| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B267056 y female breast mass, breast core bx (cqz-32 4-22-2010)
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
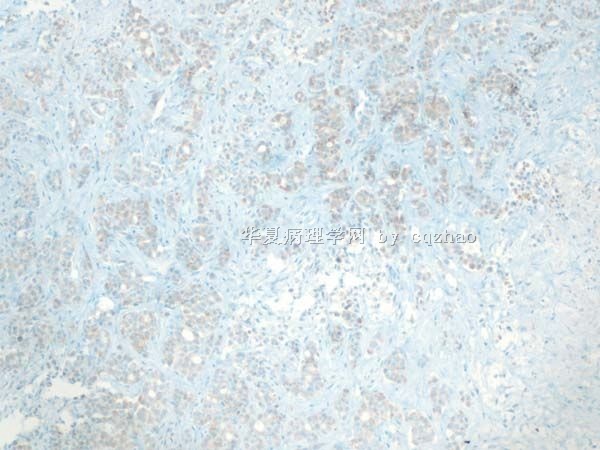
F1 100x
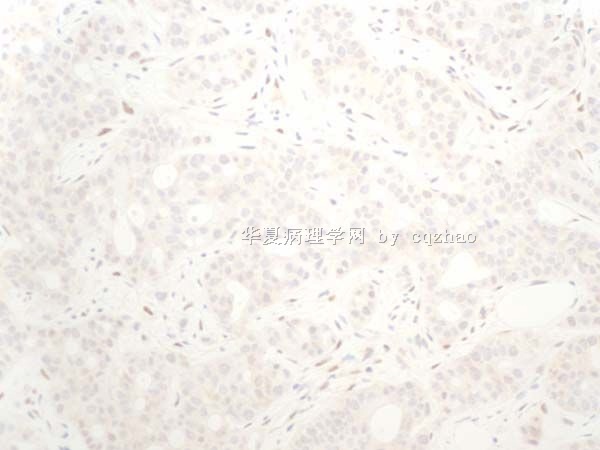
F2 200x
F3 400x
相关帖子
-
本帖最后由 于 2010-06-29 01:20:00 编辑
| 以下是引用cqzhao在2010-6-2 5:07:00的发言:
This women is present with bilateral breast mass. I signed out invasive carcinoma. Comment: most likely it is a metastatic tumor, especially upper GI, such as pancrease. After I signed out I noticed the patient had back mass diagnosed in the similar to my case in another hospital. Morphologic features are not like adenoid cystic ca. Just becasue of some of your comment for this case I did ckit, p63, smmhc. P63 and smmhc are pure negative, ckit weakly and focally positive. Clearly stains are not support ACC also. Till now no primary was found in this patient. However I feel very positive it is metatstic tumor of breast. The reason I showed the case here: We should consider the possiblity of metastasis when we notice some cases with unusual cytomorphology. Thanks, cz
(abin译: 患者有双侧乳房肿块。我签发的是浸润性癌。备注:很可能为转移性肿瘤,特别是上消化道原发者,如胰腺。 发出报告后,我注意到患者在另一家医院发现了背部肿块,诊断和我的病例相似。 形态学特征不像腺样囊性癌。仅仅是由于大家的讨论意见,我才做了CD117、p63、SMMHC。p63和SMMHC全部阴性。CD117局灶弱阳性。很明显这些染色也不支持腺样囊性癌。 至今仍未发现原发灶。然而我觉得很肯定它是转移性肿瘤。 我上传此例的目的:某些少见形态的病例,要想到转移的可能性。 谢谢!cz) |

