| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
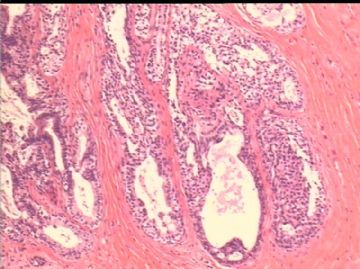
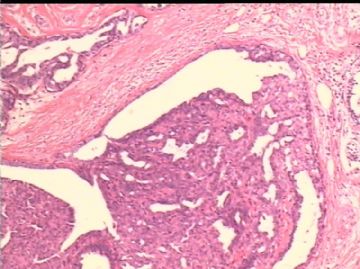
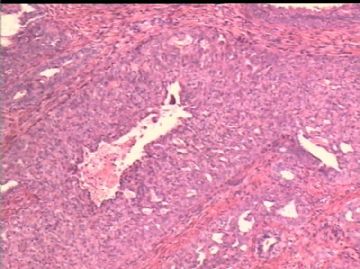
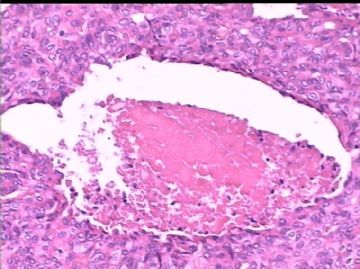
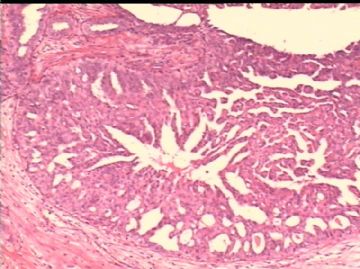
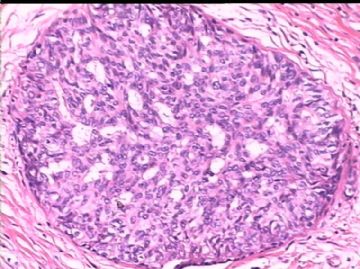
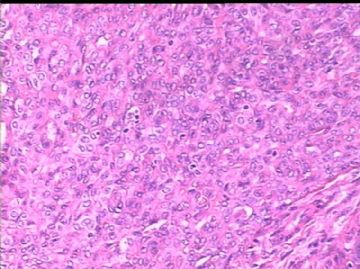
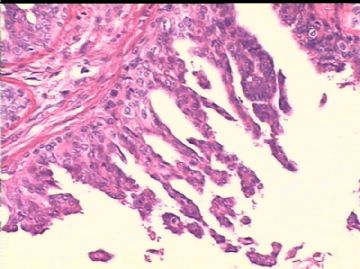
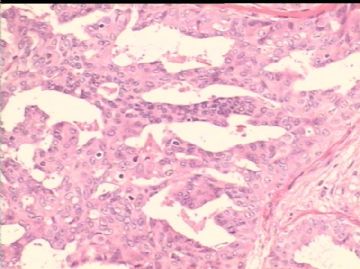
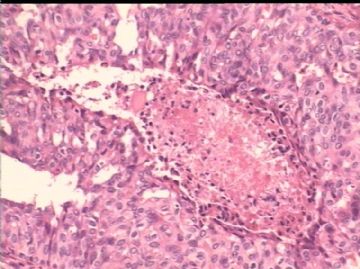
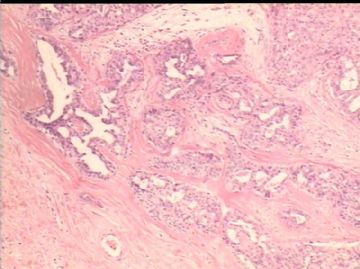
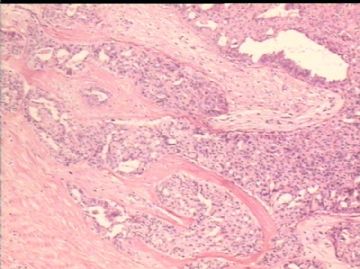
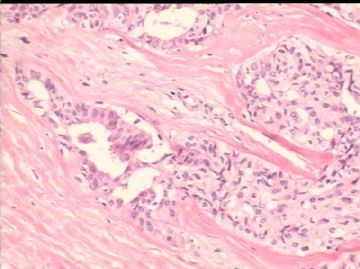
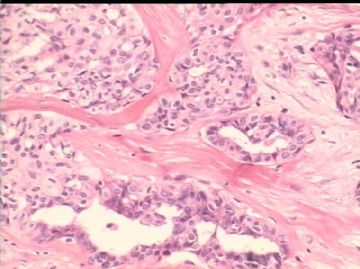
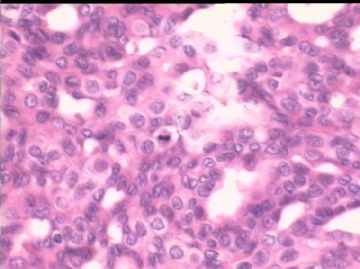
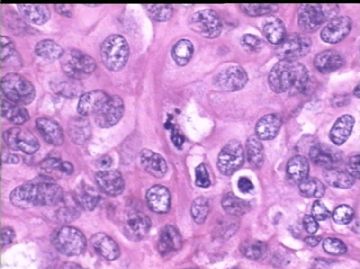
