| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
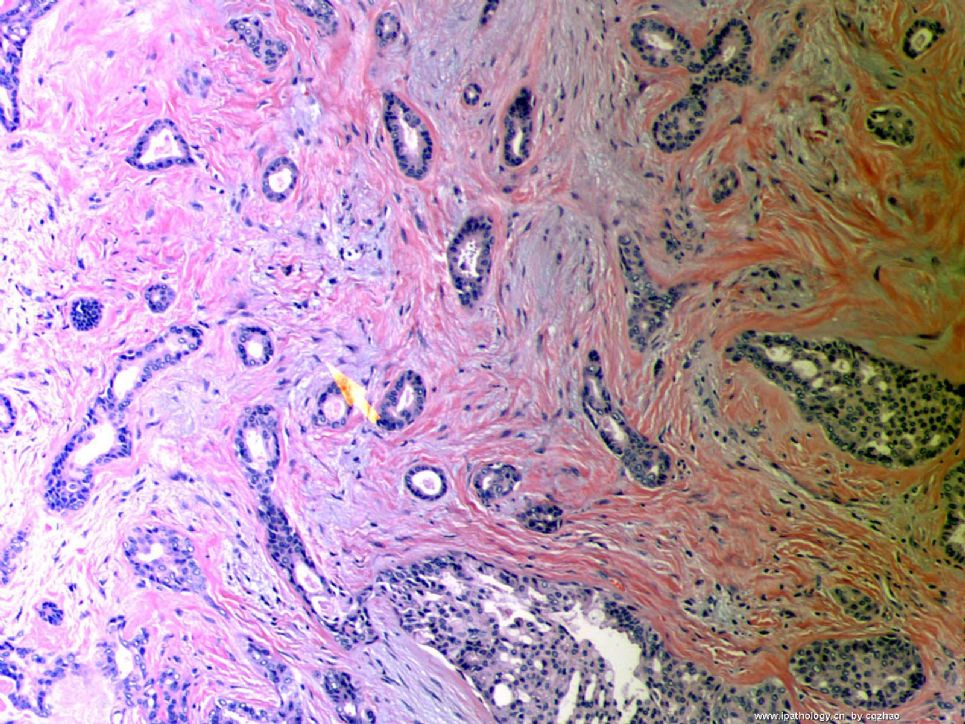
- B1046Breast tubular leisons, MGA and differential diagnosis (cqz 2)
| 姓 名: | ××× | 性别: | F | 年龄: | 49 |
| 标本名称: | Breast excisional biopsy (乳腺切除活检) | ||||
| 简要病史: | |||||
| 肉眼检查: | |||||
Microscopically it is a 0.8 cm lesion as photo.
Your diagnosis and differential diagnosis.
(镜下病变直径0.8cm,如图。请诊断和鉴别诊断)
名称:图1
描述:图1
-
本帖最后由 于 2010-05-16 23:38:00 编辑
相关帖子
- • 左乳肿物
- • 乳腺肿物一例
- • 腺病?癌?其他?(12楼常规,24楼免疫组化及会诊结果)
- • 左乳肿块,2X1.5cm,请会诊
- • 乳腺肿物
- • 求助:56岁女,左乳肿物,能排除小管癌吗?
- • 38岁乳腺(新加HE切片)
- • 乳腺包块。33岁
- • 乳腺肿块
- • 乳腺小管癌?
-
本帖最后由 于 2008-10-12 22:56:00 编辑
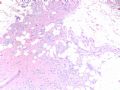
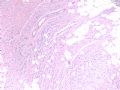
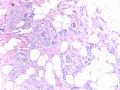
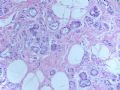
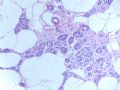
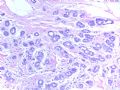
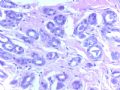
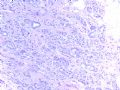
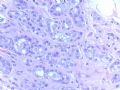
This is a typical tubular ca.
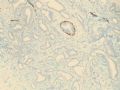
Fig 1 20x H&E
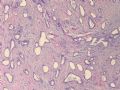
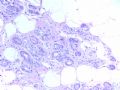
Fig 2.10x SMMHC stain
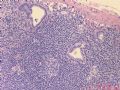
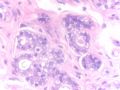
Fig 3. 10x P63 stain
Fig 4. 10x K67, very low proliferative index
Tubular carcinoma (TC)is composed of small angular, oval, and tubular glands in the fibrotic background. Generally it is easy to make diagnosis. However it may be confused with sclerosing adenosis and microglandular hyperplasia (MGH).
