| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B1046Breast tubular leisons, MGA and differential diagnosis (cqz 2)
| 姓 名: | ××× | 性别: | F | 年龄: | 49 |
| 标本名称: | Breast excisional biopsy (乳腺切除活检) | ||||
| 简要病史: | |||||
| 肉眼检查: | |||||
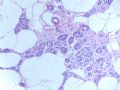
Microscopically it is a 0.8 cm lesion as photo.
Your diagnosis and differential diagnosis.
(镜下病变直径0.8cm,如图。请诊断和鉴别诊断)
名称:图1
描述:图1
-
本帖最后由 于 2010-05-16 23:38:00 编辑
相关帖子
- • 左乳肿物
- • 乳腺肿物一例
- • 腺病?癌?其他?(12楼常规,24楼免疫组化及会诊结果)
- • 左乳肿块,2X1.5cm,请会诊
- • 乳腺肿物
- • 求助:56岁女,左乳肿物,能排除小管癌吗?
- • 38岁乳腺(新加HE切片)
- • 乳腺包块。33岁
- • 乳腺肿块
- • 乳腺小管癌?
-
本帖最后由 于 2010-09-02 12:20:00 编辑
Am J Surg Pathol. 2009 Apr;33(4):496-504.
Molecular evidence for progression of microglandular adenosis (MGA) to invasive carcinoma.
Shin SJ, Simpson PT, Da Silva L, Jayanthan J, Reid L, Lakhani SR, Rosen PP.
Department of Pathology and Laboratory Medicine, New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY 10065, USA. sjshin@med.cornell.edu
Abstract
Microglandular adenosis (MGA) is an uncommon, benign breast lesion that is characterized by a proliferation of small uniform, round glands lined by a single layer of epithelial cells around open lumina with haphazard infiltrative growth in fibrous and fatty breast tissue. Although MGA usually has an indolent course, there is morphologic evidence that MGA can be a precursor for the development of intraductal and invasive ductal carcinoma. To investigate the possibility of such a transition, we studied 17 cases of MGA or atypical MGA some of which had given rise to carcinoma in situ (CIS) and/or invasive ductal carcinoma using the reticulin stain, immunohistochemistry (S-100, p63, Ki-67, and p53), and a molecular approach involving microdissection and high-resolution comparative genomic hybridization and MYC chromogenic in situ hybridization. MGA and carcinomas arising from MGA were typically negative for p63 and positive for S-100 and Ki-67 and occasionally positive for p53. High-resolution comparative genomic hybridization identified recurrent gains and losses in MGA (2q+, 5q-, 8q+, and 14q-) and atypical MGA (1q+, 5q-, 8q+, 14q-, and 15q-). Some examples of MGA and carcinomas arising from MGA harbored few gross chromosomal abnormalities whereas others had considerable genetic instability with widespread aberrations affecting numerous chromosomal arms. Such widespread genetic changes, together with recurrent loss of 5q and gain of 8q were reminiscent of those reported specifically for basal-like, estrogen receptor-negative, and BRCA1-associated breast tumors. Concordant genetic alterations were identified between MGA, atypical MGA, and higher risk lesions (CIS and invasive ductal carcinoma) and in some cases there was an accumulation of genetic alterations as cases "progressed" from MGA to atypical MGA, CIS, and invasive ductal carcinoma. The molecular data suggests that MGA, atypical MGA, and carcinoma arising in MGA in a single case were clonally related. This result implicates MGA as a nonobligate precursor for the development of intraductal and invasive ductal carcinoma.
-
本帖最后由 于 2008-12-24 20:14:00 编辑
| 以下是引用天山望月在2008-12-15 21:39:00的发言:
个人感觉: 仅从细胞图片看,有时不易诊断小管癌,需与导管内乳头状瘤或癌、DCIS、低级别的浸润性导管癌、淋巴瘤等鉴别。组织切片和免疫组化有助诊断。 不知对否?请赵老师点评!谢谢! |
You are right.