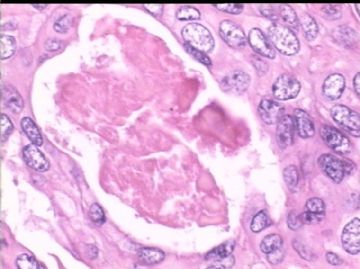
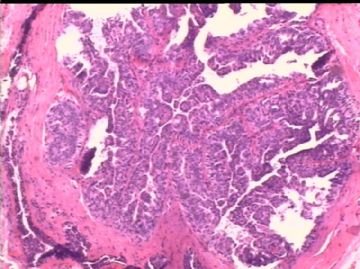
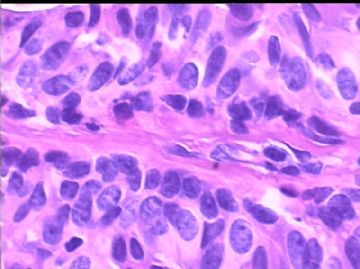
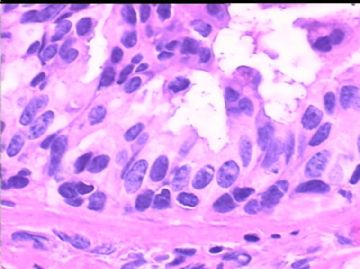
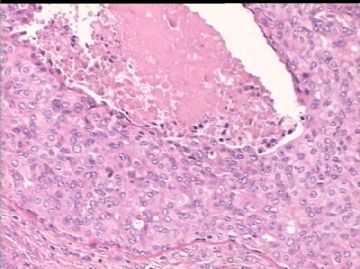
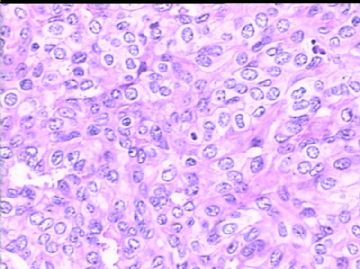
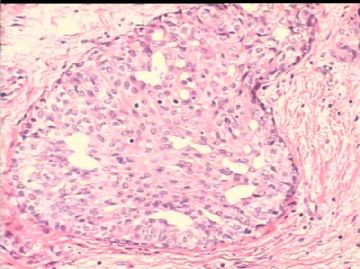
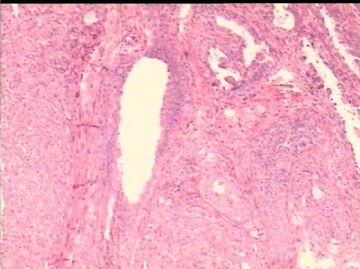
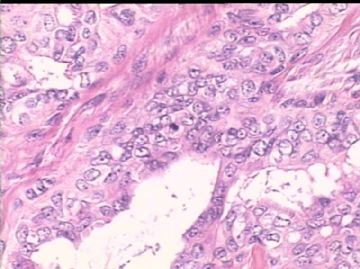
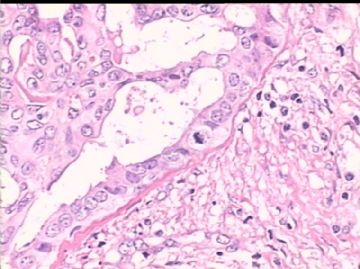
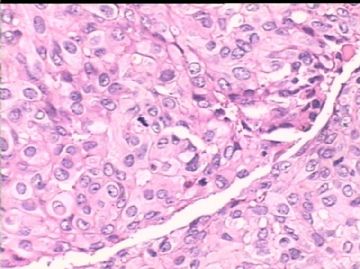
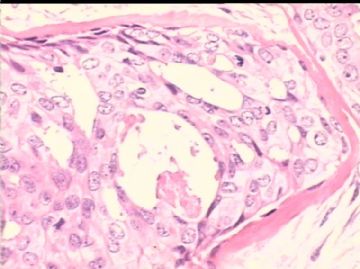
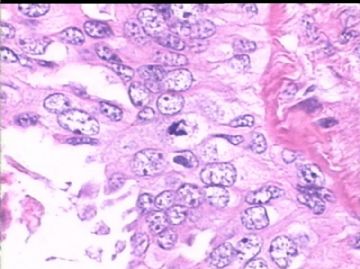
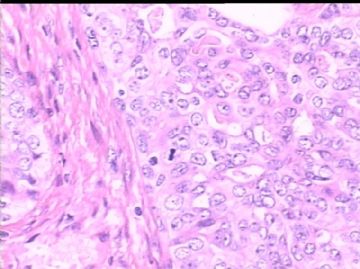
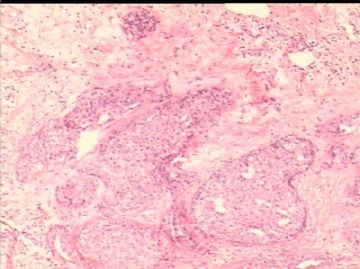
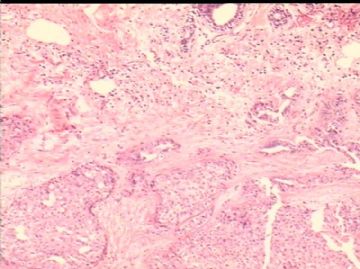
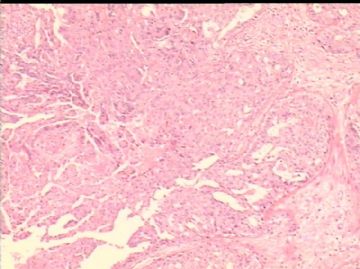
