| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
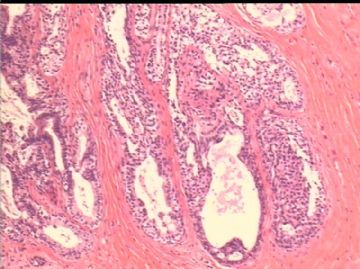
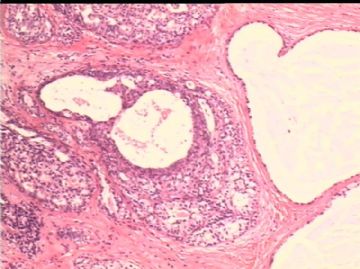
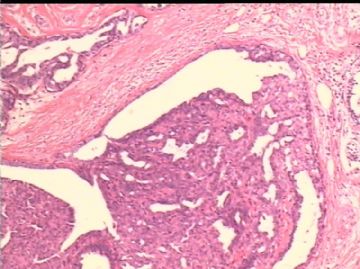
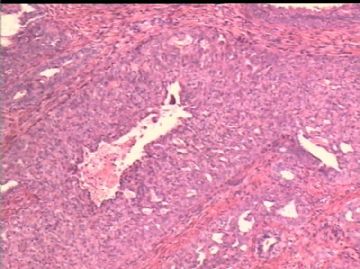
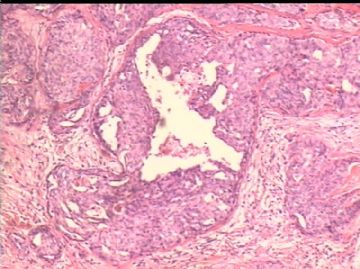
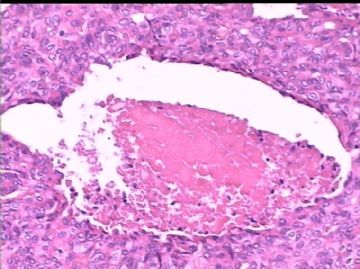
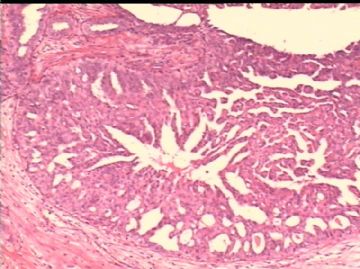
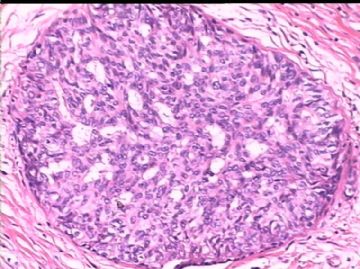
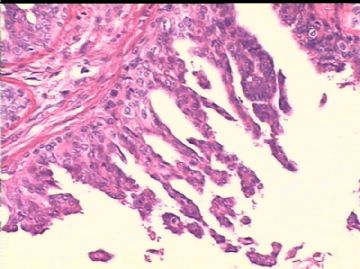
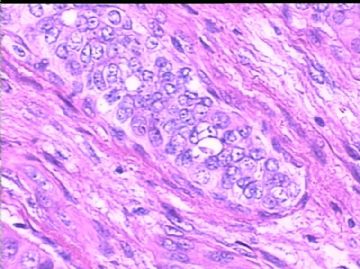
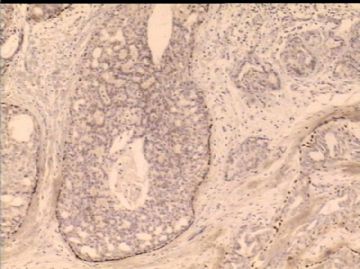
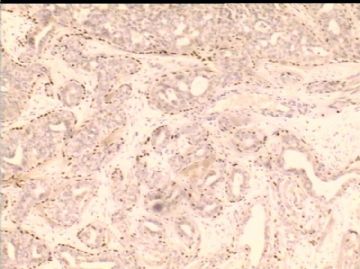