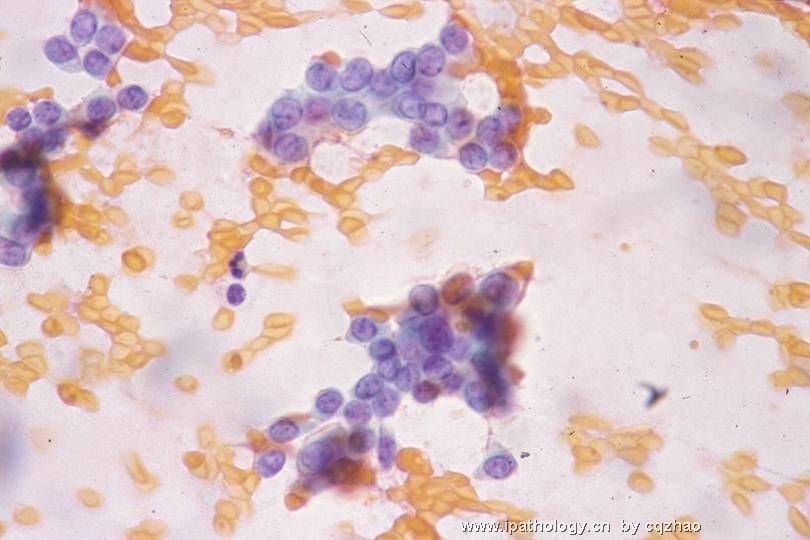
Like other low grade ca, TC is very difficult to make dx in FNA cytology, especially from the benign lesions. It is important you can call atypia and require core biopsy. Cell block may be helpful, but not IHC.
-
本帖最后由 于 2008-12-15 21:31:00 编辑
You work so hard and should get some awards.
你如此勤奋,应该获奖。
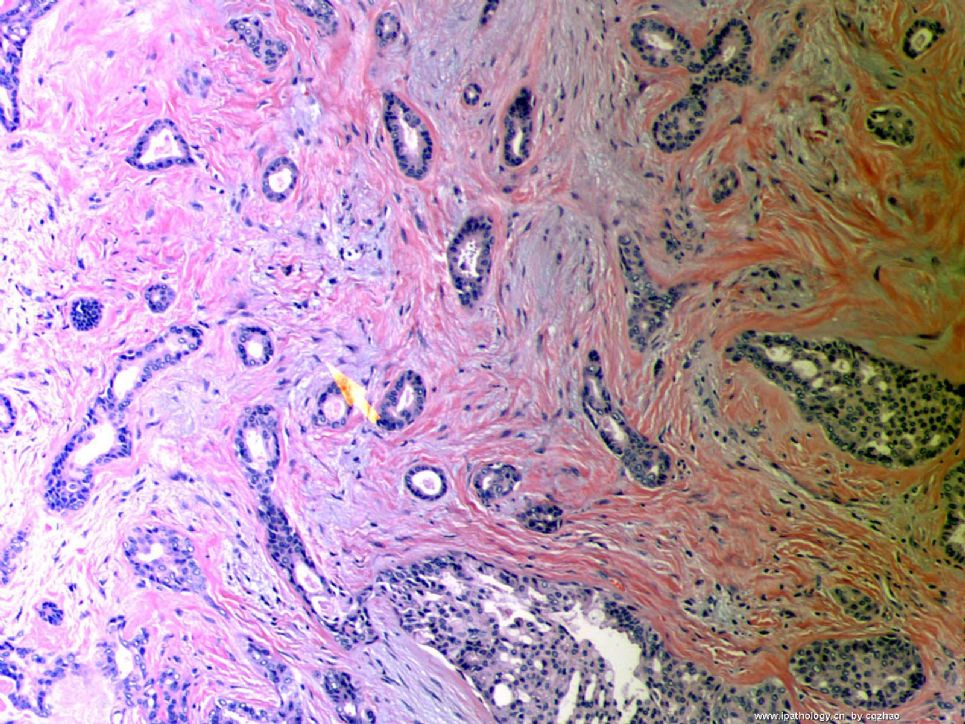
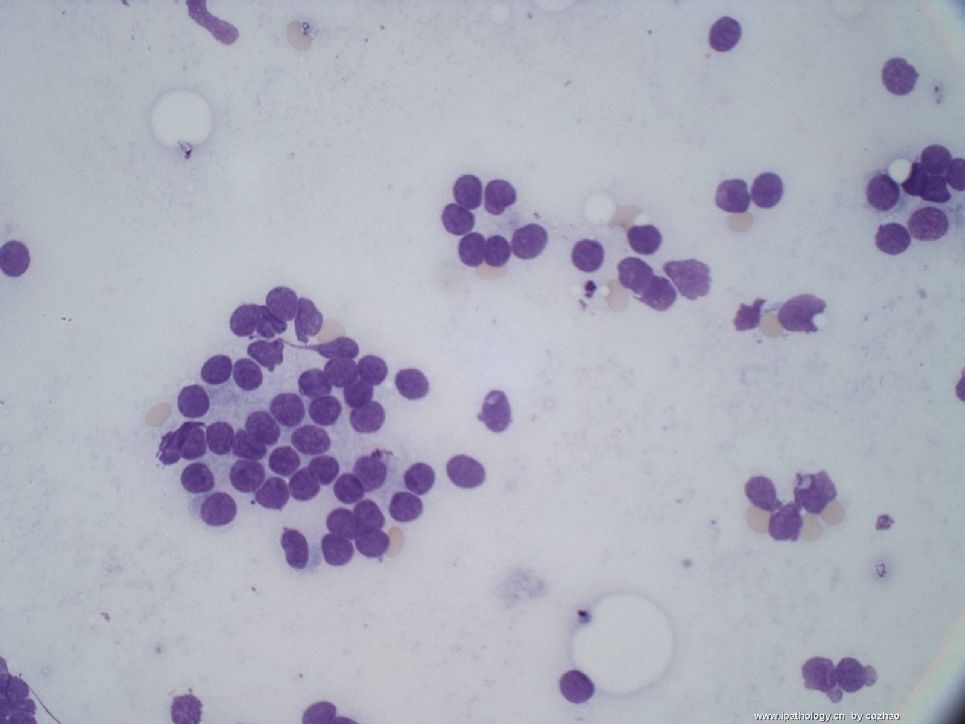
Fig 1 and 2 are two classic pathology or cytopathology board photos. Whe you see them during a test, just pick the answer tubular ca immediately and go to the next question.
图1和图2是两个经典的病理学或细胞病理学样本图片。考试时看到它们时,只要立即选择小管癌即可,直接跳到下一题。
Fig 3-6 are cases of tubular ca FNA confirmed by biopsy. In true practice, you must be cautious to call tubular carcinoma for these cases. It is better to call atypical, favor... et al. Ask to do the biopsy. It is very difficult to diagnose tubular ca by FNA cytology. Find a good FNA book to read the cytopathologic features of these lesions.
图3-6是小管癌的FNA表现,由活检证实。在实际工作中,必须非常小心诊断小管癌。最好称为“不典型细胞,倾向……”等等,然后要求活检。FNA细胞学诊断小管癌非常困难。找一本FNA好书,阅读一下这些病变的细胞病理学特征。
Now you have all my photos and no more to teach you.
现在我已经全部奉献出有关小管癌的所有图片,没有更多内容用来教学了。
