| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 小腿肿物
| 性别 | 女 | 年龄 | 31 | 临床诊断 | 神经鞘瘤 |
|---|---|---|---|---|---|
| 一般病史 | 右下肢间断性疼痛3年。 | ||||
| 标本名称 | 小腿肿物 | ||||
| 大体所见 | 灰白结节一个,大小1.1*1cm,包膜完整,切面灰白质中。 | ||||
相关帖子
- • 左小腿肚软组织肿瘤
- • 【20090105】右小腿包块
- • 皮下结节?
- • 小腿皮下肿物
- • 右小腿,血管**瘤?
- • 右小腿皮肤肿块
- • 小腿部肿物(100499)
- • 小腿肿物
- • 左小腿肿块
- • 右小腿皮下肿物
-
liangjinjun 离线
- 帖子:2328
- 粉蓝豆:2
- 经验:2457
- 注册时间:2007-08-07
- 加关注 | 发消息
-
本帖最后由 海上明月 于 2013-09-25 09:35:18 编辑
1、 原单位可以标记vimentin、CD10、PGP9.5、NKI/C3、SMA和CD68
2、 Neurothekeoma 可能和神经没有任何关系,除了上面的文章外,美国外科病理学2009年的文章提到Neurothekeoma和plexiform fibrohistiocytic tumor(丛状纤维组织细胞瘤)有关系,但是只是富于细胞的Neurothekeoma和丛状纤维组织细胞瘤有相关性,而与粘液性Neurothekeoma和混合性Neurothekeoma没有关系
3、文章题名:Neurothekeoma and plexiform fibrohistiocytic tumor: were histologic resemblance or histogenetic relationship?
4、终于好像明白了一些,呵呵,病理还是有点意思的!
-
海上明月: 是的,CD68标记阳性就是一种提示。Neurothekeoma 发生的起源目前尚未阐明。或许不是雪旺细胞起源,但PGP9.5阳性提示与神经似乎脱不了干系。2013-09-25 09:41

- 你所浪费的今天,是昨天死去的人渴望的明天。你所拥有的现在,是明天的你回不去的昨天。
-
本帖最后由 海上明月 于 2013-09-23 09:53:34 编辑
查到美国外科病理学2007年的一篇文章,摘要如下,支持海上明月老师的观点
Neurothekeoma: an analysis of 178 tumors with detailed immunohistochemical data and long-term patient follow-up information.
This report describes the clinicopathologic findings in 176 patients who presented with 178 tumors currently referred to as neurothekeomas. Our study group included 64 males and 112 females, ranging from 20 months to 85 years old at the time of their first surgical procedure (median age: 17 y). Twenty-four percent of patients were <or=10 years of age and only 20% of patients were >or=30 years of age at initial diagnosis. The patients typically presented with a solitary, superficial, slow-growing, and relatively asymptomatic mass in the 0.3 to 2.0 cm size range. One patient had multiple tumors. More than 75% of the lesions involved the head (n=63), upper extremities (n=44), and shoulder girdle (n=27) regions. The tumors were evident a few weeks to 4 years (median duration: approximately 7 mo) before surgical resection was sought. Histologically, the lesions involved the dermis and/or subcutis, and they formed multinodular masses with varying amounts of myxoid matrix and peripheral fibrosis. On the basis of the amount of myxoid matrix, the tumors were subclassified as cellular (n=63), mixed (n=67), or myxoid (n=48). All cases had spindled and epithelioid mononuclear neoplastic cells with relatively abundant cytoplasm and indistinct cell borders. The majority of cases also had occasional multinucleated tumor cells. The lesional cells had a strong tendency for whorled growth, and oftentimes, focal fascicular growth was also present. Nuclear atypia was minimal in 62 cases, mild in 73 cases, at least focally moderate in 41 cases, and focally marked in 2 cases. Mitotic activity ranged from 0 to 124 mitotic figures/25 wide-field high power fields (WHPFs) (median mitotic count: 4 mitotic figures/25WHPFs). Twenty-five lesions had >10 mitotic figures/25WHPFs. A total of 16 cases (9%) had atypical mitotic figures. Osteoclastlike giant cells were detected in 39% of cases. Immunoreactivity was typically present for vimentin, NKI/C3, CD10, microphthalmia transcription factor, and PGP9.5, and focal reactivity was sometimes noted for smooth muscle actin and CD68. All tumors tested were negative for S100 protein, glial fibrillary acidic protein, and Melan A. The overwhelming majority of cases had involvement of the tissue margins. A complete follow-up record is available for 71 patients (40.3%) with follow-up intervals ranging from 3 years 2 months to 34 years 9 months (median: 17 y 9 mo). Limited or incomplete follow-up information is also available for an additional 14 patients with follow-up intervals ranging from weeks to approximately 10 years (median: 5 mo). Regrowth of tumor after biopsy or local excision was reported in 13 patients, one of whom had 2 recurrences. However, because of the nature of our consultation practice and a tendency for clinicians to specifically send us cases with a complex clinical course, this is believed an overestimation of the true recurrence rate. Neurothekeomas are morphologically and immunohistochemically distinct from true nerve sheath myxomas. An origin from fibroblastic cells with the ability to differentiate into myofibroblasts and a tendency to recruit histiocytic cells is postulated.