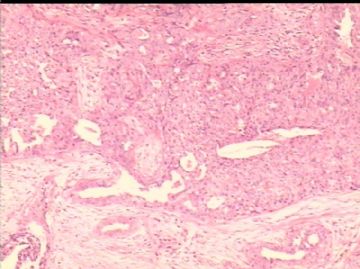
- B2503女/48岁,右乳腺肿瘤 1.2cm, 诊断?
| 姓 名: | ××× | 性别: | 女 | 年龄: | 48岁 |
| 标本名称: | 右乳腺肿块 | ||||
| 简要病史: | 发现肿块2月余。 | ||||
| 肉眼检查: | 乳腺组织一块,1.8 x1.7cm, 中央见一灰红色结节,直径1.2 cm, 边界清楚,无包膜。 | ||||
-
本帖最后由 于 2010-02-21 12:27:00 编辑

- xljin8
相关帖子
- • 乳腺癌?
- • 乳腺肿物
- • 乳腺肿物
- • 左乳癌标本乳头一个导管内的病变
- • 乳腺两个相邻导管内的病变
- • 乳腺肿物,请各位老师帮忙会诊
- • 女 46岁发现左乳腺肿块一月余
- • 乳腺肿物
- • 乳腺肿物
- • 左乳肿块
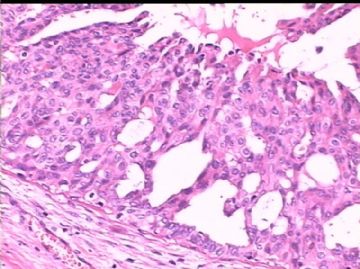
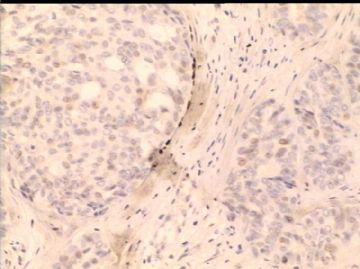
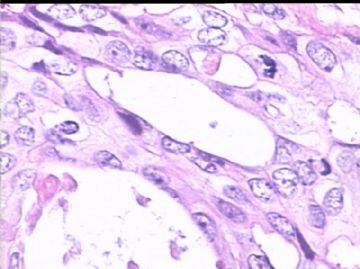
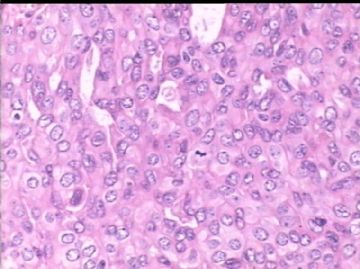
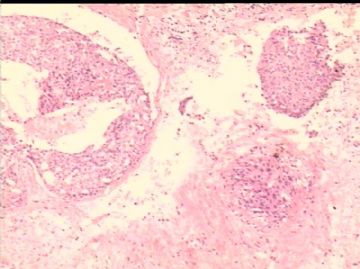
| 以下是引用青青子矜在2010-2-22 19:49:00的发言:
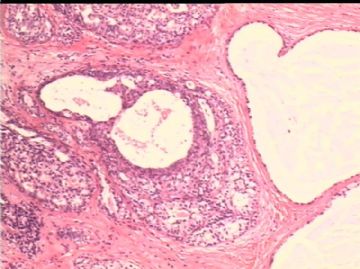