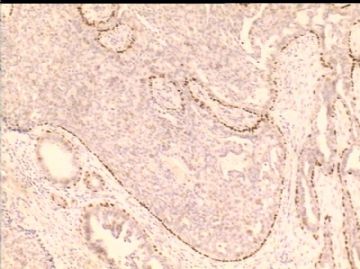
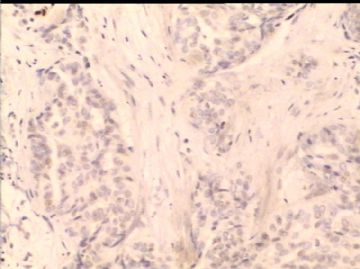
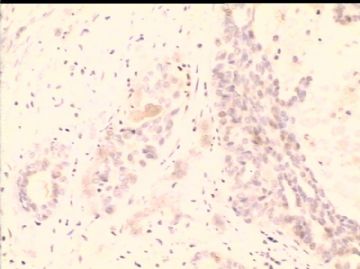
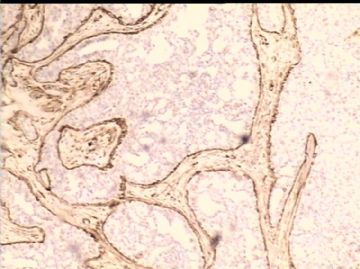
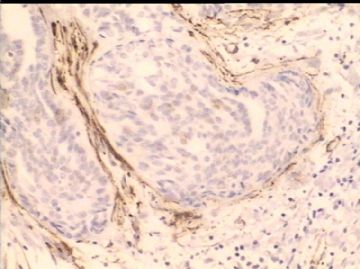
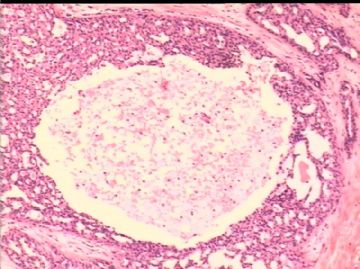
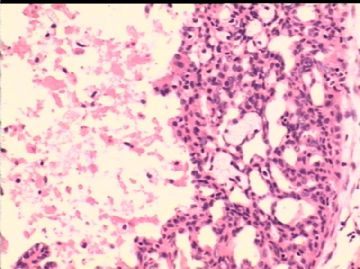
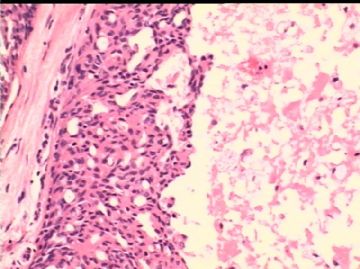
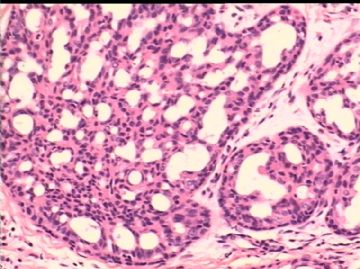
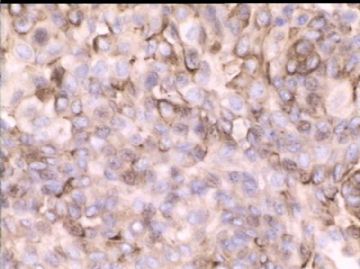
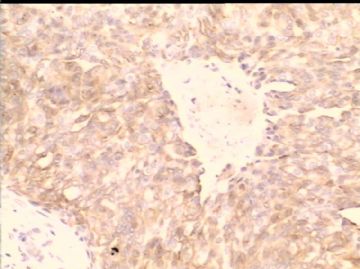
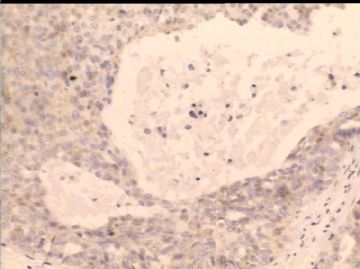
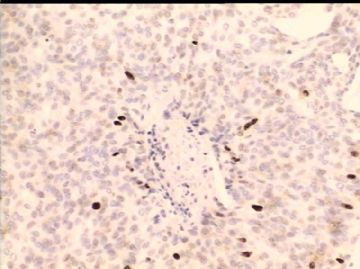
- B2503女/48岁,右乳腺肿瘤 1.2cm, 诊断?
