| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
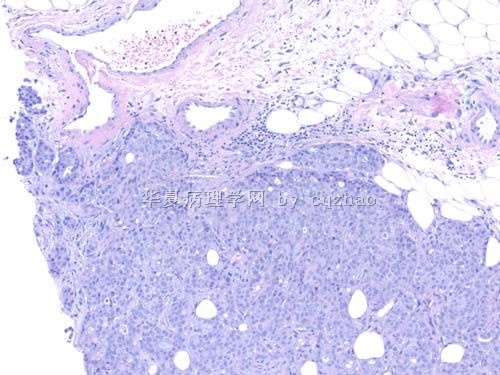
- B267056 y female breast mass, breast core bx (cqz-32 4-22-2010)
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
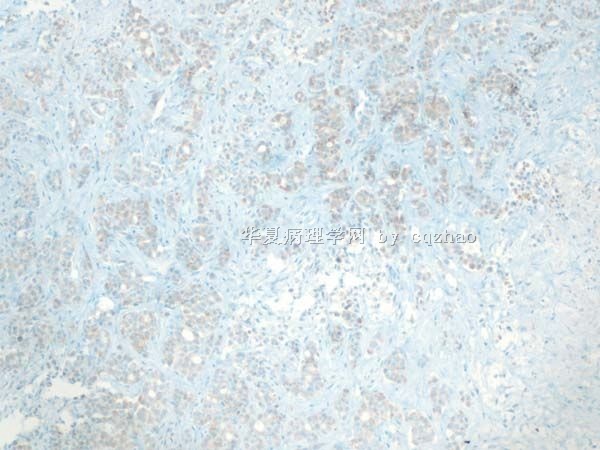
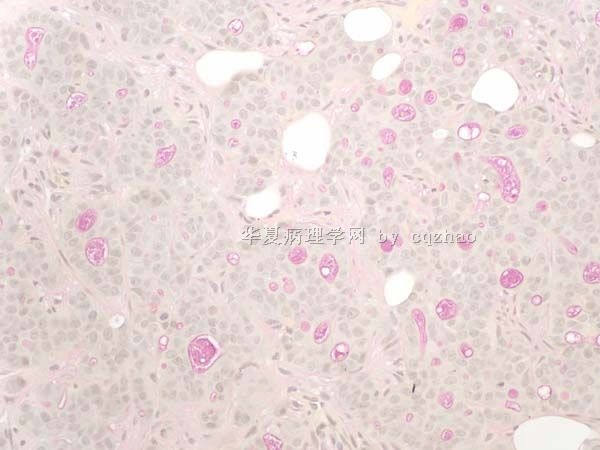
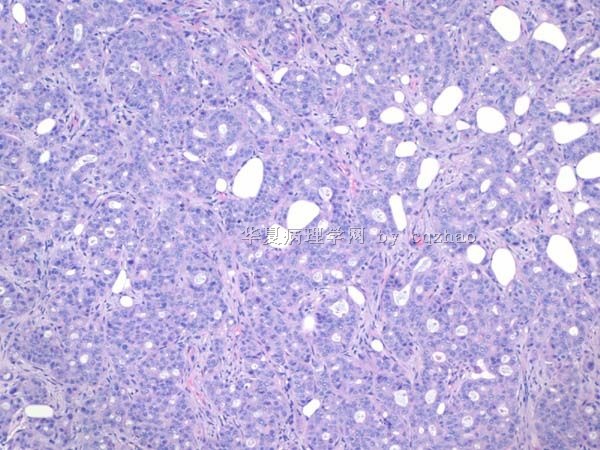
F1 100x
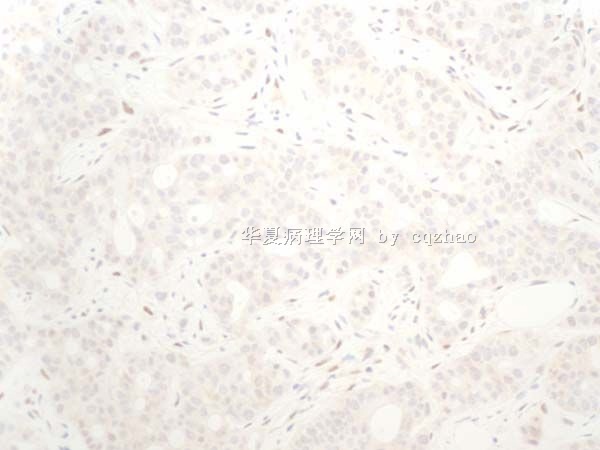
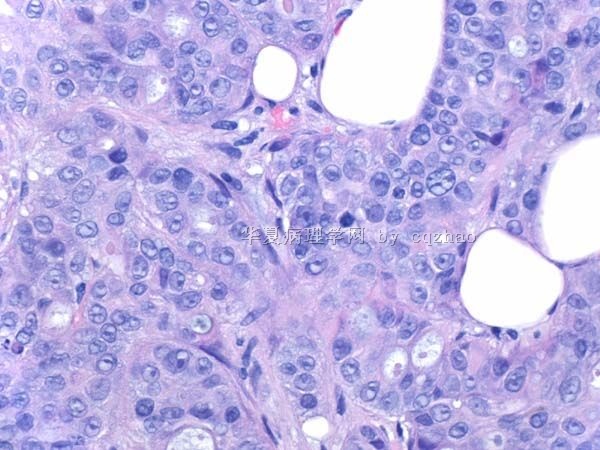
F2 200x
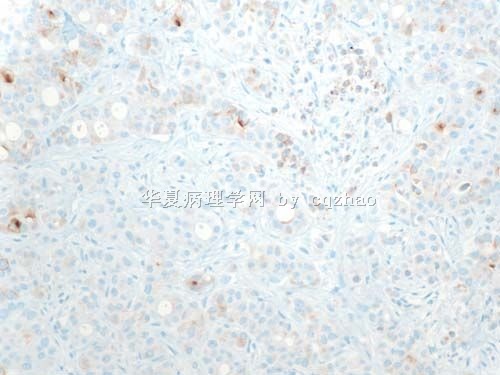
F3 400x
相关帖子
-
本帖最后由 于 2010-06-29 01:21:00 编辑