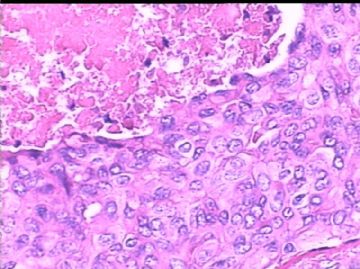
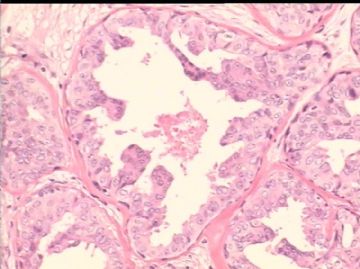
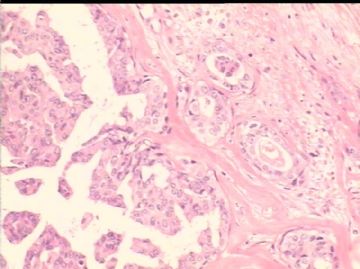
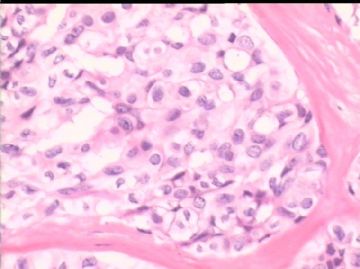
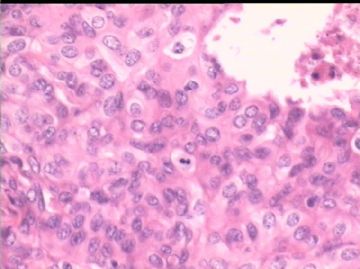
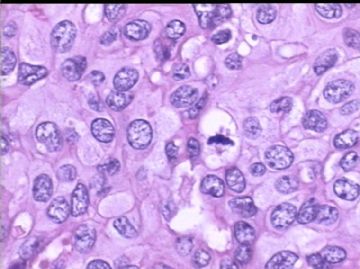
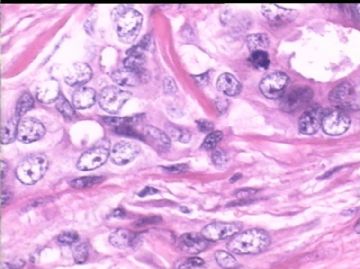
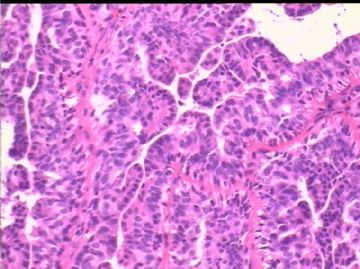
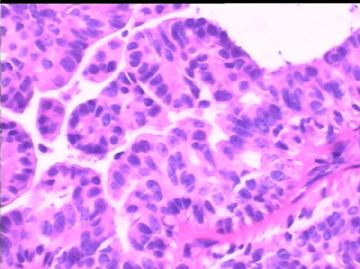
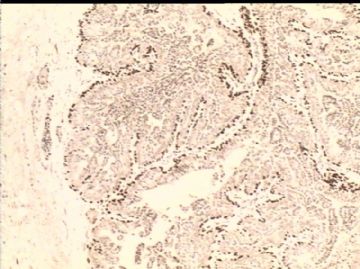
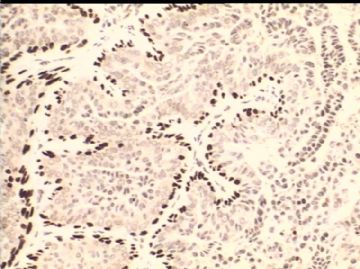
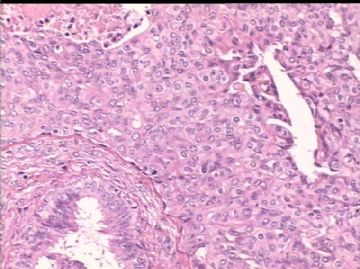
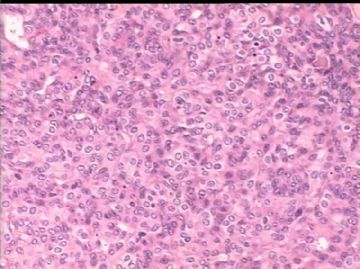
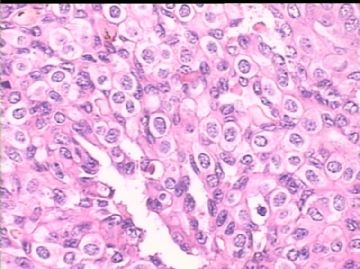
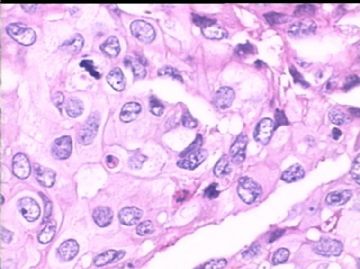
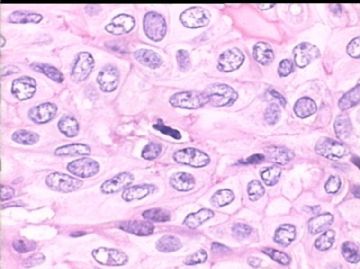
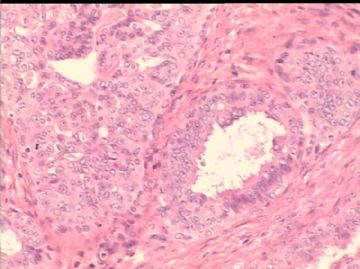