| 姓 名: | ××× | 性别: | 女 | 年龄: | 48岁 |
| 标本名称: | 右乳腺肿块 | ||||
| 简要病史: | 发现肿块2月余。 | ||||
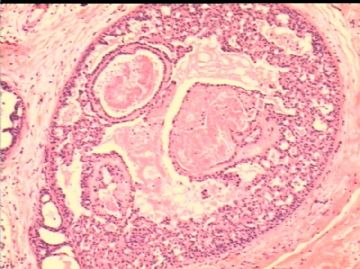
| 肉眼检查: | 乳腺组织一块,1.8 x1.7cm, 中央见一灰红色结节,直径1.2 cm, 边界清楚,无包膜。 | ||||
-
本帖最后由 于 2010-02-21 12:27:00 编辑

- xljin8
相关帖子
- • 乳腺癌?
- • 乳腺肿物
- • 乳腺肿物
- • 左乳癌标本乳头一个导管内的病变
- • 乳腺两个相邻导管内的病变
- • 乳腺肿物,请各位老师帮忙会诊
- • 女 46岁发现左乳腺肿块一月余
- • 乳腺肿物
- • 乳腺肿物
- • 左乳肿块
-
yanghuaijun 离线
- 帖子:106
- 粉蓝豆:1
- 经验:106
- 注册时间:2009-08-23
- 加关注 | 发消息
It is not an easy case especially evaluating based on the photos only.
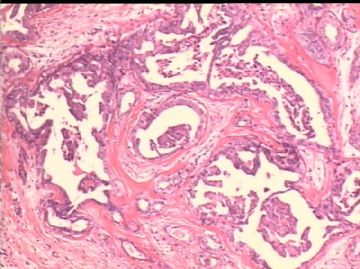
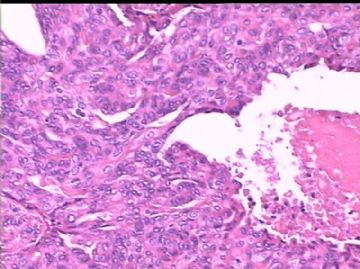
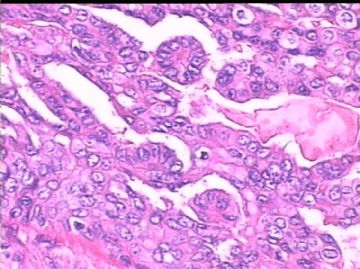
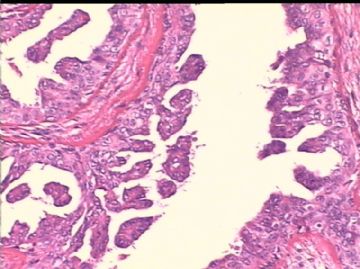
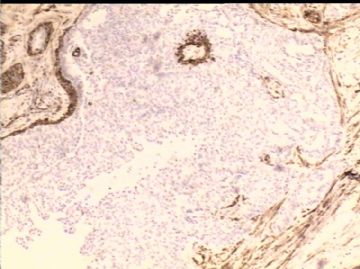
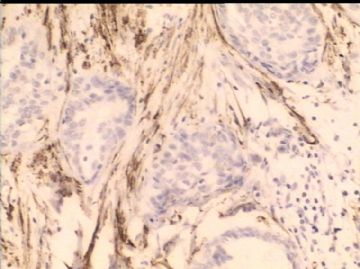
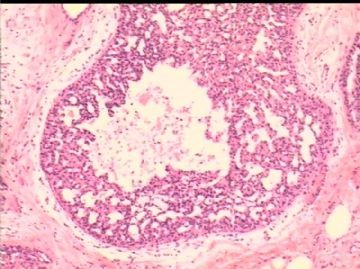
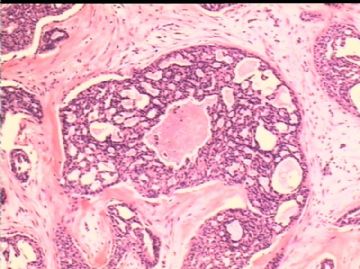
