- 2012年第27期——尿道与阴道间隙肿块(已点评)
| 性别 | 女 | 年龄 | 49 | 临床诊断 | |
|---|---|---|---|---|---|
| 临床症状 | 阴道肿块,并无疼痛 | ||||
| 标本名称 | 尿道与阴道间隙肿块 | ||||
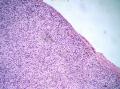
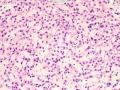
| 大体所见 | 淡黄色卵圆形包块1枚,2cm×1.5cm×1cm,切面亮白色,质韧。 | ||||
本例图片采用麦克奥迪MoticBA410显微镜+MoticamPro285A摄像头采集制作。
点评专家:王曦
点评专家:王曦(42楼 链接:>>点击查看<< )
获奖名单:xhyong(12楼 链接:>>点击查看<< )
-
本帖最后由 冰洋 于 2012-08-08 09:50:23 编辑

知之者不如好之者,好之者不如乐之者。(语出幽梦影)
-
本帖最后由 TK1905 于 2012-07-07 07:56:23 编辑
- Superficial, circumscribed bland lesion of external female genital tract
- Superficial cervicovaginal myofibroblastoma
- Restricted to external female genital tract
- Vagina, cervix, vulva
- Superficial circumscribed
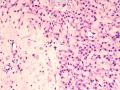
- No capsule
- Frequent grenz zone between lesion and epithelium
- No entrapped fat
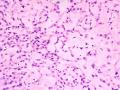
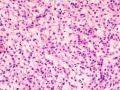
- Uniform bland stellate and spindled cells
- Oval, elongate nucleus, frequently wavy
- Even chromatin
- Small nucleolus
- 2/26 cases with a few multinucleated cells
- 4/26 cases with mild pleomorphism
- Variable patterns of cellularity
- Moderately to highly cellular overall
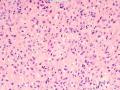
- Densely collagenous foci with vague fascicles
- Myxoid foci
- Lace-like or sieve-like pattern
- Cells surround nodules of collagen or myxoid stroma
- Mean age 55 years
- Only 2 of 26 cases under age 38
悲催啊!在鉴别诊断中又看见一个病:浅表性肌纤维母细胞瘤(又名浅表性宫颈阴道肌纤维母细胞瘤),觉得也很像,甚至就是它,但除了一点,即本例取材整个肿块未见阴道粘膜上皮覆盖在肿块之上,不知道手术中该肿块是否真位于阴道粘膜表浅???
浅表性肌纤维母细胞瘤:好发于阴道(占绝大多数)、宫颈、会阴,年龄绝大多数是围绝经期、绝经后,体积也很小,大多低于6cm,平均2-3cm左右。
镜下无包膜,常位于阴道的粘膜鳞状上皮下,肿块与粘膜下软组织有不清楚的交界。
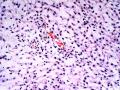
血管不显著,细胞可呈中等数量到高度富于细胞(本例就是这样),细胞主要为星状细胞、梭形细胞,细胞温和,罕见核分裂,极少数例子伴有轻微的局灶的多形性。可以有局灶或部分上皮样细胞。也可以有疏松密集区交替。疏松区细胞呈蕾丝花边样或筛状、网状排列,富于细胞区可局灶密集胶原纤维伴有不甚清楚的束状排列,无陷入的脂肪细胞。
和血管肌纤维母细胞瘤主要鉴别点就是没有显著的血管,本例血管确实不是很突出,很少,不是主要病变。围绕血管生长不是很明显。
细胞形态上浅表性肌纤维母细胞瘤以星状+梭形为主,本例星状、梭形、上皮样均有;血管肌纤维母细胞瘤以上皮样细胞为主,且始终在薄壁血管周生长或成簇或条索
IHC:CD34、Vim、PR、ER、Desmin大多数例子均+,SMA部分例子表达。
Definition
Alternate/historical names
Diagnostic Criteria
Superficial cervicovaginal myofibroblastoma: fourteen cases of a distinctive mesenchymal tumor arising from the specialized subepithelial stroma of the lower female genital tract.