“如果这些病例显示典型的IHC结果,那H&E也很容易鉴别。”的确,我们在实际工作中也有相同体会。 刚发完以上,突然发现金教授的补充图片。 1、P63见增生上皮周围连续表达,至少这不是个浸润性癌; 2、SMA除了基底膜表达,部分区域见散在阳性肌上皮,另部分区域失表达呈单一性增生,至少有不典型增生; 3、不敢诊断DCIS。如果是DCIS,伴有中央性坏死至少是个中、高等级别DCIS,但细胞异型性不够。 4、希望补充CK5/6及ER/PR 请给我们讲讲乳头状瘤和乳头状癌的鉴别诊断(1)形态学和组织化学;2)免疫组织化学标记;(3)分子遗传学; 非常感谢! |

- xljin8
-
本帖最后由 于 2010-02-23 11:20:00 编辑
Reading true slides will be much easier for these kinds of cases.
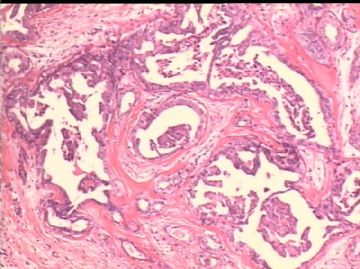
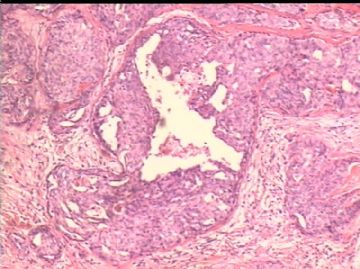
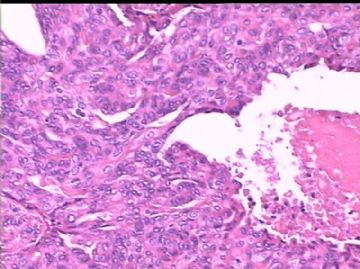
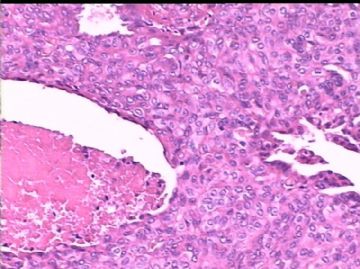
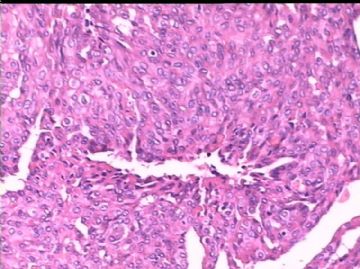
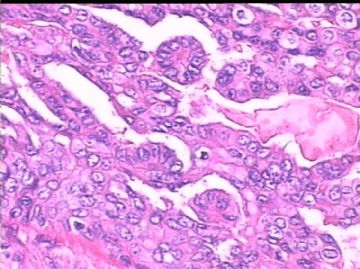
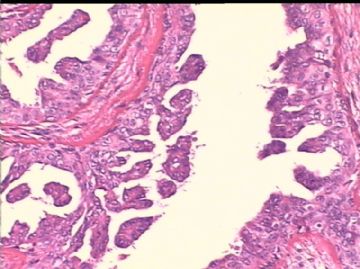
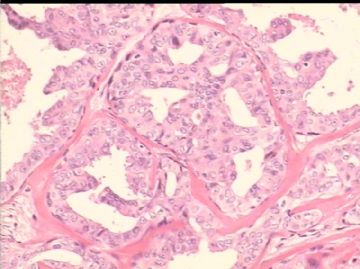
