编辑
相关帖子
- • 左乳肿物
- • 乳腺肿物一例
- • 腺病?癌?其他?(12楼常规,24楼免疫组化及会诊结果)
- • 左乳肿块,2X1.5cm,请会诊
- • 乳腺肿物
- • 求助:56岁女,左乳肿物,能排除小管癌吗?
- • 38岁乳腺(新加HE切片)
- • 乳腺包块。33岁
- • 乳腺肿块
- • 乳腺小管癌?
-
本帖最后由 于 2008-10-12 22:12:00 编辑
Looks like tubular carcinoma, a well differentiated invasive ductal carcinoma. It requires >75%(?) tubular formation in neoplastic glands. Lower right hand portion of the photo shows possible low grade DCIS. The stroma probably represents desmoplastic response to those tumor glands. I talk with uncertain tone "probable, possible, looks like" because a single photomicrograph is a very limited source for a significant diagnosis, i cannnot be very sure.
abin译:
像小管癌,属于一种分化好的浸润性导管癌。它要求肿瘤性腺体中小管结构>75%(译注,这个标准有争议,有人严格要求100%。WHO认为小管结构达90%作为诊断标准可能较为妥当)。
右下可能为低级别DCIS。间质可能是促结缔组织反应。
回22楼和26楼:
需要在微腺性腺病和浸润癌之间鉴别。腺腔小,较一致,腺体周围似有肌上皮混杂,支持微腺性腺病。但部分腺上皮异型性明显,关键是脂肪组织中有浸润。不能除外癌。必须做P63,CK5/6和SMA等肌上皮标记。
期待Dr. Zhao的讲解。。。。。。

- If you have great talents, industry will improve them; if you have but moderate abilities, industry will supply their deficiency. 如果你很有天赋,勤勉会使其更加完美;如果你能力一般,勤勉会补足其缺陷。
-
stevenshen 离线
- 帖子:343
- 粉蓝豆:2
- 经验:343
- 注册时间:2008-06-03
- 加关注 | 发消息
-
本帖最后由 于 2008-10-12 23:18:00 编辑
Florid small glandular proliferation with infiltration of stroma and fat = microglandular adenosis pattern; marked cytologic atypia including prominent nucleoli; stroma alteration more than that of benign microglandular adenosis. Morphologic diagnoses infiltrating ductal carcinoma with microglandular adenosis pattern or arising from microglandular adenosis. IHC stain with myoepithelial markers and collagen IV and S100 (as described by Dr. Zhao) will be help to confirm the diagnosis. Never seen such a case. Look forward to hearing about the final diagnosis. Thanks.
abin译:小腺体旺炽性增生,浸润间质和脂肪,这是微腺腺病的生长方式;有明显的细胞学非典型性,包括明显核仁;间质的改变也超出了良性微腺腺病的程度。
形态学诊断:呈微腺腺病结构的浸润性导管癌,或发生于微腺腺病的浸润性导管癌。
作肌上皮标记和S-100免疫组化以及胶原IV染色有助于确诊。从未见过这样的病例。期待最后诊断。
谢谢。
Thank all of you for reading the case and writing your diagnosis here. Most of you have the correct or almost right interpretation or differential diagnosis.
This is a microglandular adenosis (MGA) case. The main differential dx contain tubular carcinoma (TC) and other adenosis and its variants. The diagnosis is not very difficult based on the morphology if you see few cases already. Histologically, MGA consists small round glands with open lumens, distributed mostly randomly in a hypocellular dense collagenous or fatty stroma. The glands are lined by a single layer of (flat to) uniform cuboidal epithelial cells and completely invested by a basement membrane (TC with no BM). The Lumen contains PAS+ eosinophilic secretion. You should make the dx if you know these morphologic features well. Please compare the morphologic features of this case with that of my above TC cases.
IHC stains can help you. I summaried a brief table below.
|
IHC Antigens |
MGA |
Tubular Ca |
Other adenosis |
|
cytokeratin |
+ |
+ |
+ |
|
S-100 |
+ |
- |
- |
|
ER/PR |
- |
+ |
+ |
|
Myoepithelial markers |
- |
- |
+ |
|
Basement membrane* |
+ |
- |
+ |
*Collagen IV, laminin, reticulin
Very glad to see that some of you have noted the presense of cellular atypia. Focal areas (last 4 photos) show varied gland configuration or irregularity of the glands. Some glans lack secretion and the lumens are obscured by celluar prolifearion. The cells demonstrate mild-moderate nuclear pleomorphism and prominent nucleoli. So the case was dianosed MGA with focal atypia or atypical MGA (AMGA).
MGA is an extremely rare benign breast lesion. 108 cases were originally diagnosed as MGA in M.D Anderson Cancer Center (one of the largest cancer center in the US) from 1983 to 2007. Of the 108 cases, 65 cases had available materials for review. 11 of 65 cases qualified to have MGA component. Myoepithelial layers was detected in other 54 cases and they were reclassified as adenosis. Now you know the true MGA case is rare and rare. The hospital I currently work is one of the largest gyn and breast center in the US. Only one MGA case was diagnosed in the past three years. The current case is the one when I worked at AFIP.
The lesion is spectrum of glandular proliferations ranging from uncomplicated MGA to MGA with atypia to MGA associated carcinoma (MGACA). For difficult cases IHC stains for Ki67 and p53 can be helpful.
Ki67: MGA <3%; AMGA 5-10; MGACA>30%
p53: MGA<3%; AMGA 5-10%; MGACA>30%
I think the percentage is just for reference and histologic features are the key for diagnosis.
Useful reference:
1. Khalifeh IM etal. Clinical, histopathologic, and immunihistochemical features .... Am J Surg pathol 2008;32:544-552.
2. Koenig C et al. Carcinoma arising in microglandular adenosis: an immunohistochemical analysis....Int J Surg Pathol 2000;8:303-315.
Just came back from China and feel tired. I put the case here three weeks ago and have to complete it . Sorry for the delay.
Thanks,
cqz
-
谢谢各位老师的讲解,很有启发。
第22楼的结构特点和生长方式:无小叶结构,浸润脂肪,小腺体或小管增生,腔圆有红染分泌物,胞浆淡染有空泡。间质有较多粗胶原。
主要考虑以下几个鉴别诊断:微腺腺病MGA或微腺体增生MGH,小管癌TC或高分化的浸润性导管癌,以及乳头部腺瘤。
形态学特点首先考虑MGA。没有促结缔组织反应,基本排除TC或浸润性导管癌。它也不像乳头部腺瘤。
需要免疫组化(肌上皮标记如SMA和p63等,ER,PR,CK5,S-100)及胶原IV等帮助诊断。
另外请Dr.Zhao讲解一下与腺泡细胞癌的鉴别,谢谢。

