| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B1820乳房不典型血管瘤( cqz-20)
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
About 50 y/f breast core bx.
Immaging showed a 0.7x0.5 cm demarcated abnormal area.
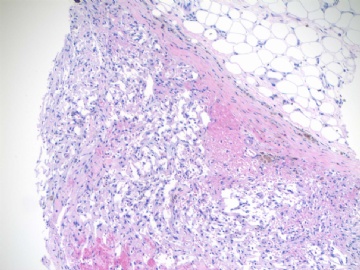
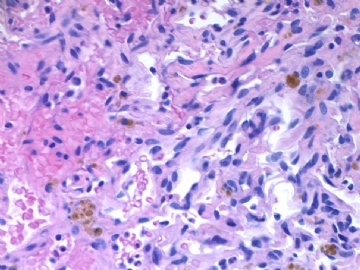
F1,100x, demostrating the margins
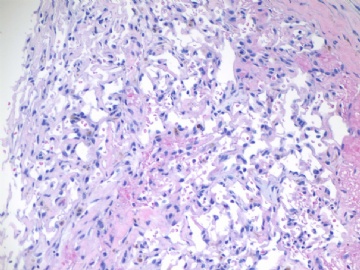
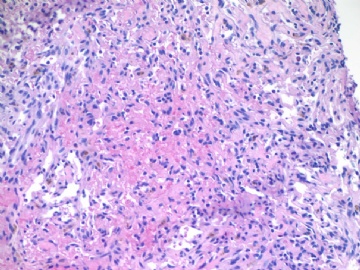
F2-3 200x
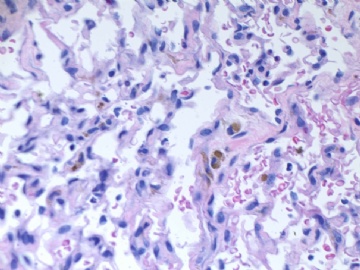
F4-5 400x
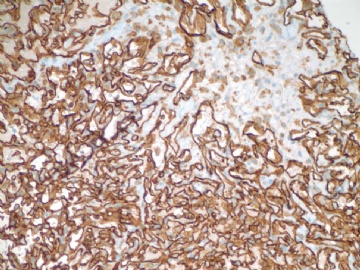
F6 CD31stain
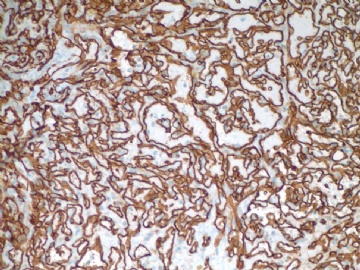
F7 CD34 stain
-
本帖最后由 于 2009-07-18 09:31:00 编辑
相关帖子
I am in research this week and have time to review all people's discussion this morning. Thank Drs Huang, Abin, and Quyibl for your great translation, and all of people who joined the discussion and review in this subject.
From the publications (see above) of Dr. Rosen and Sharon Wess, world-famous soft tissue experts (of cause it does not mean what they mentioned are always right), we know the basic fact that the term of atypical vascular lesions in breast is accepted among pathologists world-wild.
Why do we discuss some cases in the web? The only reason is to share with others or to learn from others. If I signed out my true cases for malignant I do not care others in the internet to call bengin or malignant. It is the same you signed your cases as benign or maligant, you do not need to care some people in the internet to have the different diagnosis. When you sign your cases and release the reports, you have the responsiblity for your professonal job, patients, families, and hospitals, but others in the internet have not any responsibility.
Frankly speaking I will not agree to co-sign any case in the true world based on a few photos in the internet.
Ki67: Based on Rosen' paper published in 1992 ki67 seems to have some meaning for distinguishment of some breast vascular lesions, especially for benign vs. atypical vascular lesions or atypical lesions vs. low grade hemagiosarcoma. However it may be no use for some classic angiosarcoma even for typical low grade angiosarcoma.
In fact I asked Dr. Christoper Fletcher, Director of surgical pathology, Brigham and Women's Hospital, Harvard Medical School (famous soft tissue pathologist), about his oppinion about ki67 in the dx of breast vascular lesions. He said they never use ki67 for breast vascular lesions in Brigham and Women's Hospital.
Ok, I complete this topic and final discussion.
Thank all of you again. cz
-
jianshu322 离线
- 帖子:447
- 粉蓝豆:17
- 经验:1405
- 注册时间:2008-12-22
- 加关注 | 发消息
-
本帖最后由 于 2009-07-18 20:22:00 编辑
Above is the full report and comment in this case. You can use as your reference in your daily case.