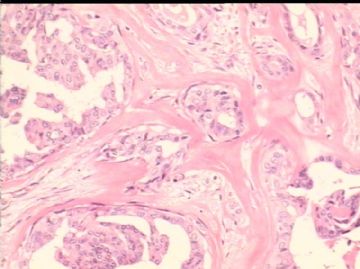
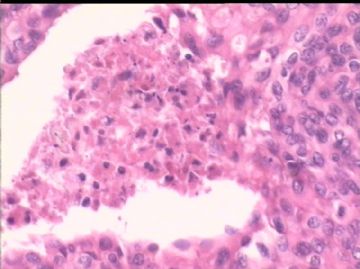
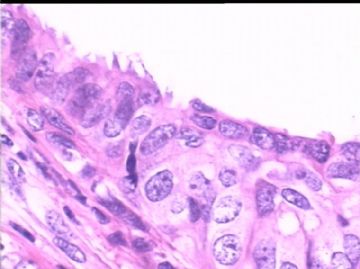
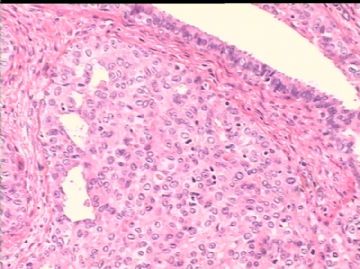
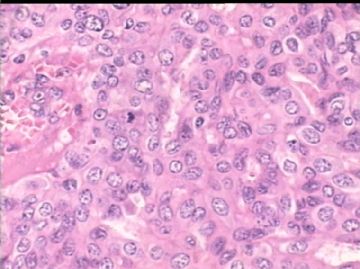
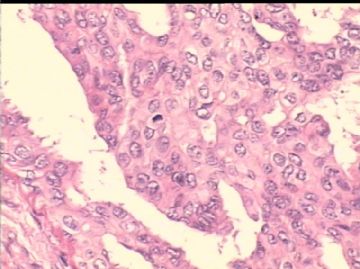
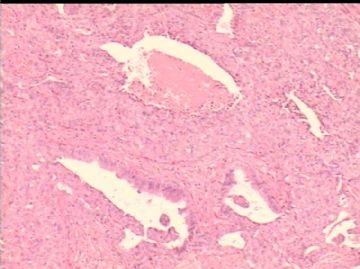
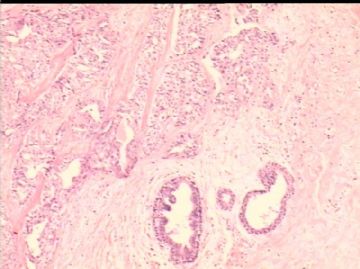
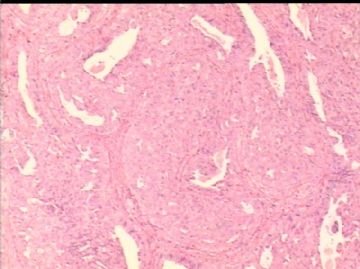
For papillary lesions, myoepithelial stains will be useful to demonstrate myoepithelail cells lining the fibrovascular cores are present or not. If all myoepithelial layer within the papillae are lost, it is a papillary DCIS. If florid ductal hyperplasia is present, you will not see the myoepithelial cells also.