This women is present with bilateral breast mass. I signed out invasive carcinoma. Comment: most likely it is a metastatic tumor, especially upper GI, such as pancrease.
After I signed out I noticed the patient had back mass diagnosed in the similar to my case in another hospital.
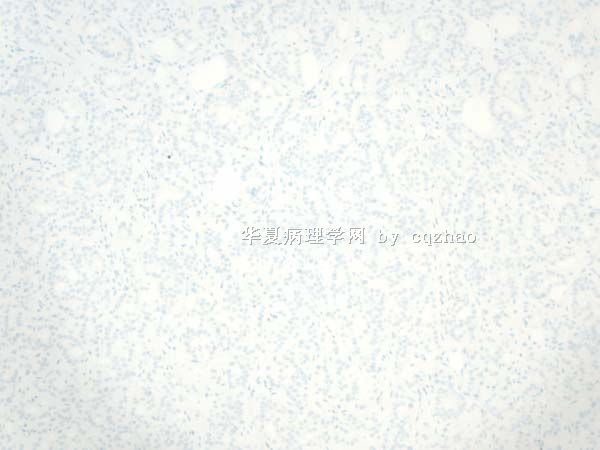
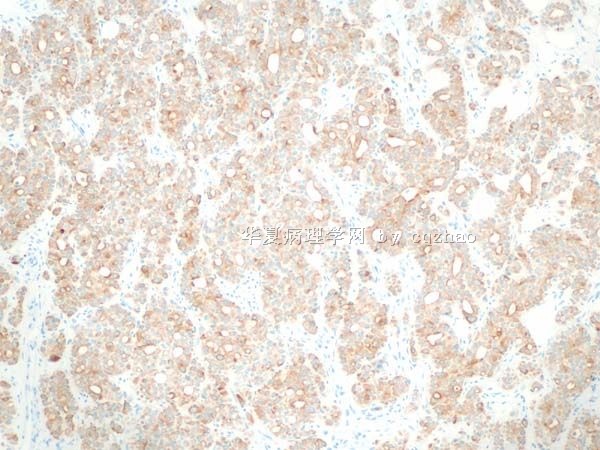
Morphologic features are not like adenoid cystic ca. Just becasue of some of your comment for this case I did ckit, p63, smmhc. P63 and smmhc are pure negative, ckit weakly and focally positive. Clearly stains are not support ACC also.