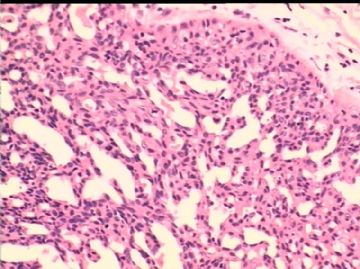
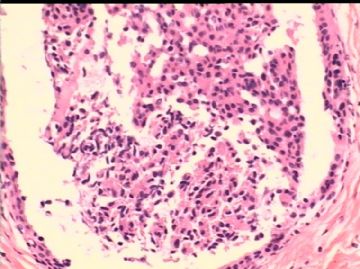
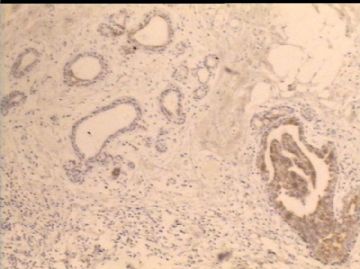
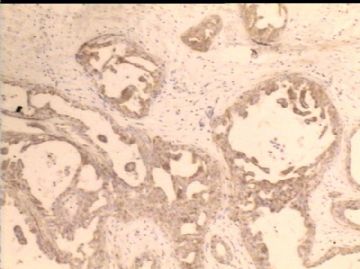
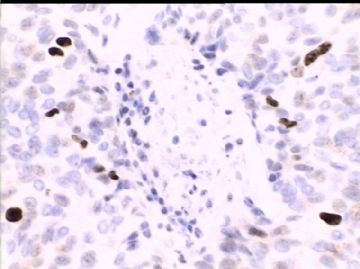
1. Generally speaking it is a papillary lesion.
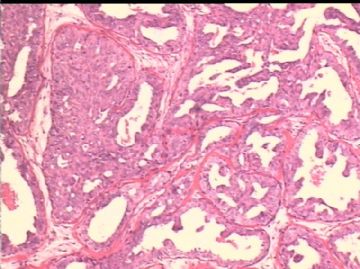
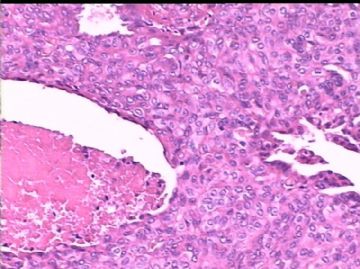
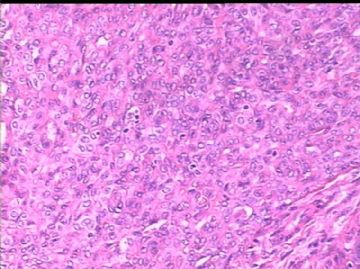
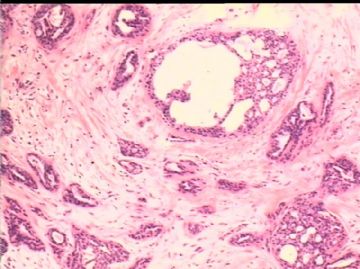
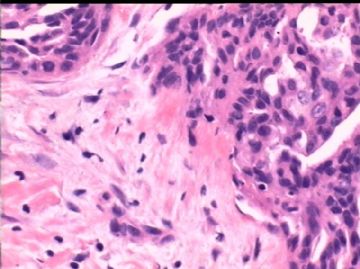
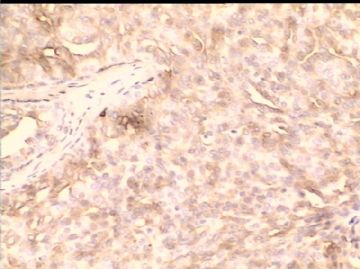
2. Features: Sclerosing, ductal epithelial proliferation, necrosis.
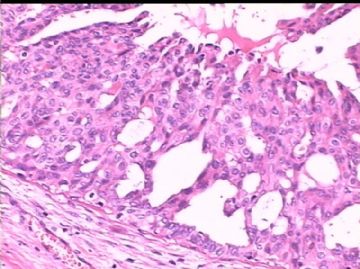
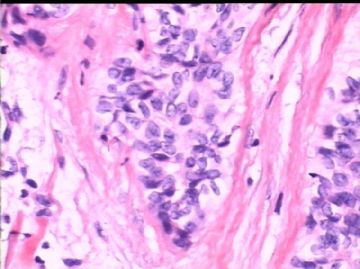
3. Cytomorphologic features are not like DCIS, such as streaming, nuclei varing in size and overlapping, cellular swirling, fenestrations. Of cause I do not think it is invasive tumor.