- 你所浪费的今天,是昨天死去的人渴望的明天。你所拥有的现在,是明天的你回不去的昨天。
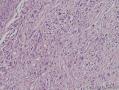
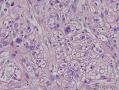
本例的诊断思维建议由神经鞘粘液瘤演绎,诊断为 Neurothekeoma
有以下符合的依据、特点和鉴别要点:
1)神经鞘粘液瘤和 Neurothekeoma的共同特点:(1)可发生于肢体,局限于真皮(本例符合);(2)分布呈小叶状 多结节,小叶间被纤维间隔分开,小叶分界清晰(本例符合);(3)小叶内间质呈粘液样基质(本例符合);(4)肿瘤细胞主要成分之一为梭形细胞。等等。
2)神经鞘粘液瘤和 Neurothekeoma的不同点:(1)发病年龄30-50岁多见,但前者偏向年龄大一些的成人多,后者偏向青少年或年轻一些成人多;男女比例是前者男性多,后者女性多;(2)前者为梭形细胞与星形细胞成分,细胞较稀疏,可见细胞突起,小叶内黏液基质较多,偶见类圆细胞,而Neurothekeoma主要为梭形细胞和肥胖的类圆形细胞成分,细胞较前者丰富,小叶内黏液基质较前者明显少,类圆形上皮样细胞多,其胞质丰富,胞质突起不大显形;(3)前者肿瘤细胞基本没有异型性,难以见到核分裂;而Neurothekeoma的瘤细胞核多,染色较深,,有轻度异型性,见核分裂;(4)这一条最重要,就是前者是具有施万细胞/或神经支持细胞分化,因此表达S-100蛋白(S100+)等神经标志物;而Neurothekeoma的组织发生和分化尚未阐明,不具有施万细胞/或神经支持细胞分化,因此绝大多数病例不表达S-100蛋白(S100-)。
本例S-100阴性,结合那么多胖梭形/类圆形的上皮样细胞等特点,完全支持诊断Neurothekeoma。
本例细胞这么丰富,也可以考虑富于细胞性神经鞘粘液瘤,但S-100阴性不支持。
3)本例虽然是丛状小叶状分布,易与丛状神经纤维瘤混淆,但至少有两点是不支持丛状神经纤维瘤的:
(1)本例有胖梭形类圆形上皮样细胞成分,这是丛状神经纤维瘤不易见到的,而神经纤维常呈细长形,可见波纹状形态,不会有类圆形上皮样细胞和星形细胞的;再说丛状神经纤维瘤是儿童好发的。
(2)丛状神经纤维瘤与神经鞘粘液瘤多表达S-100蛋白,而本例S-100阴性,故不支持丛状神经纤维瘤,也不支持丛状神经鞘瘤,而支持Neurothekeoma的诊断。
以上纯属个人意见。仅供参考!