Source
Department of Pathology, Northwestern University Medical School, Chicago, IL, USA.
Abstract
The clinicopathologic features and immunohistochemical profiles of 14 cases of a distinctive mesenchymal tumor that arises in the superficial lamina propria of the cervix and vagina and is histologically distinguishable from mesodermal (fibroepithelial) stromal polyp, including the cellular (pseudosarcomatous) variant, angiomyofibroblastoma, aggressive angiomyxoma, and other well-recognized lesions that occur in this location, are described. The lesions presented as a polypoid (n = 10) or nodular (n = 4) mass in the vagina (n = 12) or cervix (n = 2) of women ranging in age from 40 to 74 years (median, 58 years). The tumors were subepithelial in location, were well circumscribed, and ranged in size from 1 to 6.5 cm. (mean, 2.7 cm). Microscopically, the process was moderately to highly cellular and composed of relatively bland spindled and stellate-shaped mesenchymal cells embedded in a finely collagenous stroma that was punctuated by myxoid and edematous foci in 9 cases. The lesions characteristically had a multipatterned architecture with tumor cells focally assuming a lacelike/sievelike growth pattern in the more stroma-rich areas of the tumor and a vague fascicular growth pattern in the more cellular foci. Mitotic activity was minimal, and no atypical mitotic figures were identified. The tumors were immunoreactive (in decreasing order of relative strength) for vimentin (5 of 5 cases), estrogen (10 of 10 cases), and progesterone (10 of 10 cases) receptors, desmin (13 of 13 cases), CD34 (11 of 13 cases), alpha-smooth muscle actin (5 of 11 cases), and muscle-specific actin (2 of 8 cases). The desmin and CD34 antibodies highlighted the interconnecting, dendritic processes associated with many of the tumor cells. No immunoreactivity was detected for S100 protein, epithelial membrane antigen, or keratins. Follow-up data for 11 patients (range, 1 to 20 years; median, 4 years) showed no recurrence or metastasis after local excision. The term "superficial cervicovaginal myofibroblastoma" is proposed because it reflects the distinguishing features of this benign, relatively site-specific mesenchymal tumor. The process probably arises as a neoplastic proliferation of hormonally responsive mesenchymal cells native to the unique subepithelial stromal layer normally found through the endocervix and vulva of adult women.
Superficial cervico-vaginal myofibroblastoma: a report of five cases.
Source
Department of Pathology, King Edward Memorial Hospital, Subiaco, Western Australia, Australia. colin.stewart@sjog.org.au
Abstract
AIMS:
To describe the pathological and immunohistochemical features of five cases of superficial cervico-vaginal myofibroblastoma (SCVM), a recently described mesenchymal tumour affecting middle-aged and elderly females.
METHODS:
The histological features of five cases of SCVM arising in four patients were reviewed including one case which recurred locally 9 years after initial excision biopsy. All cases were immunostained using the streptavidin-biotin technique using antisera to vimentin, smooth muscle actin, desmin, S100 protein, cytokeratin, h-caldesmon, calponin, CD99, CD117 (c-kit), bcl-2, oestrogen receptor and progesterone receptor.
RESULTS:
The patients were aged from 40 to 71 years (mean 55.2 years). The tumours were situated within the vagina (four cases) and cervix (one case) and ranged from 16 to 45 mm in greatest dimension. One patient had two separate vaginal SCVM. The tumours were characterised by uniform spindle and stellate-shaped cells separated by a collagenous or myxoid stroma. No mitotic activity was identified. Characteristically the tumours were well circumscribed and separated from the surface epithelium by a rim of normal stroma. The initial and recurrent tumours in one patient were similar except for increased stromal collagen in the recurrence. All tumours were immunoreactive for vimentin, desmin, CD34, CD99, bcl-2, calponin and hormone receptors while two tumours showed focal smooth muscle actin expression. There was no expression of S100 protein, h-caldesmon, CD117 or cytokeratin.