MGH glands also lack myoepithelial cells, but basement memberane stain (for example college IV) and S-100 stain are positive. These two stains are negative for TC. Microscopically, MGA is an infiltrative proliferation of small glands in fibrous or fatty stroma. MGA is composed of small uniform and regular glnads containing eosinophilic secretion.
It is not difficult to tell the difference between TC and sclerosing adenosis (SA). However, occasionally SA can be a mimic of TC. When the dx is unsure, stains of myoepithelial markers can be very useful like my first case.
Thank for reading
njwbhuang译:
第15楼提供的四张图,如下。这才是典型的小管癌。
小管癌是由一些小的有角的、卵圆形和小管状腺体组成,包埋于纤维性间质背景中。一般情况下较易诊断,然而它可与硬化性腺病和微腺体增生(MGH)混淆。
MGH中腺体也无肌上皮细胞,但基底膜染色(Ⅳ型胶原)和S-100蛋白染色阳性,而小管癌中则染色阴性。镜下,微腺性腺病(MGA)是小的腺体浸润于纤维或脂肪间质内,腺体较小,大小较一致,腺腔内含有嗜酸性分泌物。
小管癌与硬化性腺病(SA)的鉴别并不困难。然而,偶尔SA可能误诊为小管癌。当诊断不确定时,正如本例一样,肌上皮标记物有助于诊断。
谢谢阅读。
-
本帖最后由 于 2008-10-12 22:22:00 编辑
To the Second floor:
There are no consensus concerning the proportion of tubular structures to establish the dx of TC. Some suggest the different cut-off points 75%, 90%, 100%. New WHO mentioned that for pragmatic reason, a 90% purity requirement offers a practical solution. For my daily practie, I use 100% as cut off point. Otherwise I call invasive ductal carcinoma with (focal) tubular feature. Few percentage of high grade carcinoma may cause poor prognosis.
In the right side, few ducts show UDH and no ADH present.
abin译:
关于诊断所需的小管结构的比例,尚未一致,有三种观点75%,90%和100%。新WHO提出90%作为实用标准。
我在日常工作中采用100%的诊断标准。否则我称为浸润性导管癌伴(局灶)小管癌特征。很少比例的高级别癌也可能预后差。
切片右侧一些导管为UDH,没有ADH。
-
本帖最后由 于 2008-10-12 22:34:00 编辑
Just released another tubular carcinoma and share with people who love breast pathology.
Slide Key:
H&E 10x
Lymph node 20x
Lymph node 20x ER stain
This is a very low grade tumor of 0.7 cm with Nottingham grade 1. However axillary SNB shows 1 mm micrometastases.
Definition:
Isolated tumor cell: single cells or small clusters of cell not greater than 0.2 mm. (孤立的肿瘤细胞:单个细胞或小簇,不超过0.2mm)
Micrometastases: >0.2 mm to <2 mm. pN1mi (微小转移:>0.2mm 但<2 mm)
Thanks
-
stevenshen 离线
- 帖子:343
- 粉蓝豆:2
- 经验:343
- 注册时间:2008-06-03
- 加关注 | 发消息
-
本帖最后由 于 2008-10-12 22:41:00 编辑
Thanks very much for this very challenging case and great discussion. I have to say that I would also make the diagnosis of invasive tubular carcinoma as well by looking at the first picture. It appears to have all the features that we use for a tubular carcinoma. I am interested to know why Dr. Zhao even consider to do the immunostain in the first place. Can you please share with us your diagnostic process and experience. What morphologic features that prompt you to order an IHC? If I don't do the stain, I would make a wrong diagnosis. It is true that tubular carcinoma is one of the many common pitfalls in breast pathology. Thanks again.
abin译:
非常感谢提供如此具有挑战性的病例,并有极好的讨论。我一开始也把第一张图诊断为浸润性小管癌了。它似乎具有我们用于诊断小管癌的所有特征。我很想知道,Dr. Zhao为什么第一步会想到做免疫组化。能否请教诊断过程和经验?什么形态特征促使您作IHC?我如果不作IHC,可能会误诊。确实,小管癌是乳腺病理诊断中的许多常见陷阱之一。再次感谢。
-
本帖最后由 于 2008-10-12 23:07:00 编辑
Send you a rare breast lesion case.
Slide keys
Fig 1-3. 4x
Fig 4. 10x
Fig 5-7. 20x
Fig 8. 40x
Fig 9. 20x
Fig 10. 40x
Fig 11. 20x
Fig 12. 60x
You will not see this kind case often even if you are breast pathologists. Hope whoever see the photos write down your dx and short discussion if you like to. Interested to know your dx. I assume that dx is not difficult for you in this website. Here is free and you can say what you want to. You will not have any responsbility. Just think it is your patient and how you will deal with the case.
I will come back three weeks later and have a short discussion with ones who are interested in this case.
