| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B1820乳房不典型血管瘤( cqz-20)
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
About 50 y/f breast core bx.
Immaging showed a 0.7x0.5 cm demarcated abnormal area.
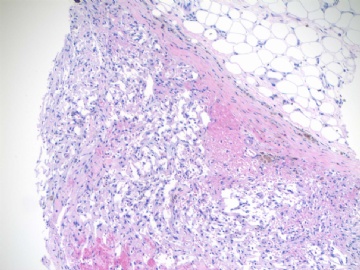
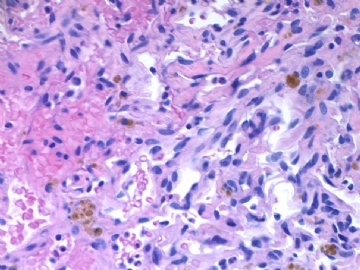
F1,100x, demostrating the margins
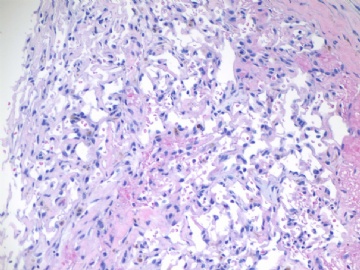
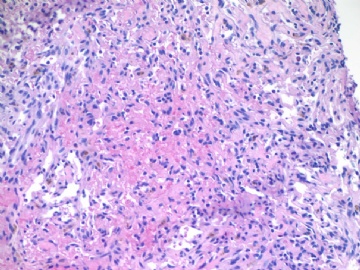
F2-3 200x
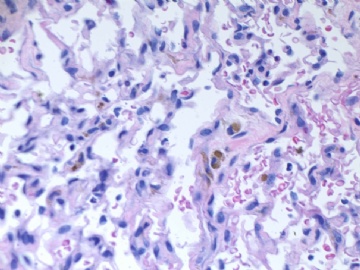
F4-5 400x
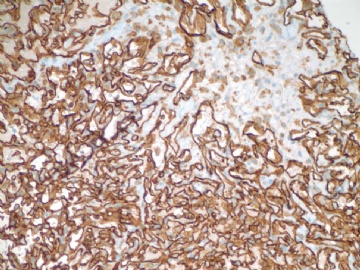
F6 CD31stain
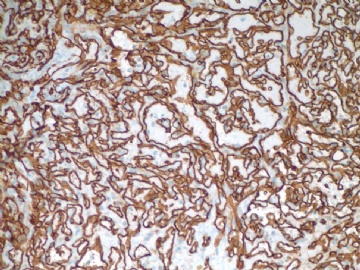
F7 CD34 stain
-
本帖最后由 于 2009-07-18 09:31:00 编辑
相关帖子
-
本帖最后由 于 2009-06-07 17:47:00 编辑
I remeber we had a breast vascular lesion case in this web with a lot of debatable discusion.
Above is a my case three weeks ago. Patient has no cancer or radiation history. She did have a breast core biopsy in the same breast two years ago. The diagosis was small papilloma and ducatal hyperplsia. I reviewed the previous breast core slides and agree with the interpretation. I called the radiologist to review the current and previous imaging films to confirm current lesion and the biopsy lesion two years ago were different areas. I felt difficult to sign out the breasst core biopsy case. Just wonder how you guys would sign out the case if it were yours.
I am on service for FNA on site evaluation for surgeons (several lung mass patients) this weekend. Now we are waiting for patient and I have time to send you this case. Enjoy your weekend
cz
quyibl译:
我记得网上有过一个存在很大争议的乳腺血管性病变的病例。
上面这个是我三周前的一个病例。病人没有乳腺癌或放射线照射史。两年前同侧乳腺做过活检,诊断是小的乳头状瘤伴导管增生。我复习了原先的乳腺活检切片,同意当时的诊断。我请放射科医师复验现在和原先的影像片,确定两次病变不在同一位置。我感到签出这个病例很困难,非常想知道如果这是你的病例,你会怎么签发这个报告。
这个周末, 我在为外科医生做现场的FNA(几个肺部包块的病人),现在正在等待病人,所以有时间发送给你们这个病例。 周末愉快!cz
The overall features still favour a benign vascular lesion. Dr Zhao, could you please give us an exact Ki67 count?
At this stage, I would sign out report like this: A vascular lesion with atypical features, favour a hemangioma. Complete excision of lesion with clear margins is recommanded.
Luckily, I cannot sign out report independently right now. But I really want to know, whether this report will cause trouble.