CONCLUSIONS:
SCVM appears to be a relatively distinct lesion although there is some histological and immunophenotypical overlap with other mesenchymal tumours, particularly fibroepithelial polyp, leiomyoma and solitary fibrous tumour. As local recurrence developed 9 years after intial treatment in one patient, long-term clinical follow-up would seem appropriate.
Vulvovaginal myofibroblastoma: expanding the morphological and immunohistochemical spectrum. A clinicopathologic study of 10 cases.
Source
GF Ingrassia Department, Section of Anatomic Pathology, Policlinico Universitario-Vittorio Emanuele, University of Catania, 95123 Catania, Italy. g.magro@unict.it
Abstract
We analyzed the clinicopathologic features of 10 cases of vulvovaginal myofibroblastoma to widen its morphological and immunohistochemical spectrum. Most tumors (8/10 cases) were located in the vagina. The patients' age ranged from 44 to 77 years, and tumor size ranged from 0.4 to 3 cm. Histologically, 5 tumors had the characteristics of vulvovaginal myofibroblastoma. In addition, we identified 3 cases composed of spindle-shaped cells arranged in short fascicles with intervening thick collagen bands, closely reminiscent of mammary myofibroblastoma. Notably, 1 case resembled Sertoli cell tumor, sclerosing type, because of its predominant cord-like arrangement. In another case, there were highly cellular areas composed of uniform-packed, rounded cells that, at low magnification, looked like a malignant "small round blue cell tumor." A variably thick band of native connective tissue separated tumors from the overlying squamous epithelium even if, in 3 cases, tumor cells extended up to the epithelium. In 7 cases, a variable number of vessels showed perivascular hyalinization. Only rare mitotic figures were identified. All tumors were diffusely positive for vimentin, desmin, and CD99. A variable staining intensity was observed for CD34, Bcl-2, B-cell lymphoma 2 (Bcl-2) CD10, estrogen receptor, and progesterone receptor in most cases, but none expressed α-smooth muscle actin. We emphasize that vulvovaginal myofibroblastoma encompasses a morphological spectrum wider than previously described. The overlapping morphological and immunohistochemical features of vulvovaginal and mammary myofibroblastomas led us to speculate that these are related entities with morphological variations on a common basic theme likely dependent on anatomical location.
A wide variety of mesenchymal lesions occur in the lower female genital tract.5,6 Broadly, these mesenchymal lesions can be separated into two groups. The first group includes several well-characterized tumors that show a marked tendency to occur in the lower female genital tract, such as aggressive angiomyxoma, angiomyo- fibroblastoma, and cellular angiofibroma.7-9 These tumors can also be called as relatively site-specific. The second group embraces a wide range of heterogeneous lesions that frequently occur in this region, but arise in other anatomic sites as well, with examples as fibroepithelial stromal polyp, superficial angiomyxoma and leiomyoma.
SCVM represents a new member of the first group. SCVM appears underrecognized. To our knowledge, only 31 cases of SCVM have been reported so far in the literature.1-4 The current four cases raise the number to 35. These 35 cases occurred in 34 patients ranging in age from 23 to 80 years with mean of 57 years. To date, 32 patients (94%) were in their peri- or post-menopausal years. Eleven (32%) patients had received Tamoxifen or hormone- replacement therapy. Clinically, the most common presentation was an asymptomatic polypoid nodule or mass, with cysts or polyps being the most preoperative diagnosis. Thirty patients presented with solitary nodular mass, whereas 4 patients had two separated lesions. Thirty tumors were located in the vagina or vaginal fornix, 3 in the cervix and 2 in the vulva. Because the tumor also occurred in the vulva, Ganesan et al2 suggested the term superficial myofibroblastoma of the lower female genital tract to replace SCVM.
Overall, most SCVM were described as polyps or had a polypoid outline, measuring 1.0 cm to 8.0 cm (mean, 2.5 cm) in diameter. Histologically, SCVM was characterized by its superficial subepithelial location and uniform spindle and stellate cells arranged in diverse growth patterns within a myxoid to collagenous stroma. Tumor cells in SCVM typically expressed vimentin, desmin, CD34, ER and PR, with desmin and CD34 accentuating the dendritic processes of the cytoplasm, whereas actins was consistently negative.