Thanks,
cqz
abin译:这一例即使是乳腺病理专科医生,也不常见。希望看过的朋友写下诊断和简单讨论。很想知道你们的诊断。我猜这对你们网站上的人来说不难。这里是自由讨论,可以发表你的任何观点。不需要负责。只是把它作为你的患者,你将如何一日处理这一病例。
我会在三周后回来,与喜欢这一例的朋友作简短讨论。
谢谢。
| 以下是引用cqzhao在2008-10-4 1:27:00的发言:
Send you a rare breast lesion case. Slide keys Fig 1-3. 4x Fig 4. 10x Fig 5-7. 20x Fig 8. 40x Fig 9. 20x Fig 10. 40x Fig 11. 20x Fig 12. 60x You will not see this kind case often even if you are breast pathologists. Hope whoever see the photos write down your dx and short discussion if you like to. Interested to know your dx. I assume that dx is not difficult for you in this website. Here is free and you can say what you want to. You will not have any responsbility. Just think it is your patient and how you will deal with the case. I will come back three weeks later and have a short discussion with ones who are interested in this case. Thanks, cqz |

朱正龙
| 以下是引用cqzhao在2008-10-2 17:53:00的发言:
This is a typical tubular ca. Fig 1 20x H&E Fig 2.10x SMMHC stain Fig 3. 10x P63 stain Fig 4. 10x K67, very low proliferative index Tubular carcinoma (TC)is composed of small angular, oval, and tubular glands in the fibrotic background. Generally it is easy to make diagnosis. However it may be confused with sclerosing adenosis and microglandular hyperplasia (MGH). MGH glands also lack myoepithelial cells, but basement memberane stain (for example college IV) and S-100 stain are positive. These two stains are negative for TC. Microscopically, MGA is an infiltrative proliferation of small glands in fibrous or fatty stroma. MGA is composed of small uniform and regular glnads containing eosinophilic secretion. It is not difficult to tell the difference between TC and sclerosing adenosis (SA). However, occasionally SA can be a mimic of TC. When the dx is unsure, stains of myoepithelial markers can be very useful like my first case. Thank for reading
|
译文:这是典型的小管癌。
小管癌是由一些小的有角的、卵圆形和小管状腺体组成,包埋于纤维性间质背景中。一般情况下较易诊断,然而它可与硬化性腺病和微腺体增生(MGH)混淆。
MGH中腺体也无肌上皮细胞,但基底膜染色(Ⅳ型胶原)和S-100蛋白染色阳性,而小管癌中则染色阴性。镜下,微腺性腺病(MGA)是小的腺体浸润于纤维或脂肪间质内,腺体较小,大小较一致,腺腔内含有嗜酸性分泌物。
小管癌与硬化性腺病(SA)的鉴别并不困难。然而,偶尔SA可能误诊为小管癌。当诊断不确定时,正如本例一样,肌上皮标记物有助于诊断。
谢谢阅读。
回22楼和26楼:
需要在微腺性腺病和浸润癌之间鉴别。腺腔小,较一致,腺体周围似有肌上皮混杂,支持微腺性腺病。但部分腺上皮异型性明显,关键是脂肪组织中有浸润。不能除外癌。必须做P63,CK5/6和SMA等肌上皮标记。
期待Dr. Zhao的讲解。。。。。。

- If you have great talents, industry will improve them; if you have but moderate abilities, industry will supply their deficiency. 如果你很有天赋,勤勉会使其更加完美;如果你能力一般,勤勉会补足其缺陷。
-
stevenshen 离线
- 帖子:343
- 粉蓝豆:2
- 经验:343
- 注册时间:2008-06-03
- 加关注 | 发消息
-
本帖最后由 于 2008-10-12 23:18:00 编辑
Florid small glandular proliferation with infiltration of stroma and fat = microglandular adenosis pattern; marked cytologic atypia including prominent nucleoli; stroma alteration more than that of benign microglandular adenosis. Morphologic diagnoses infiltrating ductal carcinoma with microglandular adenosis pattern or arising from microglandular adenosis. IHC stain with myoepithelial markers and collagen IV and S100 (as described by Dr. Zhao) will be help to confirm the diagnosis. Never seen such a case. Look forward to hearing about the final diagnosis. Thanks.
abin译:小腺体旺炽性增生,浸润间质和脂肪,这是微腺腺病的生长方式;有明显的细胞学非典型性,包括明显核仁;间质的改变也超出了良性微腺腺病的程度。
形态学诊断:呈微腺腺病结构的浸润性导管癌,或发生于微腺腺病的浸润性导管癌。
作肌上皮标记和S-100免疫组化以及胶原IV染色有助于确诊。从未见过这样的病例。期待最后诊断。
谢谢。
| 以下是引用abin在2008-10-13的发言: 谢谢各位老师的讲解,很有启发。 |