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
| 以下是引用abin在2008-10-13的发言: 谢谢各位老师的讲解,很有启发。 |
| 以下是引用cqzhao在2008-10-28 12:29:00的发言并翻译:
谢谢大家阅读病例并写出了诊断。大多数都给出了正确的判断和鉴别诊断。 本例为微腺腺病(MGA)。主要鉴别:小管癌(TC)和其它腺病及变型。如果见过几例,形态学诊断并不太难。组织学:MGA由小而圆的腺体组成,腺腔开放,大多数随机分布于少细胞的致密胶原化间质或脂肪中。腺体衬覆一致的单层扁平或立方上皮,有完整的基底膜包绕(TC无基底膜)。腔内含PAS+嗜酸性分泌物。如果知道这些形态学特征,应该能够诊断。请与我提供的上述TC病例相比较。 免疫组化可能有帮助,总结如下:
*Collagen IV, laminin, reticulin
很高兴看到有人注意到存在细胞学非典型性。灶性区域(最后4图)显示不规则的腺体结构。一些腺体无分泌物,细胞增生使腺腔结构不清。细胞呈轻-中度核多形性,有明显核仁。因此本例诊断为MGA伴局灶非典型增生(非典型性MGA)。 MGA是极其罕见的乳腺良性病变。1983-2007,M.D Anderson Cancer Center(美国最大的癌症中心)原诊断了108例MGA。其中65例有可回顾资料。11/65例有MGA成分,其余54例检出肌上皮层,重新归类为腺病。至此你会明白MGA确实是少而又少。我目前工作的医院是美国最大的妇科和乳腺中心,过去三年中仅诊断一例MGA。本例是我在AFIP工作时遇到的。 腺体增生的病变谱包括无特殊病变的MGA-MGA伴非典型性-MGA伴癌(MGACA)。困难病例,Ki67和p53免疫染色可能有帮助。 Ki67: MGA <3%; AMGA 5-10; MGACA>30% p53: MGA<3%; AMGA 5-10%; MGACA>30% 我认为上述比例仅供参考,组织学特征才是诊断的关键。 一些有用的参考文献: 1. Khalifeh IM etal. Clinical, histopathologic, and immunihistochemical features .... Am J Surg pathol 2008;32:544-552. 2. Koenig C et al. Carcinoma arising in microglandular adenosis: an immunohistochemical analysis....Int J Surg Pathol 2000;8:303-315. 我刚从国内回来,感觉累。三周之前我提供了病例现在必须完成。抱歉耽搁了。 谢谢。 cqz |

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。