(abin译)

名称:图1
描述:图1

名称:图2
描述:图2

名称:图3
描述:图3

名称:图4
描述:图4
名称:图5
描述:图5
名称:图6
描述:图6
Made some questions for our follow teaching. Choose three and put here.
You are wellcome to write your answers. Please pay attention: One question may have more than one answers
1. Which is (are) not true about tubular carcinoma cytology
A. Hypo-cellular specimen
B. Angulated, pointed, open rigid tubules
C. Little or no cellular atypia
D. Bipolar naked nuclei usually not present
E. Cohesive clusters of cells
F. The sensitivity for the dx is lower for FNA, 50%
F. All are true.
2. Which is (are) not true about tubular carcinoma
A. Have excellent prognosis
B. Majority (60-70%) now present as nonpalpable mammographic abnormality
C. Pure TC: >90% of the tumor should exhibit tubules
D. Usually ER/PR+, Her2-
E. Less than 50% cases have associated with low grade DCIS
F. All are true.
3. Which markers are useful to distinguish tubular carcinoma from microglandular hyperplasia
A. Myoepithelial markers
B. Collagen IV
C. S-100
D. CK7
F. ER
Thank all of you for reading the case and writing your diagnosis here. Most of you have the correct or almost right interpretation or differential diagnosis.