The following photo may represent DCIS or UDH in term of IHC pattern. We still need H&E to make dx
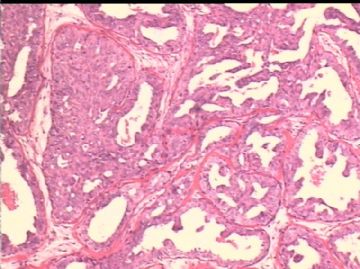
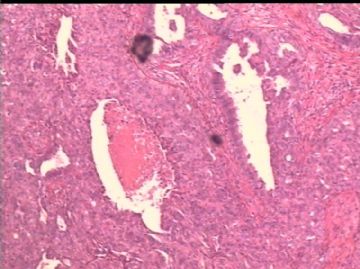
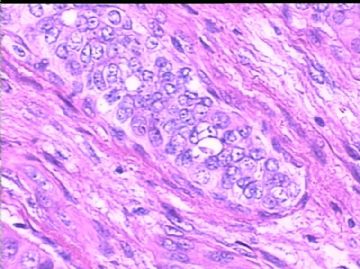
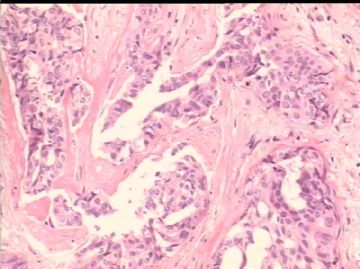
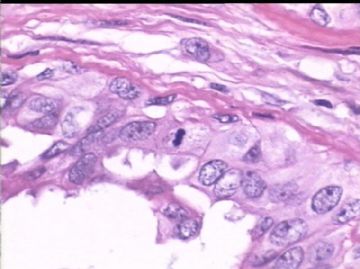
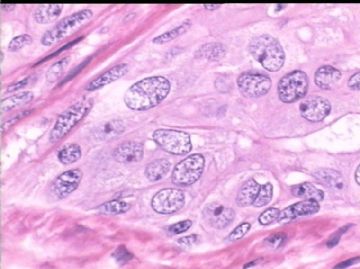
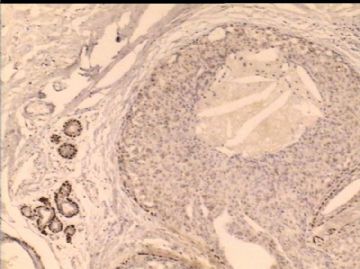
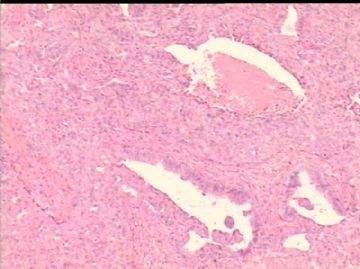
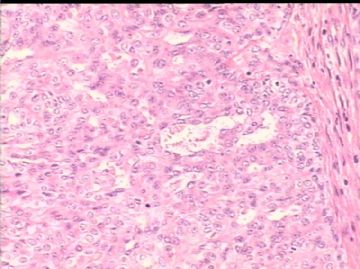
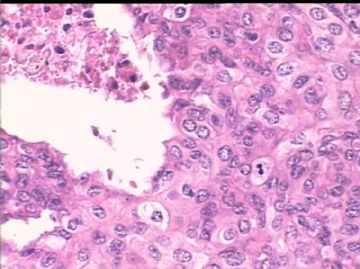
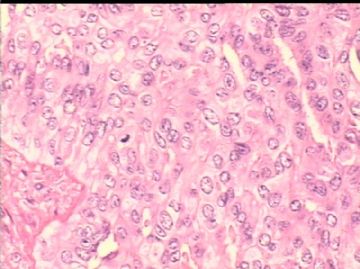
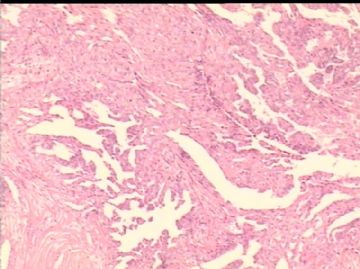
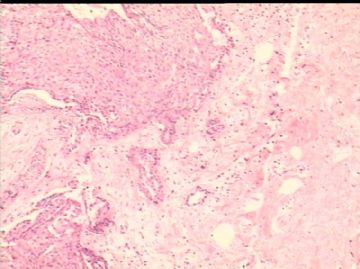
I cannot buy invasion so far. Need to see more.
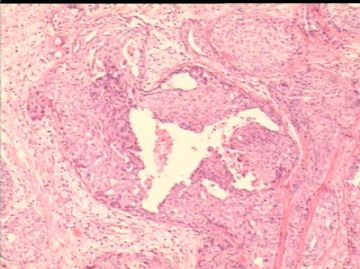
Solid papillary carcinoma: Generally all of the areas are solid tumor nodules. They are not present in the way focal benign papilloma and focal solid papillary ca.
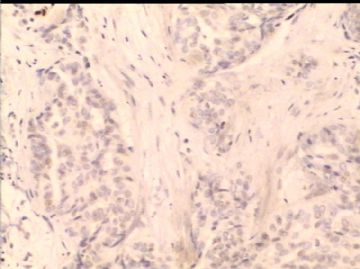
I increase my call now. Maybe it is case like DCIS involving papilloma.