What did I learn from this case? be cautious when you sign out your cases especially for some difficult case. Always think what procedure the clinicians will do next based on our pathology dx.
I feel very happy I changed my breast core biopsy dx from angiosarcoma to atypical vascular lesion. If I called angiosarcoma in core bx, patient would have mastectomy, instead of segment mastectomy. I will feel bad for myself and also for the patient. This may be a law-suit case due to my over call in core bx.
Wish every one knows that our pathology jobs are important, great, but dangerous.
以上是本例的完整报告。你可以在日常工作中作为参考。
我从本例中学到什么?签发报告要小心,尤其是一些疑难病例。总是要考虑到,根据你的报告,临床将会如何处理。
我很高兴,把乳腺粗针穿刺活检的报告从血管肉瘤改成了不典型血管病变。如果我在粗针活检时报血管肉瘤,患者将要切除乳房,而不是乳腺区段切除。我会对自己也对患者感到不爽。这也可能因为我在粗针活检时的过诊断而成为诉讼病例。
希望所有人知道,我们病理工作重要、伟大,但危险。(abin译)
-
本帖最后由 于 2009-07-18 17:33:00 编辑
My collequre released the case as:
A. Atypical hemangioma.
B. Mass measures 5 mm.
C. Surgical margins are negative for the tumor; closest margin is 7 mm from the tumor.
D. Surrounding breast tissue showing sclerosing adenosis and lactational-type change.
E. Biopsy site change.
F. Skin, negative for neoplasm.
Comment:
This atypical vascular lesion is well circumscribed and demonstrates no infiltration into surrounding breast parenchyma. Although cytologic atypia is present, mitotic activity is not evident and a stain for Ki67 does not show increased staining beyond what could be expected in the setting of prvious biopsy and fibrin thrombi. Clinical experience with this entity is limited, but at least one study deminstrated benign clinical behavior following excional biopsy (reference: Am J Surg Pathol, 1992, 16(6):553-560).
Previous core biopsy diagnosis of atypical vascular lesion is noted and the slides were reviewed (case No xxxx).
Dr. XXXXX has reviewed the representative slides and agrees with above interpretaiton.
The case was discussed with surgeon Dr. xxxx at xx o'clock on month/day/2009.
abin译:
本例,我的同事签发的报告如下:
A.不典型血管瘤。
B.肿块大小5mm。
C.手术切缘阴性,肿瘤距最近切缘7mm。
D.周围乳腺组织呈硬化性腺病和泌乳性改变》。
E.活检后改变。
F.皮肤无肿瘤。
注:
这个不典型血管病变界限清楚,未见浸润周围乳腺间质。尽管有细胞学不典型性,但核分裂活性不明显,且除以前活检部位和血栓周围外,Ki67染色并不增高。对本病变的临床经验有限,但至少有一个研究表现了切除活栓后呈良性的临床行为(reference: Am J Surg Pathol, 1992, 16(6):553-560)。
注意到以前的粗针活检诊断为不典型血管病变,并复习了原切片(病例号XXXX)。
Dr. XXXXX复习了切片并同意以上分析。
本例与外科医生Dr. xxxx讨论过(年月日时……)。
Dr. bzlixinjun and abin's interpretation is excellent. Thank you. Just wonder if Dr bzlixinjun is working in China or other countries.
-
bzlixinjun 离线
- 帖子:63
- 粉蓝豆:23
- 经验:64
- 注册时间:2007-10-28
- 加关注 | 发消息
-
本帖最后由 于 2009-07-12 23:24:00 编辑
Focally higher rates of labeling may be found in a hemangioma at sites of organizing thrombi or where a biopsy was previously performed on the lesion.(Rosen's Breast Pathology ,3ed).This case had a breast core biopsy, so high area of Ki-67 index can be able to interpret. Moreover ,complete capsule and very small lesion all suggested benign outcome. We also see the complex structure and atypical nuclear after all. A diagnois of atypical vascular lesions may be appropriate to this case. And a follow-up is essential.
abin译:
Ki67标记表现为局灶较高的核增殖指数,可见于一些血管瘤的机化血栓局部,或者以前做过活检的部位(Rosen's Breast Pathology ,3ed)。本例做过粗针穿刺活检,因此存在Ki-67高指数区也就可以解释了。而且,病变有完整包膜,非常小,也提示为良性过程。然而我们也能看到复杂结构和不典型核。本例诊断为不典型血管病变也许比较合适,并且,随访也很重要。