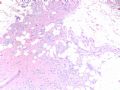
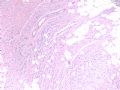
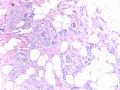
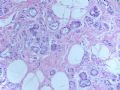
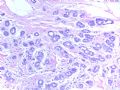
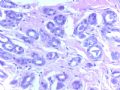
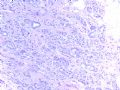
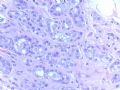
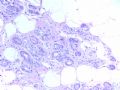
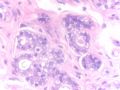
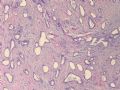
This is a microglandular adenosis (MGA) case. The main differential dx contain tubular carcinoma (TC) and other adenosis and its variants. The diagnosis is not very difficult based on the morphology if you see few cases already. Histologically, MGA consists small round glands with open lumens, distributed mostly randomly in a hypocellular dense collagenous or fatty stroma. The glands are lined by a single layer of (flat to) uniform cuboidal epithelial cells and completely invested by a basement membrane (TC with no BM). The Lumen contains PAS+ eosinophilic secretion. You should make the dx if you know these morphologic features well. Please compare the morphologic features of this case with that of my above TC cases.
IHC stains can help you. I summaried a brief table below.
|
IHC Antigens |
MGA |
Tubular Ca |
Other adenosis |
|
cytokeratin |
+ |
+ |
+ |
|
S-100 |
+ |
- |
- |
|
ER/PR |
- |
+ |
+ |
|
Myoepithelial markers |
- |
- |
+ |
|
Basement membrane* |
+ |
- |
+ |
*Collagen IV, laminin, reticulin
Very glad to see that some of you have noted the presense of cellular atypia. Focal areas (last 4 photos) show varied gland configuration or irregularity of the glands. Some glans lack secretion and the lumens are obscured by celluar prolifearion. The cells demonstrate mild-moderate nuclear pleomorphism and prominent nucleoli. So the case was dianosed MGA with focal atypia or atypical MGA (AMGA).
MGA is an extremely rare benign breast lesion. 108 cases were originally diagnosed as MGA in M.D Anderson Cancer Center (one of the largest cancer center in the US) from 1983 to 2007. Of the 108 cases, 65 cases had available materials for review. 11 of 65 cases qualified to have MGA component. Myoepithelial layers was detected in other 54 cases and they were reclassified as adenosis. Now you know the true MGA case is rare and rare. The hospital I currently work is one of the largest gyn and breast center in the US. Only one MGA case was diagnosed in the past three years. The current case is the one when I worked at AFIP.
The lesion is spectrum of glandular proliferations ranging from uncomplicated MGA to MGA with atypia to MGA associated carcinoma (MGACA). For difficult cases IHC stains for Ki67 and p53 can be helpful.
Ki67: MGA <3%; AMGA 5-10; MGACA>30%
p53: MGA<3%; AMGA 5-10%; MGACA>30%
I think the percentage is just for reference and histologic features are the key for diagnosis.
Useful reference:
1. Khalifeh IM etal. Clinical, histopathologic, and immunihistochemical features .... Am J Surg pathol 2008;32:544-552.
2. Koenig C et al. Carcinoma arising in microglandular adenosis: an immunohistochemical analysis....Int J Surg Pathol 2000;8:303-315.
Just came back from China and feel tired. I put the case here three weeks ago and have to complete it . Sorry for the delay.
Thanks,
cqz
-
本帖最后由 于 2008-10-12 23:07:00 编辑
Send you a rare breast lesion case.
Slide keys
Fig 1-3. 4x
Fig 4. 10x
Fig 5-7. 20x
Fig 8. 40x
Fig 9. 20x
Fig 10. 40x
Fig 11. 20x
Fig 12. 60x
You will not see this kind case often even if you are breast pathologists. Hope whoever see the photos write down your dx and short discussion if you like to. Interested to know your dx. I assume that dx is not difficult for you in this website. Here is free and you can say what you want to. You will not have any responsbility. Just think it is your patient and how you will deal with the case.
I will come back three weeks later and have a short discussion with ones who are interested in this case.
Thanks,
cqz
abin译:这一例即使是乳腺病理专科医生,也不常见。希望看过的朋友写下诊断和简单讨论。很想知道你们的诊断。我猜这对你们网站上的人来说不难。这里是自由讨论,可以发表你的任何观点。不需要负责。只是把它作为你的患者,你将如何一日处理这一病例。
我会在三周后回来,与喜欢这一例的朋友作简短讨论。
谢谢。
-
本帖最后由 于 2008-10-12 22:34:00 编辑
Just released another tubular carcinoma and share with people who love breast pathology.
Slide Key:
H&E 10x
Lymph node 20x
Lymph node 20x ER stain
This is a very low grade tumor of 0.7 cm with Nottingham grade 1. However axillary SNB shows 1 mm micrometastases.