By the way, Dr Zhao, did you do pericytes stain? What do you think about the use of it in differentiating benign from malignant tumours?
| 以下是引用漫游人在2009-6-17 7:47:00的发言:
The overall features still favour a benign vascular lesion. Dr Zhao, could you please give us an exact Ki67 count? At this stage, I would sign out report like this: A vascular lesion with atypical features, favour a hemangioma. Complete excision of lesion with clear margins is recommanded. Luckily, I cannot sign out report independently right now. But I really want to know, whether this report will cause trouble. By the way, Dr Zhao, did you do pericytes stain? What do you think about the use of it in differentiating benign from malignant tumours? 总体特征仍然倾向良性血管性病变。赵博士,请你给出Ki-67精确值好吗? 在这种情况,我会这样发报告:伴有不典型特征的血管性病变,考虑血管瘤。建议完整手术切除。 幸运的是,我现在还不能独立发报告。但我很想知道我这样发报告有没有麻烦。顺便问一下赵博士,你做周细胞染色吗?你会考虑用它区分良性与恶性肿瘤吗? |
-
本帖最后由 于 2009-06-17 10:41:00 编辑
Thank you all for your input and Dr. Huang's translation.
To answer 漫游人:
I have never used pericyte stain. You can share your knowledge if you used the stain.
Ki67 positive cells should be <5%.
You said you cannot sign out case indipendently. Are you a reisident or fellow? I like your discussion a lot. You like an experienced pathologists.
Welcome to share your knowledge here.
Thank you Dr Zhao for your encouragement. If I were in China, I would be in the position of signing out report. I'm currently in overseas and trying to get through their training programe. I really liked your cases and the way you were presenting them. It's very educative.
I had my residence training in china that was very different from my current training and definately your training in America. We were trained to do spot diagnosis on almost any situation and were not used to give differential diagnosis on no matter a difficult case or a straight forward case. So if I didn't know an answer, i could not even give an alternative. Even today, I still have the problem sometimes.
I think the situation is better in major hospitals. I believe the general situation will improve gradually especially through this education platform.
-
本帖最后由 于 2009-06-09 21:45:00 编辑
Thank all discussion above. Very good. This is the way for discussion.
When we make a diagnosis we should consider the sample types. Generally our diagnosis will guide the next surgical procedure. The standard care is that the women should have total masterectomy if we call angiosarcoma.
To answer Dr. 漫游人 's question: The location of the lesion is 11 o'clock, parenchyma. You analysis is excelelnt.
Dr. Rosen's paper quyibl mentioned is a good one in term of benign or malignant breast vascular lesion.
I had ki67 stain. Will take a photo and paste here.
Welcome more people to share the oppinion. Thanks, cz
quyibl译:
谢谢上面精彩的讨论。这才是讨论的方式。
当我们做出一个诊断时我们应当考虑标本的类型。通常我们的诊断将指导下一步的外科手术方式。如果我们诊断血管肉瘤,标准的处理方式是这位女士做全乳腺切除。
回答“漫游人”医生的问题:肿块位于11点,乳腺实质内。你的分析很精彩。
Rosen的论文是一个不错的鉴别乳腺血管肿瘤良恶性的方法。我做了ki67的染色,会采集照片贴在这的。
欢迎更多的人参与讨论。谢谢,CZ。
-
本帖最后由 于 2009-07-08 22:40:00 编辑
http://www.ipathology.cn/forum/forum_display.asp?keyno=143381
Dr. wfbjwt had an interesting breast vascular lesion case above with a lot of discussion. You can compare the two cases for study purpose if you are interested.
abin译:
http://www.ipathology.cn/forum/forum_display.asp?keyno=143381
这个链接是Dr.wfbjwt提供的一例关于乳腺血管病变的有趣病例,有很多讨论。如果有兴趣,作为学习目的,你可以比较这两个病例。
We were trained to do spot diagnosis on almost any situation and were not used to give differential diagnosis on no matter a difficult case or a straight forward case. So if I didn't know an answer, i could not even give an alternative.
实话啊……
像我这样的刚入行的人遇到的最大的问题就是这个
一旦有疑难的
就老虎啃天了……

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Thank 漫游人's introduction.
I heard the spot diagnosis is for clinical patholgy, such as some blood work, urine exam. I never heard its usage in surgical patholog. Anatomic pathology related issues include frozen, on site evaluation in fine needle aspiration.
I am 孤陋寡闻. spot dx for surgical specimen is not easy, but you can get train well for your logic thinking.
Anyway, thank for share.
-
本帖最后由 于 2009-07-08 22:47:00 编辑
Ok. I am telling the story about this case.
Again I am gynecologic/breast pathologist and know a little about soft tissue tumors. I check a lot books and classic photos for vascular lesions when I had the case. The sections of the lesion demonstrate anastomosing vascular channels, endothelial cells nuclei with mild atypia and some with hyperchromatic. Solid and spindle cell foci are present. My cases are very similar to some of the angiosarcoma photos in Rosen breast book. I felt that it was an angiosarcoma case. I showed my case in our daily slide review conference. Our chief (about twenty hospitals in UPMC; all pathologist belong one large dept; we have one dept Chair; the haeds in pathology dept in each hospital are called chiefs or directors) and some pathologists agreed my angiosarcoma dx. My chief thought it was sarcoma without any question and would like to co-sign the case with me. I discussed the case with primary doctor of the patient and suggested the patient should see the breast sugeon. So I released the case as angiosarcoma-low grade with a long comment at 6 0'clock in the same day. We release case electronically in the computer. The related physicians will receive the pathology reports very quickly by automatical fax system when we release the case in computer. Also we cannot change the reports by ourselve after the cases were signed out.