Till now no primary was found in this patient. However I feel very positive it is metatstic tumor of breast.
The reason I showed the case here: We should consider the possiblity of metastasis when we notice some cases with unusual cytomorphology.
Thanks, cz
(abin译:
患者有双侧乳房肿块。我签发的是浸润性癌。备注:很可能为转移性肿瘤,特别是上消化道原发者,如胰腺。
发出报告后,我注意到患者在另一家医院发现了背部肿块,诊断和我的病例相似。
形态学特征不像腺样囊性癌。仅仅是由于大家的讨论意见,我才做了CD117、p63、SMMHC。p63和SMMHC全部阴性。CD117局灶弱阳性。很明显这些染色也不支持腺样囊性癌。
至今仍未发现原发灶。然而我觉得很肯定它是转移性肿瘤。
我上传此例的目的:某些少见形态的病例,要想到转移的可能性。
谢谢!cz)
Mod Pathol. 2006 Oct;19(10):1351-7. Epub 2006 Jun 30.
Immunophenotypic overlap between adenoid cystic carcinoma and collagenous spherulosis of the breast: potential diagnostic pitfalls using myoepithelial markers.
Rabban JT, Swain RS, Zaloudek CJ, Chase DR, Chen YY.
Department of Pathology, University of California, San Francisco, CA 94143, USA. joseph.rabban@ucsf.edu
Abstract
Adenoid cystic carcinoma of the breast is a rare neoplasm whose cribriform architecture may mimic invasive cribriform carcinoma, cribriform ductal carcinoma in situ, and collagenous spherulosis. The diagnosis may be even more challenging in needle core biopsies. Immunohistochemical expression of p63 and c-kit distinguishes adenoid cystic carcinoma from invasive cribriform carcinoma and ductal carcinoma in situ. A formal comparison of the immunophenotype of adenoid cystic carcinoma to collagenous spherulosis has not been reported. Of concern is the overlap in myoepithelial markers between these two entities. Both may express S100, smooth muscle actin, and p63. This overlap may cause diagnostic confusion yet is under-emphasized in the literature. The expression profile of newer myoepithelial markers has not been studied in this setting. We evaluated smooth muscle actin, p63, calponin, smooth muscle myosin heavy chain, as well as c-kit, in nine cases of cribriform pattern adenoid cystic carcinoma of the breast in comparison to 12 cases of collagenous spherulosis. Both entities strongly expressed p63 and smooth muscle actin; in adenoid cystic carcinoma, the basaloid myoepithelial-like tumor cells expressed these markers, but the ductular epithelial cells did not. Neither calponin nor smooth muscle myosin heavy chain was expressed in adenoid cystic carcinoma but both were strongly expressed in collagenous spherulosis. Whereas the ductular epithelial cells of adenoid cystic carcinoma were positive for c-kit in all cases, collagenous spherulosis was negative for c-kit. Positive p63 expression by a cribriform breast lesion is not sufficiently specific to confirm a diagnosis of adenoid cystic carcinoma. A broader panel that includes calponin or smooth muscle myosin heavy chain and c-kit is required to exclude collagenous spherulosis in settings in which the distinctive morphologic features that separate these entities are not conspicuously present. Reliance on p63 or smooth muscle actin alone poses a potential diagnostic pitfall in evaluating cribriform breast lesions.
-
本帖最后由 于 2010-05-27 05:19:00 编辑
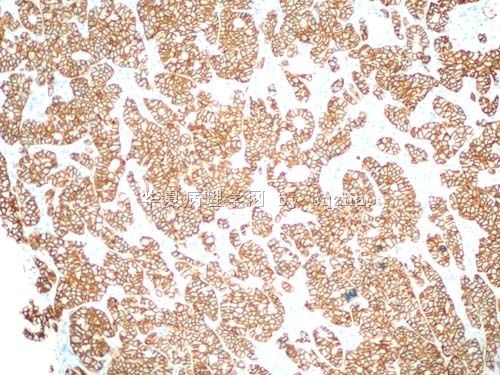
1. It is like a malignant tumor
2. Do not like any classic type of breast ca
3. If it is a breast ca like this looking, the chance of negative ER/PR is low. Plus GCDFP, mammaglobin negative and ck20 positive.
4. So need to think some things else.