| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
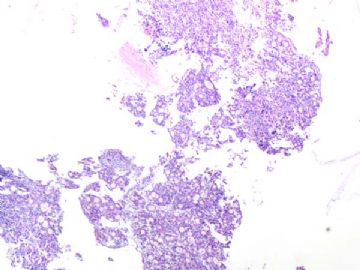
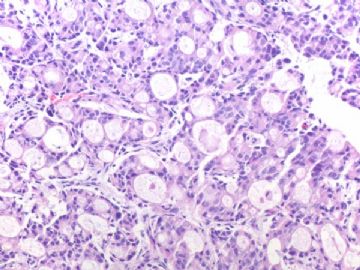
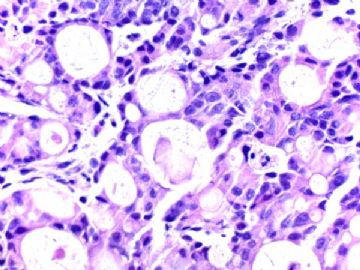
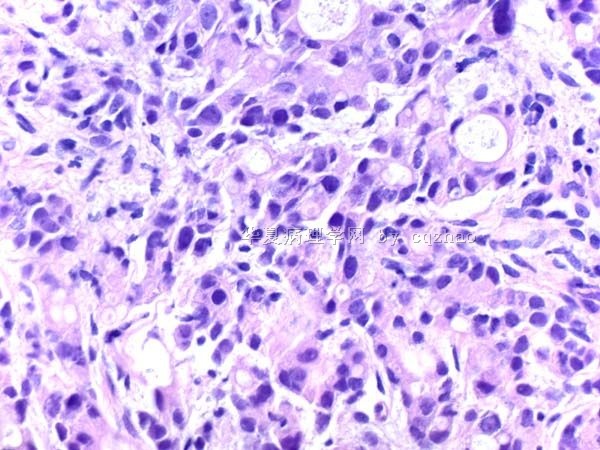
- B291244 y/f vaginal bleeding, endometrial biopsy
(女,44岁,阴道不规则出血,子宫内膜活检)
40x
200x
400x
-
本帖最后由 于 2010-10-02 09:19:00 编辑
相关帖子
| 以下是引用cqzhao在2010-10-2 2:57:00的发言: Do not move the case please |


- If you have great talents, industry will improve them; if you have but moderate abilities, industry will supply their deficiency. 如果你很有天赋,勤勉会使其更加完美;如果你能力一般,勤勉会补足其缺陷。
-
本帖最后由 于 2010-10-02 18:27:00 编辑
| 以下是引用abin在2010-10-2 9:28:00的发言:
欢迎大家讨论:诊断思路?鉴别诊断?初步诊断? Dr.cqzhao能否提供一张带有正常内膜的图片?供比较,会简化难题,谢谢! 另外,有没有特殊病史?实际工作中遇到这种情况就要打电话问临床了。 |
Reasonable.
1 This was a consult case last week.
2. The specimen with scant tissue. The low power photo show all field of the specimen. No normal endometrial tissue seen.
3. Patient had history of breast cancer in 2003 when she was 36 year. She had mastectomy. Very bad luck...
 谢谢Dr.cqzhao!
谢谢Dr.cqzhao!
内膜标本呈明显的腺样结构,分化不算太差,但是没有内膜腺体或间质起源的迹象。既然有乳腺癌病史,我重点考虑乳腺癌转移。
鉴别诊断:
继发性腺癌(乳腺癌首选)?
原发的少见腺癌(怎么看也不像啊,没有一种内膜癌亚型能对得上号)
免疫组化(mammaglobin,GCDFP-15、CK、Vimentin)和/或复习乳腺癌切片有助于诊断。
我只见过一例乳腺癌转移到内膜和卵巢,为浸润性多形性小叶癌。

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
-
本帖最后由 于 2010-10-03 07:33:00 编辑
非常好的病例,36岁(2003)时患有乳腺癌,44岁子宫内膜刮出组织中见腺癌。
病理诊断应该从二个方面考虑:
1)原发性内膜样腺癌,特殊类型(Endometrioid adenoncarcinoma with a microglandular pattern)
首先,年轻乳腺癌患者很可能有遗传史,如BREA-1、BRCA-2基因突变;HNCPP、Lynch综合症等易患因素。其次乳腺癌病人抗雌激素治疗也是发生内膜癌的危险因素之一。
2)乳腺癌转移
鉴别诊断的简单方法是复习2003年乳腺癌病理切片,根据形态考虑诊断和IHC标记,WT-1可用于鉴别乳腺和内膜癌。
谢谢!