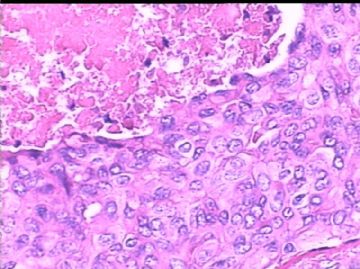
4. Atypical features: focal micropapillary growth, foally with a little monotanous prolifearion, focal central necrosis (though it is not unusual to see the necrosis in UDH).
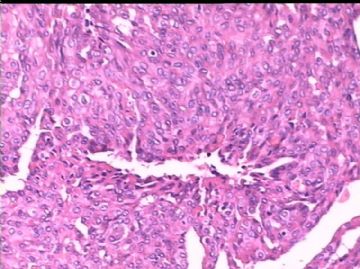
5. I favor a dianosis of atypical papilloma based on above features.
Of cause if you want to write more you can diagnos as atypical papilloma with sclerosis and ductal epithelial hyperplasia with focal necrosis.
6. The only differential dx for me is solid papillary ca. But thinking over I denied the dx.
7. I Often noticed the people suggested to use IHC for UDH, ADH, DCIS. It is useless. It is a morphologic dx for these three, not IHC. If the cases showed IHC results well, they should be easily diagnosed by H&E. If they are borlerline cases by H&E, they will not be distinguished by IHC also. I as a breast/gyn pathologist rarely know the pathologists still use the IHC for differential dx of UDH, ADH, and DCIS in the USA. In 2004 I once started to do a study in this area, I gave up this research after I got the prelimary result.