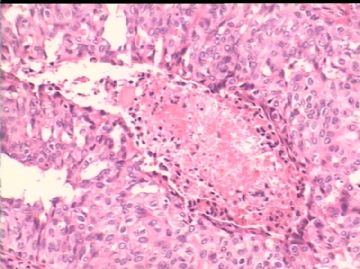
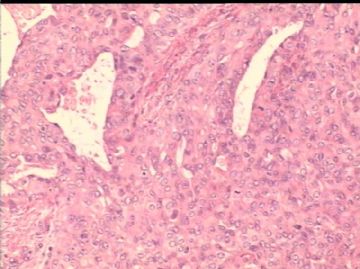
Origianlly it is a papillary lesion. Focal ducts keep proliferation-atypical -dcis. It is very arbitriary to divide atypical papilloma, DCIS involving papilloma, papillary carcinoma based on the % size involving by atypical proliferation. I feel it may be reasonable to call DCIS involving papilloma.
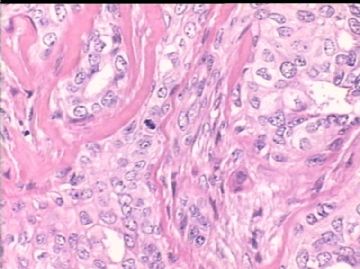
Invasive ca and DCIS are totally two different concepts. The prognosis and clinical management are different. We have to have very solid evidence to call invasion.
Till now I would not buy invasion. Of cause Dr. Jin will make his decision for his case. We are just talking and share no any responsibility. Ha, ha.
Again, thank Dr. Jin to share the case.
If all our Chinese pathologists have the 严谨的精神 as Dr. Jin, we will arrive the leading position in pathology area in the world.
cz
| 以下是引用海上明月在2010-2-22 6:11:00的发言:
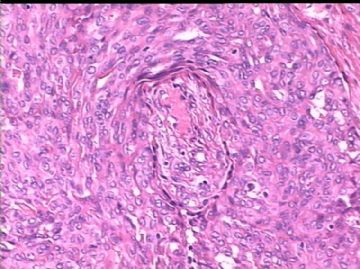
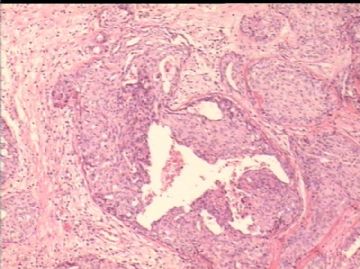
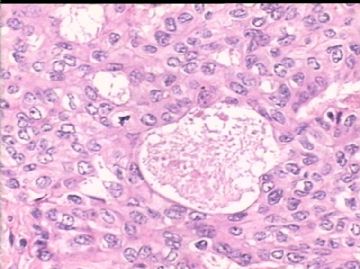
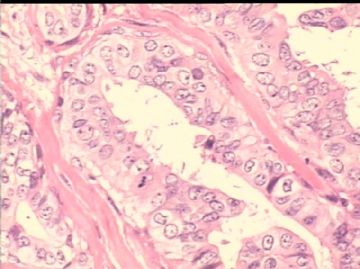
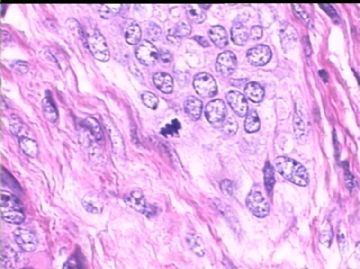
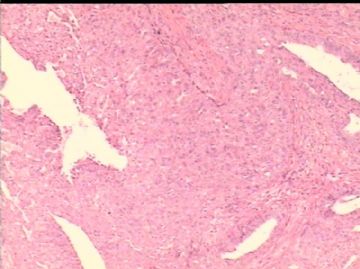
谢谢金主任出的好病例! 认为这是一个从中间到恶性的结构多样混杂的病例。有的酷似乳头状瘤,但却有肿瘤性坏死;有的酷似导管内癌,但却似有浸润(图7、8),甚至怀疑累及脉管(图24);有灶区酷似乳头状瘤(硬化型)。就是有的为导管内癌,也表现为不同亚型。导管内癌存在,浸润癌不能除外。需多个肌上皮标志物IHC辨别。也需要标记淋巴管血管等,鉴证浸润否。 |
很抱歉我引用了自己的发言。金老师的病例很精彩,Dr.Jin和Dr.Zhao两位老师的发言很精辟,向您们表示敬意。谢谢!
请允许我再次发言。
我反复仔细看过前后的HE切片,尤其是最后的一批图片,增加了对这个病例诊断的信心。这例可能性最大的诊断是:伴有显著原位癌成分的浸润性导管癌。
我想做的下一步工作是用IHC标记证明是否存在脉管(主要是淋巴管)受累。在没有IHC证实之前,不能放弃这个考虑。
还想知道有没有查腋窝淋巴结肿大的证据。谢谢!

- 王军臣