- 王军臣
-
本帖最后由 笑笑之人 于 2013-09-22 18:31:01 编辑
今天利用早晨工作之余,复习了外周神经中带有“丛状”字样的肿瘤,对它们的认识也再次加深了,现在将我的理解综述如下:
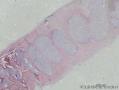
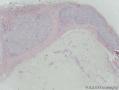
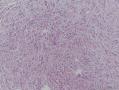
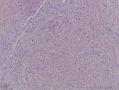
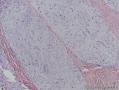
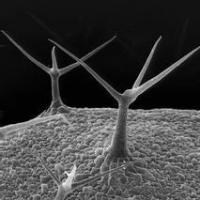
1、“丛状”只是一个形态学上的诊断,如同“乳头状”、“管状” 和“绒毛状” 一样,是形态学诊断而已,关键还是后面的肿瘤名称,如丛状神经纤维瘤,那就必须具备神经纤维瘤的一切特征;丛状神经鞘瘤就必须具备神经鞘瘤的一切特征 。图1是丛状神经纤维瘤,图2是丛状神经鞘瘤,大家自己看看对不?
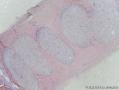
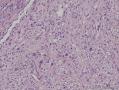
2、神经鞘粘液瘤,既不是神经纤维瘤的亚型,也不是神经鞘瘤的亚型,它是一个其它独立的肿瘤,是发生在表皮内的一个疾病,是结节状而不是丛状!(图三是神经鞘粘液瘤的图)
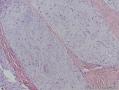
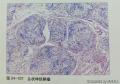
3、图四是本病例,大家自己看看像哪一个,我个人觉得是结节状,而不是丛状,所以还是更像神经鞘粘液瘤。当然它应该在表皮内,如果楼主能提供更加详细的资料就好了!
4、谢谢!

- 你所浪费的今天,是昨天死去的人渴望的明天。你所拥有的现在,是明天的你回不去的昨天。
病理分型为二类(见后),组织病理改变基本相似,
经典型(Classic nerve sheath myxomas):肿瘤局限,境界清楚,位于真皮内,粘液基质细胞型(Cellular nerve sheath myxomas):肿瘤边界不清,呈浸润生长,可侵及皮下,
假若是这个瘤子,一般要与皮肤一同切除,因为神经鞘黏液瘤属于皮肤病变。
-
本帖最后由 笑笑之人 于 2013-09-20 16:58:58 编辑
病理分型为二类(见后),组织病理改变基本相似,
经典型(Classic nerve sheath myxomas):肿瘤局限,境界清楚,位于真皮内,粘液基质细胞型(Cellular nerve sheath myxomas):肿瘤边界不清,呈浸润生长,可侵及皮下,

- 你所浪费的今天,是昨天死去的人渴望的明天。你所拥有的现在,是明天的你回不去的昨天。
由于神经鞘黏液瘤与神经纤维瘤关系密切,二者的鉴别目前仅具有理论意义。
但是区别一种肿瘤的亚型和搞的非常清楚一种肿瘤组织学类型好像是每一位病例医师的常规工作态度。
神经鞘黏液瘤是一种局限于真皮的梭形细胞肿瘤,瘤细胞呈清晰的小叶状分布,小叶内的间质呈黏液样,小叶之间为纤维性间隔。此瘤多发生于30-50岁间的成年人,可发生于躯体的任何部位,但以四肢远端最为多见;高倍镜下瘤细胞主要由梭形细胞和肥胖的类圆形上皮样细胞组成,并可见到合体性的多核巨细胞。而这些特征在丛状神经纤维瘤中难以见到。
丛状神经纤维瘤同样比较少见,但多发生于儿童,多于幼儿期发病,好发生于头颈部,多累及神经,特别是神经丛,几乎均发生于伴有NF1的患者。丛状神经纤维瘤可波及四肢,严重时称神经瘤型橡皮病,皮肤松弛臃肿,色素沉积严重,其下骨组织肥大。肉眼观,丛状神经纤维瘤病变范围较大,可波及大段神经,使受累神经扭曲呈“蠕虫状”。若病变较小,其丛状生长方式仅在镜下可见,则不应该诊断丛状神经纤维瘤。
鉴于以上组织学图像结合临床病史、发病部位及年龄均需首先考虑神经鞘黏液瘤。