- 博学之,审问之,慎思之,明辨之,笃行之。
-
qingfengxn 离线
- 帖子:10
- 粉蓝豆:1
- 经验:10
- 注册时间:2010-06-02
- 加关注 | 发消息
-
本帖最后由 于 2010-06-29 01:21:00 编辑
This women is present with bilateral breast mass. I signed out invasive carcinoma. Comment: most likely it is a metastatic tumor, especially upper GI, such as pancrease.
After I signed out I noticed the patient had back mass diagnosed in the similar to my case in another hospital.
Morphologic features are not like adenoid cystic ca. Just becasue of some of your comment for this case I did ckit, p63, smmhc. P63 and smmhc are pure negative, ckit weakly and focally positive. Clearly stains are not support ACC also.
Till now no primary was found in this patient. However I feel very positive it is metatstic tumor of breast.
The reason I showed the case here: We should consider the possiblity of metastasis when we notice some cases with unusual cytomorphology.
Thanks, cz
(abin译:
患者有双侧乳房肿块。我签发的是浸润性癌。备注:很可能为转移性肿瘤,特别是上消化道原发者,如胰腺。
发出报告后,我注意到患者在另一家医院发现了背部肿块,诊断和我的病例相似。
形态学特征不像腺样囊性癌。仅仅是由于大家的讨论意见,我才做了CD117、p63、SMMHC。p63和SMMHC全部阴性。CD117局灶弱阳性。很明显这些染色也不支持腺样囊性癌。
至今仍未发现原发灶。然而我觉得很肯定它是转移性肿瘤。
我上传此例的目的:某些少见形态的病例,要想到转移的可能性。
谢谢!cz)
Mod Pathol. 2006 Oct;19(10):1351-7. Epub 2006 Jun 30.
Immunophenotypic overlap between adenoid cystic carcinoma and collagenous spherulosis of the breast: potential diagnostic pitfalls using myoepithelial markers.
Rabban JT, Swain RS, Zaloudek CJ, Chase DR, Chen YY.
Department of Pathology, University of California, San Francisco, CA 94143, USA. joseph.rabban@ucsf.edu
Abstract
Adenoid cystic carcinoma of the breast is a rare neoplasm whose cribriform architecture may mimic invasive cribriform carcinoma, cribriform ductal carcinoma in situ, and collagenous spherulosis. The diagnosis may be even more challenging in needle core biopsies. Immunohistochemical expression of p63 and c-kit distinguishes adenoid cystic carcinoma from invasive cribriform carcinoma and ductal carcinoma in situ. A formal comparison of the immunophenotype of adenoid cystic carcinoma to collagenous spherulosis has not been reported. Of concern is the overlap in myoepithelial markers between these two entities. Both may express S100, smooth muscle actin, and p63. This overlap may cause diagnostic confusion yet is under-emphasized in the literature. The expression profile of newer myoepithelial markers has not been studied in this setting. We evaluated smooth muscle actin, p63, calponin, smooth muscle myosin heavy chain, as well as c-kit, in nine cases of cribriform pattern adenoid cystic carcinoma of the breast in comparison to 12 cases of collagenous spherulosis. Both entities strongly expressed p63 and smooth muscle actin; in adenoid cystic carcinoma, the basaloid myoepithelial-like tumor cells expressed these markers, but the ductular epithelial cells did not. Neither calponin nor smooth muscle myosin heavy chain was expressed in adenoid cystic carcinoma but both were strongly expressed in collagenous spherulosis. Whereas the ductular epithelial cells of adenoid cystic carcinoma were positive for c-kit in all cases, collagenous spherulosis was negative for c-kit. Positive p63 expression by a cribriform breast lesion is not sufficiently specific to confirm a diagnosis of adenoid cystic carcinoma. A broader panel that includes calponin or smooth muscle myosin heavy chain and c-kit is required to exclude collagenous spherulosis in settings in which the distinctive morphologic features that separate these entities are not conspicuously present. Reliance on p63 or smooth muscle actin alone poses a potential diagnostic pitfall in evaluating cribriform breast lesions.
- Cribriform and tubular carcinoma of breast: both are extensively positive for oestrogen and progesterone receptors but negative for CD117 and p63.
Adenoid cystic carcinoma of the breast
Adenoid cystic carcinoma of the breast is analogous to adenoid cystic carcinoma of the salivary glands.
Epidemiology
Adenoid cystic carcinoma of the breast constitutes 0.1 to 1.0% of all carcinomas of the breast.
Histopathology
The architectural pattern may be trabecular, cribriform, solid or basaloid, usually a combination of these.
Immunohistochemistry
|
|
|
adenoid cystic carcinoma |
infiltrating tubular carcinoma |
infiltrating cribriform carcinoma |
|
|
3/20 (positivity was restricted to only 105% of cells)1 |
10/101 |
10/101 | |||
|
2/20 (both cases positive for progesterone receptors were also positive for oestrogen receptors.)1 |
16/201 | ||||
|
0/201 |
3/20 (weak and incomplete membrane staining)1 | ||||
|
19/201 |
0/101 |
0/101 | |||
|
17/20 (the basaloid cases / areas were negative for p63)1 |
0/101 |
0/101 | |||
|
18/201 |
10/101 |
10/101 | |||
Differential diagnosis
Prognosis
The prognosis is usually good. 10-15% of cases develop metastases to axillary lymph nodes. A solid pattern is associated with more aggressive behaviour, distant metastases and poor five-year survival.
References
1 Mastropasqua MG, Maiorano E, Pruneri G, et al. Immunoreactivity for c-kit and p63 as an adjunct in the diagnosis of adenoid cystic carcinoma of the breast. Mod Pathol 2005; 18:1277-82
华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
- J Clin Pathol. 2003 Oct;56(10):804.
一篇文献,有免费全文:
J Clin Pathol. 2003 Jul;56(7):497-506.
Salivary gland-like tumours of the breast: surgical and molecular pathology.
Pia-Foschini M, Reis-Filho JS, Eusebi V, Lakhani SR.
Department of Pathology, University of Bologna, at Ospedale Bellaria, Bologna, I-40139 Italy.
Erratum in:
Abstract
Breast glands and salivary glands are tubulo-acinar exocrine glands that can manifest as tumours with similar morphological features, but that differ in incidence and clinical behaviour depending on whether they are primary in breast or salivary glands. Salivary gland-like tumours of the breast are of two types: tumours with myoepithelial differentiation and those devoid of myoepithelial differentiation. The first and more numerous group comprises a spectrum of lesions ranging from "bona fide" benign (such as benign myoepithelioma and pleomorphic adenoma), to low grade malignant (such as adenoid cystic carcinoma, low grade adenosquamous carcinoma, and adenomyoepithelioma), to high grade malignant lesions (malignant myoepithelioma). The second group comprises lesions that have only recently been recognised, such as acinic cell carcinoma, oncocytic carcinoma of the breast, and the rare mucoepidermoid carcinoma.
PMID: 12835294 [PubMed - indexed for MEDLINE]PMCID: PMC1769991Free PMC Article