Due to some histological and immunohistochemical overlapping features, SCVM can be confused with other mesenchymal lesions of the lower female genital tract. The principal differential diagnosis is FSP, especially the cellular variant.9 As described in the original paper, 4 cases had been primarily diagnosed as FSP. The younger population of FSP, absence of distinct Grenz zone in FSP, lack of heterogeneous cellularity and diverse growth patterns, are crucial features to distinguish SCVM from FSP.9 The other tumor enters the differential diagnosis is angiomyofibroblastoma (AMF). AMF is also characterized by alternating hypercellular and hypocellular areas. However, unlike SCVM, AMF contains abundant small to medium sized blood vessels. The tumor cells in AMF also have a propensity to grow around the vessels. Furthermore, SCVM is frequently negative for α-smooth muscle actin. In contrast, AMF is usually positive for actins.8 Cellular angiofibroma (CA) is another site-specific mesenchymal tumor that should be considered in the differential diagnosis. CA usually involves the vulva and the inguinoscrotal region. CA differs from SCVM by its numerous small- to medium-sized thick-walled vessels and negative stainging for desmin. Other lesions that may be confused with SCVM include leiomyoma, solitary fibrous tumor (SFT) and mammary-type myofibroblastoma.10 Vulvovaginal leiomyoma often shows a hyalinized or myxoid stroma, so called myxohyaline pattern. In addition to desmin, ER and PR, the tumor cells in leiomyoma are also positive for actins. SFT is another tumor which may display alternating cellularity. In contrast to SCVM, SFT is typically positive for CD34 and negative for desmin. Mammary-type myofibroblastoma is a spindle cell tumor with morphological and immunophenotypic features identical to myofibroblastoma of breast. Mammary-type myofibroblastoma shows a predilection for the inguinal area of older men. Only one case has been reported in the vaginal wall.11 In our opinion, this case is possibly a lesion of SCVM.
The pathogenesis of SCVM is not well understood. However, nearly one third of SCVM patients had a history of Tamoxifen or hormone-replacement therapy, suggesting that hormones may possibly have a role in the development of the tumor. It has been postulated that the subepithelial mesenchymal cells of the lower female genital tract, which are normally estrogen and progesterone positive, tend to be the origin of most site-specific mesenchymal tumors that arising in this site.1
Follow-up information was available in 30 cases of SCVM. Twenty-nine cases pursued a benign outcome with no evidence of recurrence or metastasis. Only one patient experienced local recurrence 9 years after initial excision biopsy.3 As there is limited potential for local recurrence, complete local excision is curable for SCVM. Nevertheless, long-term follow-up is recommended.
In conclusion, SCVM represents a distinctive entity which shows a marked predilection for the superficial aspect of the lower female genital tract, predominantly the vagina. Hormones may be involved in the growth of the tumor. Although this new entity is of little relevance to the gynecologist for therapeutic decisions, awareness of its unique clinical and histological features is helpful for the pathologists at differential diagnosis.
诊断:血管肌纤维母细胞瘤
依据:部位可算是会阴、阴道壁肿物。无症状。体积很小。镜下:低倍边界清楚,非侵袭性生长的,但也没有明确的假包膜(这点和平滑肌瘤有点不一样)。肿瘤细胞的分布特征构成肿块有疏松、密集区域交替。中高倍可见血管为薄壁血管,肿瘤实质细胞为上皮样、浆细胞样细胞或梭形细胞呈索状、簇状生长。但围绕血管不是很明显(这点有点和血管肌纤维母细胞瘤不一致),背景可见肥大等炎症细胞,但总体肿瘤细胞还算在薄壁血管周有规律排列生长。
IHC:CD34、Desmin、PR、ER、actin
鉴别诊断:
侵袭性血管粘液瘤:边界不清,侵袭生长,体积更大,背景更富于粘液而实质细胞更稀疏
平滑肌瘤:形态变异大,要依靠IHC
富于细胞性血管纤维瘤:玻璃样变小-中等大血管明显,肿瘤细胞排列无规律,很随意。和本例完全相反