- xljin8
| 以下是引用xljin8在2010-10-3 7:31:00的发言:
非常好的病例,36岁(2003)时患有乳腺癌,44岁子宫内膜刮出组织中见腺癌。 病理诊断应该从二个方面考虑: 1)原发性内膜样腺癌,特殊类型(Endometrioid adenoncarcinoma with a microglandular pattern) 首先,年轻乳腺癌患者很可能有遗传史,如BREA-1、BRCA-2基因突变;HNCPP、Lynch综合症等易患因素。其次乳腺癌病人抗雌激素治疗也是发生内膜癌的危险因素之一。 2)乳腺癌转移 鉴别诊断的简单方法是复习2003年乳腺癌病理切片,根据形态考虑诊断和IHC标记,WT-1可用于鉴别乳腺和内膜癌。 谢谢! |
赞赏金主任的精辟分析。乳腺癌转移至子宫不能除外。
如果是子宫原发性微小腺体型腺癌,可能主要见于宫颈管内膜发生或宫颈。
本例的形态学不同于一般的宫内膜腺癌,形态学更倾向乳腺浸润性导管癌转移至子宫。

- 王军臣
|
乳腺癌转移到女性生殖道很少见。有文献报道主要是转移到子宫内膜和卵巢,转移到子宫颈罕见。 本例报道的是乳腺浸润性导管癌同期转移到子宫颈。 Arch Gynecol Obstet. 2010 Apr;281(4):769-73. Epub 2009 Oct 30. Breast cancer with synchronous massive metastasis in the uterine cervix: a case report and review of the literature.Bogliolo S, Morotti M, Valenzano Menada M, Fulcheri E, Musizzano Y, Casabona F. Department of Gynecology, Breast Unit, University of Genoa, 10 Largo Rosanna Benzi, Genoa, Italy. stefanobogliolo@libero.it AbstractINTRODUCTION: Metastatic breast cancer is rare in the female genital tract, and when present it more commonly tends to involve ovary or endometrium; uterine cervix is only occasionally involved. This condition poses differential diagnostic problems in the settings of clinical and pathological investigations. CASE PRESENTATION: An asymptomatic 78-year-old woman came to our attention in the context of routine gynecological surveillance; clinical examination disclosed enlarged uterine body and cervix. Our patient then underwent computed tomography and magnetic resonance imaging that outlined the possibility of cervical cancer with parametrial involvement. Moreover, a suspect mass was found on the mammogram in the left breast. Breast surgical excision was performed, which revealed invasive breast carcinoma, while synchronous cervical biopsy discovered distant metastasis in the uterine cervix. On histological examination, both lesions showed non-cohesive architectural pattern consistent with lobular morphology; anyway, to rule out primary poorly differentiated cervical cancer, appropriate immunohistochemical panel was performed, which confirmed the mammary derivation of the tumor. Due to disseminate disease, the patient underwent multisystemic medical treatment including radiotherapy, chemotherapy and hormone therapy, and she is still alive at 30-month follow-up. DISCUSSION: Genital tract metastases in patients with known breast carcinoma can present with abnormal vaginal bleeding, but they often are asymptomatic. Therefore, only strict gynecological surveillance of these patients can permit early detection of these secondary lesions. Aggressive treatment of isolated cervical metastasis should be performed when feasible; otherwise, systemic chemotherapy with taxane could be sufficient in increasing survival. It should be emphasized that, in most cases, only accurate immunohistochemical investigation, particularly if performed on the primary lesion as well, can solve differential diagnostic problems and allow the clinician to establish appropriate treatment. |

- 王军臣
本例报道进展期乳腺癌出现阴道流血,病理证明为乳腺癌转移至子宫内膜。转移癌的形态结构有些像蜕膜样的结构特点,像是内膜本身间质发生的病变,但细胞异型、核分裂以及表达乳清蛋白等标志物可鉴定为转移性乳腺癌。
Arch Gynecol Obstet. 2009 Feb;279(2):199-201. Epub 2008 May 10.
Abnormal uterine bleeding as a presentation of metastatic breast disease in a patient with advanced breast cancer.
Karvouni E, Papakonstantinou K, Dimopoulou C, Kairi-Vassilatou E, Hasiakos D, Gennatas CG, Kondi-Paphiti A.
Department of Pathology, Aretaieion Hospital, University of Athens, Athens, Greece.
Abstract
BACKGROUND: Extragenital carcinomas secondarily involving the uterus are very rare and they usually occur as a manifestation of widespread disease. When the metastases involve the endometrium in a diffuse, permeative pattern, sparing the glands, they may cause problems in the diagnosis.
CASE: A case of metastatic carcinoma to the endometrium with a decidua-like pattern is reported. The patient had a history of breast carcinoma and presented with vaginal bleeding. The pathologic findings in the uterine curettings raised the differential diagnosis between metastatic breast carcinoma and non-neoplastic stromal lesions. The presence of nuclear atypia and mitotic activity along with the appropriate immunohistochemical findings revealed the neoplastic nature of the endometrial lesion and confirmed its origin from the breast.
CONCLUSION: Unusual uterine bleeding in a patient with breast cancer should alert the gynecologist to the possibility of metastatic breast disease. Furthermore, the metastasis to the uterus and to other organs of the genital tract can be considered as a preterminal event.

- 王军臣