Definition:
Isolated tumor cell: single cells or small clusters of cell not greater than 0.2 mm. (孤立的肿瘤细胞:单个细胞或小簇,不超过0.2mm)
Micrometastases: >0.2 mm to <2 mm. pN1mi (微小转移:>0.2mm 但<2 mm)
Thanks
-
本帖最后由 于 2008-10-12 22:22:00 编辑
To the Second floor:
There are no consensus concerning the proportion of tubular structures to establish the dx of TC. Some suggest the different cut-off points 75%, 90%, 100%. New WHO mentioned that for pragmatic reason, a 90% purity requirement offers a practical solution. For my daily practie, I use 100% as cut off point. Otherwise I call invasive ductal carcinoma with (focal) tubular feature. Few percentage of high grade carcinoma may cause poor prognosis.
In the right side, few ducts show UDH and no ADH present.
abin译:
关于诊断所需的小管结构的比例,尚未一致,有三种观点75%,90%和100%。新WHO提出90%作为实用标准。
我在日常工作中采用100%的诊断标准。否则我称为浸润性导管癌伴(局灶)小管癌特征。很少比例的高级别癌也可能预后差。
切片右侧一些导管为UDH,没有ADH。
-
本帖最后由 于 2008-10-12 22:54:00 编辑
Lower Power: Generally, typical tubular carcinomas show angular and irregular glands with open lumens in desmoplastic stroma, such as my previous two cases. Sclerosing adenosis can also exhibit varying numbers of round, oval, or angular glands with open lumen. However the findings of open lumen often are not obvious.
High power: The nuclei of TC are often round and uniform, but not for SA.
Please remember that breast bx, skin malanoma, and pap test are the top three for lawsuit. Unfortunately I am a gyn/breast apthologist and need to deal with the two areas of the three every day. Anyway, You have to think over before you release any malignant case.
Hope it can help. Thnaks.
abin译:小管癌和硬化性腺病的鉴别要点
低倍:成角和不规则的腺体,管腔开放,促结缔组织增生性间质,正如我已经上传的两个病例。硬化性腺病(SA)也表现为不同数量的圆形或卵圆形或成角腺体,管腔开放。然而,开放的管腔通常不明显。
高倍:小管癌的核通常圆而一致,而SA不是这样。
请记住,乳腺活检,皮肤恶黑,和宫颈细胞学引起的诉讼最多。不幸得很,我从事妇科/乳腺病理,每天都需要处理三者中的两个。总之,发出恶性诊断之前,一定要再三推敲。
希望有帮助。谢谢。
-
本帖最后由 于 2008-10-12 22:56:00 编辑
This is a typical tubular ca.
Fig 1 20x H&E
Fig 2.10x SMMHC stain
Fig 3. 10x P63 stain
Fig 4. 10x K67, very low proliferative index
Tubular carcinoma (TC)is composed of small angular, oval, and tubular glands in the fibrotic background. Generally it is easy to make diagnosis. However it may be confused with sclerosing adenosis and microglandular hyperplasia (MGH).
MGH glands also lack myoepithelial cells, but basement memberane stain (for example college IV) and S-100 stain are positive. These two stains are negative for TC. Microscopically, MGA is an infiltrative proliferation of small glands in fibrous or fatty stroma. MGA is composed of small uniform and regular glnads containing eosinophilic secretion.
It is not difficult to tell the difference between TC and sclerosing adenosis (SA). However, occasionally SA can be a mimic of TC. When the dx is unsure, stains of myoepithelial markers can be very useful like my first case.
Thank for reading
njwbhuang译:
第15楼提供的四张图,如下。这才是典型的小管癌。
小管癌是由一些小的有角的、卵圆形和小管状腺体组成,包埋于纤维性间质背景中。一般情况下较易诊断,然而它可与硬化性腺病和微腺体增生(MGH)混淆。
MGH中腺体也无肌上皮细胞,但基底膜染色(Ⅳ型胶原)和S-100蛋白染色阳性,而小管癌中则染色阴性。镜下,微腺性腺病(MGA)是小的腺体浸润于纤维或脂肪间质内,腺体较小,大小较一致,腺腔内含有嗜酸性分泌物。
小管癌与硬化性腺病(SA)的鉴别并不困难。然而,偶尔SA可能误诊为小管癌。当诊断不确定时,正如本例一样,肌上皮标记物有助于诊断。
谢谢阅读。
 ,但愿都对啊,对了老师颁奖昂!
,但愿都对啊,对了老师颁奖昂!