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
-
本帖最后由 于 2010-05-28 20:22:00 编辑
| 以下是引用海上明月在2010-5-28 3:35:00的发言: 如果是乳腺原发的,那会不会是一个非常罕见在乳腺发生的唾腺类型的肿瘤,比如:多形性低度恶性的腺癌或称之为唾腺型终末导管癌。 |
 非常好的提醒。还是乳腺原发的涎腺型癌的可能性大。
非常好的提醒。还是乳腺原发的涎腺型癌的可能性大。
回头看,CK7/CK20并不排除腺样囊腺癌。
HE形态:既有真腺,又有假腺和嗜碱性粘液,但是基底膜样物质不明显。符合腺样囊性癌。它表达肌上皮,这在乳腺癌中是一个例外。
期待Dr.cqzhao揭开谜底、讲解,谢谢!

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
-
本帖最后由 于 2010-05-28 03:10:00 编辑
| 以下是引用cqzhao在2010-5-27 5:18:00的发言:
1. It is like a malignant tumor 2. Do not like any classic type of breast ca 3. If it is a breast ca like this looking, the chance of negative ER/PR is low. Plus GCDFP, mammaglobin negative and ck20 positive. 4. So need to think some things else. |
赵老师发言的大意是:
1.本例看样子是恶性肿瘤;
2.不像是经典型的乳癌;
3.假如是像这样形态的乳癌,那(为什么)ER/PR阴性的几率却是低的,加上GCDFP和mammaglobin(乳球蛋白)却又是阴性,而CK20阳性;
4.所以要考虑其它(类型)。

- 王军臣
-
本帖最后由 于 2010-05-27 05:19:00 编辑
1. It is like a malignant tumor
2. Do not like any classic type of breast ca
3. If it is a breast ca like this looking, the chance of negative ER/PR is low. Plus GCDFP, mammaglobin negative and ck20 positive.
4. So need to think some things else.

 谢谢!需要反复学习反思检讨
谢谢!需要反复学习反思检讨