Dr. Schnitt , Beth Israel Medical center, Harvard once had a breast IHC review paper mentioning the usage of HMW CK. He also mentioned this part in his 2009 breast biopsy book. I asked him in persion in last uscap meeting about IHC for udh, adh, dcis. He said they did not use IHC also in this situation.
Of cause you can still use IHC stains if you feel they can help you.
Thank Dr. Jin for sharing the chellange case. Just for your reference. cz
试译赵老师发帖,献给谦虚的wfbjwt 
“小荷把翻译团队请回来吧,不然赵老师发帖我看不懂了。”
http://www.ipathology.cn/forum/forum_display.asp?keyno=230468
这不是个简单的病例,尤其是仅仅基于以上所传图片。
1、 整体来看,这是个乳头状病变;
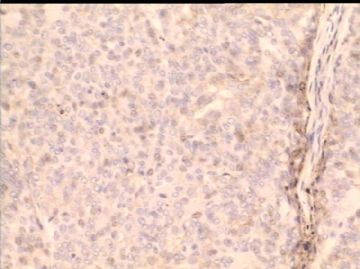
2、 特征:硬化背景,导管上皮增生,管腔内中央性坏死;
3、 细胞形态学特征:流水样及漩涡状排列,胞核大小不一及重叠,窗孔特点(边窗及扁圆形窗孔)等,这些均不提示DCIS。当然,前提是我认为这不是浸润性癌。
4、 非典型特征:灶区微乳头状生长方式、局灶单一性增生及中心性坏死(虽然极少数UDH也可见坏死)。
5、 基于以上特征,我倾向诊断为非典型性乳头状瘤。当然,如果你想更具体,可以这样诊断——伴硬化的非典型乳头状瘤,合并导管上皮增生伴中心性坏死。
6、 对我来说,唯一的鉴别诊断是实性乳头状癌,但仔细思考后我还是放弃了这一诊断。
7、 我注意到经常有人建议用IHC来鉴别UDH, ADH, DCIS,实际上,IHC在这类疾病鉴别中意义不大,三者的鉴别主要还是依靠形态学特征。如果这些病例显示典型的IHC结果,那H&E也很容易鉴别。作为乳腺与妇科病理工作者,我知道现在在美国很少有病理医生还用IHC来作UDH, ADH和DCIS的鉴别诊断。2004年,我曾经着手想做这方面的科研工作,但我看了初始结果后就放弃了。
Dr. Schnitt , Beth Israel Medical center, Harvard曾经在他关于乳腺IHC的综述性文章中提及HMW CK的用法, 2009年,他在其《乳腺活组织检查》书中再次提及相关话题。去年uscap会议时,我曾私下请教过他udh, adh, dcis中免疫标记的应用问题,他说他们在这种情况下不做IHC。
当然,如果你们认为免疫标记有帮助,你们仍然可以做。
谢谢金教授分享这一富于挑战的病例。
仅供参考!cz