njwbhuang译:
好了,我现在告诉你有关这个病例的故事
再次声明,我是一个妇科/乳腺病理医生,对软组织肿瘤知之甚少。当我遇到这个病例时,我查阅了许多书和典型图片。该病例切片显示有相互沟通的血管网,轻度不典型的内皮细胞核,部分细胞核深染。可见灶性实性和梭形细胞区域。我的病例非常相似于Rosen乳腺书中的一些血管肉瘤的图片。我认为这例应该是血管肉瘤,并将本例提交到科室每天病理读片会上。我们的主任(UPMC有20家医院,所有的病理医生属于一个大的病理科,我们有一个病理科主席,每个医院病理科的头子称为主任)和一些医生同意我的血管肉瘤的诊断。我的主任认为它是肉瘤没有问题,并且愿意与我一同签发这个报告。我与这个病人的初诊医生进行了沟通,建议这个病人应看乳腺外科医生。我在同一天6点签发了低级别血管肉瘤的病理报告,并写了一个较长的注解。我们在电脑上发报告。相关医生将很快通过自动传真系统收到病理报告。而且我们在报告发出后不能对报告进行修改。
-
似乎Ki67很有帮助,提供一些资料:
The Ki67-labeling index of angiosarcomas (mean, 38.1; median, 40.3) is substantially higher than the labeling index of hemangiomas (mean, 4.6; median, 1.7) (178). The labeling index of low-grade angiosarcomas (mean, 29.4; median, 24.5) is considerably less than the labeling indices for intermediate (mean, 41.6; median, 42.9) and high-grade angiosarcomas (mean, 44.8; median, 43.5).
The Ki67 immunostain is a useful adjunct in the diagnosis of the mammary hemangiomas. The nuclear Ki67 labelling index in mammary hemangiomas is very low, rarely exceeding 5%. Focally higher rates of labeling may be found in a hemangioma at sites of organizing thrombi or where a biopsy was previously performed on the lesion. Therefore, it is important to have an H&E-stained section available to visualize structural details when the Ki67 stain is being interpreted. The Ki67 labeling index of mammary angiosarcomas is greater than in hemangiomas, typically exceeding 20%, even in low-grade tumors. Because the distribution of labeling is not uniform in an angiosarcoma, it is possible by chance to obtain a small biopsy sample with less than 5% labelling from a low-grade angiosarcoma. A robust Ki67 labeling index on a needle core biopsy from a mammary vascular lesion would strongly favor angiosarcoma. Very sparse labelling in such a limited sample can assist in making a diagnosis of hemangioma when correlated with the H&E appearance of the lesion.
(From Rosen's Breast Pathology, 3rd Edition)
参考文献178同五楼:Shin SJ, Lesser MJ, Rosen PP. Hemangiomas and angiosarcomas of the breast: Diagnostic utility of cell cycle markers with emphasis on Ki-67. Arch Pathol Lab Med 2007;131:538–544.

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
-
本帖最后由 于 2009-07-08 22:44:00 编辑
| 以下是引用quyibl在2009-6-15 20:22:00的发言:
沉了,顶上来! KI67阳性率不超过5%,肿瘤大小0.7*0.5cm,无放射史。这些都不支持诊断恶性。没经验,搬个板凳学习中....等待老师的讲解。 |
Good. I am waiting you and others' final diagnosis.
Now you know all information for this pt. How would you sign out this case if it were your pt. Then I will tell you my report.
Of cause my report does not mean correct one.
abin译:
很好。我在等着你和别人的最终诊断。
现在你知道了患者的所有信息。如果是你的病例,你会怎样签发报告?然后我会告诉你,我是怎样签发的。
当然我的报告并不意味着一定正确。
-
本例CD31和CD34弥漫阳性,表明它是血管源性肿瘤。难点在于定性,良性/低度恶性?主要鉴别依据是Rosen的研究:
The nuclear Ki67 labelling index in mammary hemangiomas is very low, rarely exceeding 5%.
The Ki67 labeling index of mammary angiosarcomas is greater than in hemangiomas, typically exceeding 20%, even in low-grade tumors.
本例Ki67<5%,表明它是良性的血管肿瘤。这是一例我从未见过的少见的良性的乳腺血管肿瘤。
我们网站有另二例乳腺血管肿瘤:
http://www.ipathology.org.cn/forum/forum_display.asp?keyno=81946
http://www.ipathology.cn/forum/forum_display.asp?keyno=143381
谢谢Dr.Zhao的良苦用心。本例再次提醒我们,乳腺的血管病变的鉴别诊断包括很多种良性和恶性病变。
(抱歉的是,刚到新单位,没有上网条件)

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。