| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
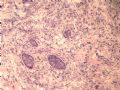
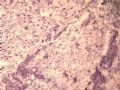
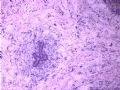
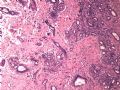
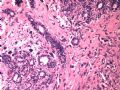
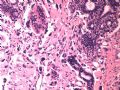
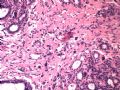
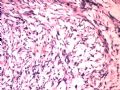
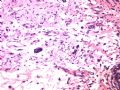
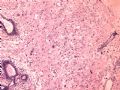
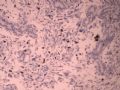
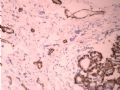
- B1614纤维腺瘤? 还是?
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
女 ,44岁,发现右乳房包块数日。大体:包块3.5×3.5×2.5cm,有完整被膜。
相关帖子
-
本帖最后由 于 2008-11-11 18:16:00 编辑
It looks benign. My impression is fibroadenoma with multinucleated giant stroma cells.
Please check original slides to see if there are mitoses of stroma cells, marked increased cellularity, the irregular edge.
abin译:
看上去是良性。我的印象是纤维腺瘤伴多核巨细胞。
请检查原切片,寻找是否有间质细胞核分裂,细胞密度明显增高和不规则边界。
-
stevenshen 离线
- 帖子:343
- 粉蓝豆:2
- 经验:343
- 注册时间:2008-06-03
- 加关注 | 发消息
-
本帖最后由 于 2008-11-11 18:18:00 编辑
These are frozen section slides. Diagnosis has to be conservative--differential include phyllodes, fibroadenoma with atypical stroma cells, sarcomatoid carcinoma; atypical cells look degenerative in nature; overall favor benign. Thanks.
abin译:
这些是冰冻切片,诊断应当相对保守些--鉴别诊断包括叶状肿瘤、纤维腺瘤伴不典型间质细胞,肉瘤样癌。不典型细胞看上去像退变性质,总体感觉良性。
谢谢。
-
liguoxia71 离线
- 帖子:4174
- 粉蓝豆:3122
- 经验:4677
- 注册时间:2007-04-01
- 加关注 | 发消息
-
shn-821128 离线
- 帖子:277
- 粉蓝豆:3
- 经验:277
- 注册时间:2008-11-02
- 加关注 | 发消息
-
Diagn Pathol. 2008 Aug 1;3:33
A diagnostic dilemma in breast pathology - benign fibroadenoma with multinucleated stromal giant cells.
Dept, of Surgery, Mayo General Hospital, Ireland. helenheneghan@hotmail.com.
ABSTRACT: Fibroadenomas are common benign breast tumours that display a characteristic pathological morphology, although several epithelial and stromal variations exist. A very rare histological finding is the presence of multinucleated giant cells throughout the stroma of a benign fibroadenoma. Cells of this type, which are more commonly found incidentally within the interlobular stroma of breast tissue, are benign and should not be mistaken for malignant cells on microscopic examination. Unfortunately a lack of awareness of this pathological entity can lead to diagnostic confusion amongst pathologists resulting in the multinucleate giant cells being mistaken for highly mitotic cells and consequently the fibroadenoma being mistaken for a malignant lesion. This may have serious implications for the subsequent management of the patient. The presence of this unusual cell type in the stroma does not alter the prognosis of otherwise benign lesion. We encountered two such cases at our institution in a six month period recently. We present their histories along with relevant radiological, microscopic and immunohistochemical features, followed by a discussion of this unusual pathological entity
Virchows Arch. 2001 Dec;439(6):768-75
Benign tumors of the breast with multinucleated stromal giant cells. Immunohistochemical analysis of six cases and review of the literature.
Department of Pathology, Charles University Medical Faculty Hospital, Hradec Králové, Czech Republic. ryskaale@fnhk.cz
The authors present six cases of benign tumors of the breast with numerous multinucleated stromal giant cells (MSGC). All six patients were women aged 37-70 years (mean 48 years), presenting clinically with a breast mass 1.0-3.8 cm in size (mean 1.9 cm; median 1.5 cm). By standard H&E examination, all cases showed the presence of numerous MSGC haphazardly dispersed within the tumor stroma. Three cases revealed MSGC merging into the surrounding adipose tissue simulating infiltrative growth. The MSGC appeared to have multiple nuclei (5 to 25) with fine chromatin and sporadic small nucleoli. Their cytoplasm was inconspicuous. The MSGC expressed vimentin only and to lesser extent CD34. These cells were negative for muscle markers, keratins, S-100 protein, vascular markers, CD68 and hormone receptors. Interestingly, the majority of MSGC and mononuclear stromal cells showed reactivity for p53 protein and Ki-67 proliferation antigen. All patients were treated by simple excision and remain free of recurrence (mean 70 months, median 48 months.). The reactivity of p53 in MSGC and mononuclear stromal cells may play a key role in linking these two cell types. Nonetheless, the presence of MSGC does not alter prognosis of otherwise typical benign lesions.
The lesions were described more than 20 years ago.
Am J Surg Pathol. 1986 Nov;10(11):823-7
Mammary fibroadenoma with multinucleated stromal giant cells.
We have studied an otherwise typical mammary fibroadenoma in a 42-year-old female in which numerous, bizarre, mitotically inactive, multinucleated giant cells were present throughout the stroma. Immunohistochemical and ultrastructural studies confirmed the mesenchymal, specifically fibroblastic, nature of the giant cells. Cells of this type, which are more commonly an incidental finding within the interlobular stroma of the breast, are benign, and should not be mistaken for malignant cells on microscopic examination.