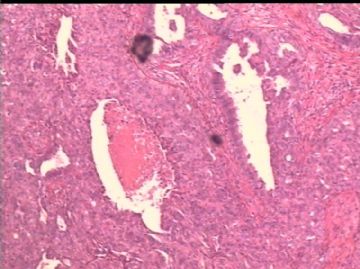
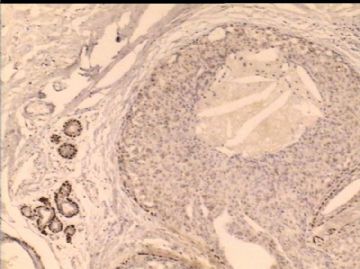
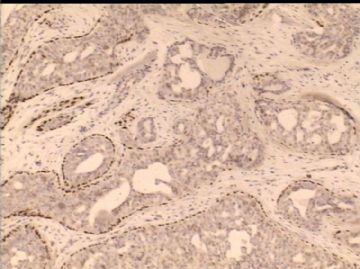
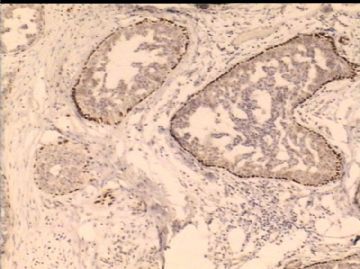
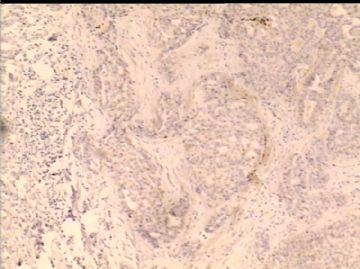
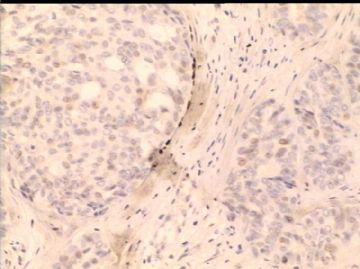
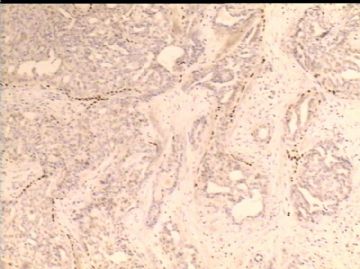
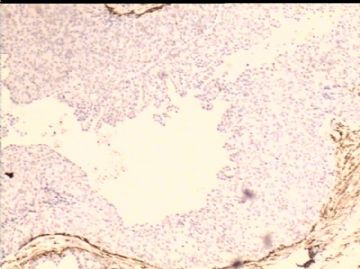
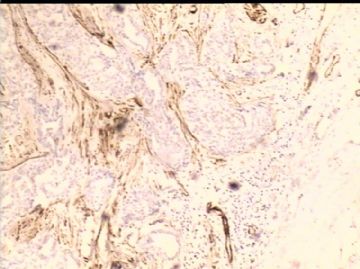
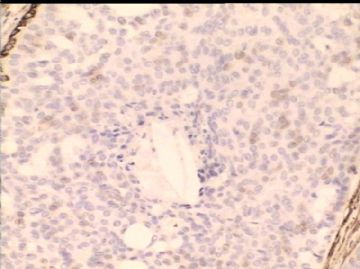
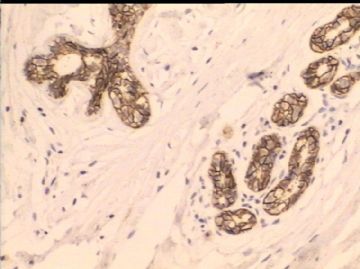
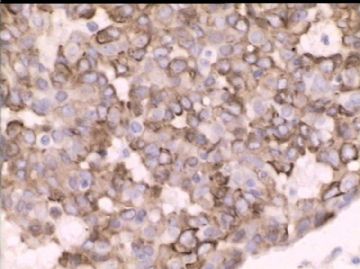
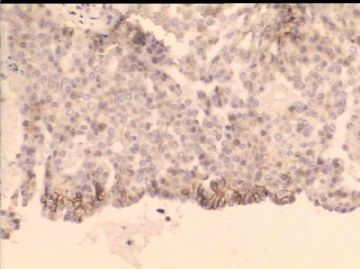
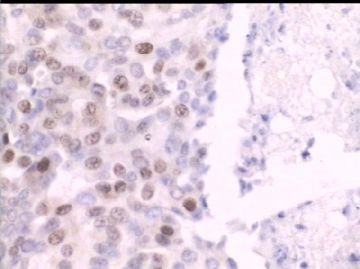
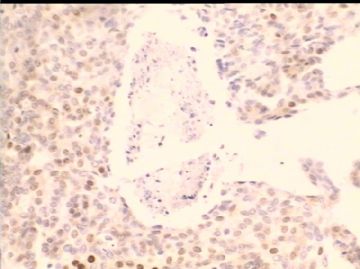
1、伴坏死的UDH。细胞增生具UDH特征,伴中央性坏死病灶。这种情况虽然少见,但如果结构和细胞特征都支持UDH诊断的话,坏死的存在并不能除外UDH的诊断。
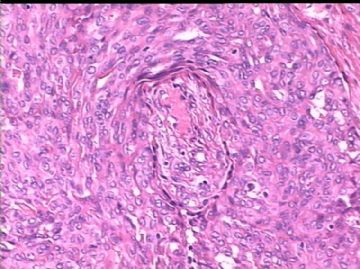
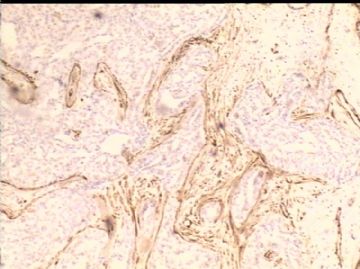
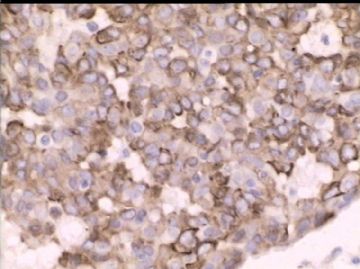
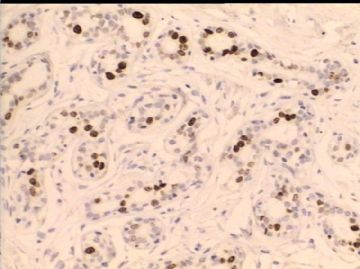
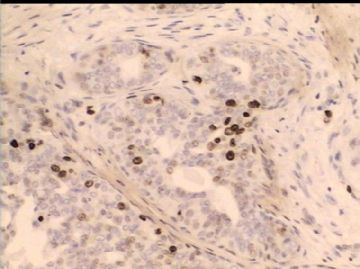
2、CK5/6的免疫染色在疑难病例诊断中有一定价值,典型镶嵌样表达模式的CK5/6染色倾向UDH,而明确CK5/6阴性细胞支持ADH及DCIS,但需注意有部分高级别DCIS表达CK5/6阳性,但其核的异型性和多形性可助和UDH鉴别;
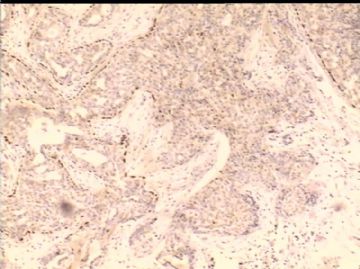
ER/PR染色也有一定辅助作用,正常导管上皮阳性(内对照)。UDH染色和周围相对正常导管上皮无差别,而ADH及DCIS的染色和周围相比常有差别,或阴性或强阳性或深浅有变化。但并不绝对,需结合HE具体分析。
ADH和小的低级别DCIS非常困难,尤其是小的DCIS,这是个有争议的话题。
3、CK5/6免疫染色显示UDH的特征性改变—镶嵌样图象(腺、肌两种上皮)。