| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B1820乳房不典型血管瘤( cqz-20)
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
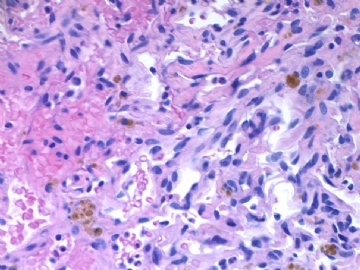
About 50 y/f breast core bx.
Immaging showed a 0.7x0.5 cm demarcated abnormal area.
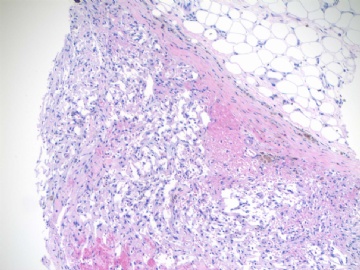
F1,100x, demostrating the margins
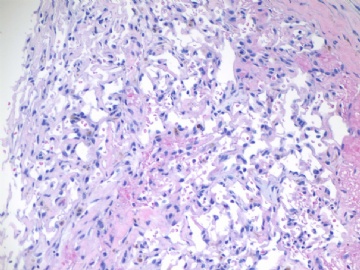
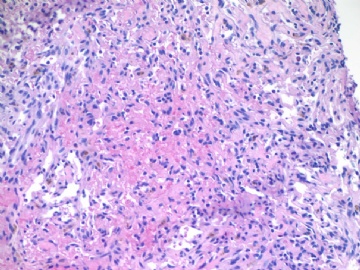
F2-3 200x
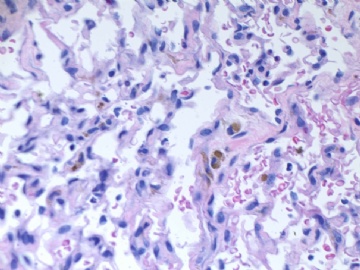
F4-5 400x
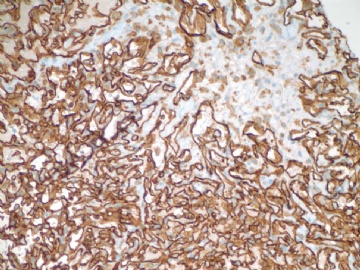
F6 CD31stain
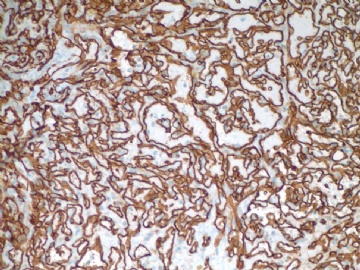
F7 CD34 stain
-
本帖最后由 于 2009-07-18 09:31:00 编辑
相关帖子
-
本帖最后由 于 2009-07-08 23:00:00 编辑
Diagn Cytopathol. 2001 Mar;24(3):215-8.
-
Atypical hemangioma of the breast: a diagnostic pitfall in breast fine-needle aspiration.
Department of Pathology and Laboratory Medicine, Hahnemann University Hospital, MCP Hahnemann University, Philadelphia, Pennsylvania 19102, USA.
We report on the fine-needle aspiration (FNA) cytology of atypical hemangioma of the breast in a 52-yr-old female. The patient presented with a 2-cm palpable left breast mass. An FNA of the mass was performed following a mammogram, corresponding to the palpable breast mass. The FNA demonstrated the presence of numerous atypical single spindle cells scattered throughout a hemorrhagic background. An unequivocal diagnosis of malignancy was not rendered in this case. However, the degree of cytologic atypia suggested a malignant process, and a recommendation for an excisional biopsy was made. Atypical hemangioma should therefore be included in the differential diagnosis of angiosarcoma and other benign and malignant spindle-cell lesions of the breast encountered on cytologic samples.
njwbhuang译:
乳腺不典型血管瘤:乳腺细针吸取诊断中的缺陷
我们报道了1例发生于52岁女性乳腺的不典型血管瘤的细针吸取细胞学(FNA)检查。病人表现为左侧乳腺2cm的可触及的肿块。在行乳腺X线摄影检查术后进行了肿块的FNA。FNA证实了多量不典型单个梭形细胞散在于出血性背景中。对这个病例没有做出明确的恶性诊断。然而,细胞学不典型程度提示恶性过程,建议肿块切除活检。不典型血管瘤因此应包括在血管肉瘤的鉴别诊断中,在细胞学标本中可遇到其他乳腺良性和恶性梭形细胞病变。
-
本帖最后由 于 2009-07-08 22:59:00 编辑
Breast. 2002 Aug;11(4):357-8.
-
Breast hemangioma mimicking carcinoma.
Department of Radiology, Hospital Universitari Germans Trias i Pujol, Badalona, Spain. mariscal@ns.hugtip.scs.es
Breast hemangiomas are rare, and usually appear as well-delimited round or oval nodules at mammography. We report a case of a woman with a breast hemangioma, which mammographic features simulated malignancy, and present its pathologic correlation. Hemangiomas are benign vascular tumors that are rarely present in the breast, usually found incidentally on microscopy of biopsy material for other. They are occasionally detected by mammography, presenting as well-delimited round, lobulated nodules, sometimes with calcifications. We present the mammographic findings and pathologic correlation in a case of breast hemangioma with an atypical radiological manifestation, simulating a carcinoma. To our knowledge, this is the first reported case with these radiologic characteristics.
njwbhuang译:
类似于癌的乳腺血管瘤
乳腺血管瘤非常罕见,乳腺摄影上通常表现为境界清楚的圆形或卵圆形结节。我们报道了1例乳腺血管瘤,乳腺摄影特征像恶性,并提供了其病理学特征。血管瘤是良性血管性肿瘤,发生于乳腺比较罕见,通常因其他病变而活检的材料上镜下偶然发现。他们偶在乳房x线摄影术上偶然发现,表现为境界清楚圆形、分叶状结节,有时伴有钙化。我们介绍了1例有不典型放射学特征,类似于癌的乳腺血管瘤的乳房x线摄影术发现和病理特征。据我们所知,这是首例伴有这些放射学特征的乳腺血管瘤病例报道。
-
本帖最后由 于 2009-07-08 22:59:00 编辑
Eur J Gynaecol Oncol. 2004;25(3):324-6.
-
Clinicopathological study of vascular tumors of the breast: a series of ten patients with a long follow-up.
Pathology Laboratory, Areteion Hospital, Athens, Greece.
Ten cases of vascular tumors of the breast were examined in our laboratory during the last decade (1992-2001). Nine patients were female and one male (ages 31-77, average 52 years). Six patients presented parenchymal vascular lesions (1 angiosarcoma, 1 atypical hemangioma, 3 perilobular hemangiomas, 1 cavernous hemangioma) measuring 0.5-6 cm in the greatest diameter. Two lesions were accidental findings in lumpectomy specimens excised for fibrocystic disease with microcalcifications. Four patients presented non-parenchymal vascular lesions: three cavermous hemangiomas (one in a male patient) and one angiolipoma measuring 1-6 cm in diameter. All tumors were treated by lumpectomy with the exception of the atypical hemangioma which was treated by simple mastectomy. The patient with the angiosarcoma was treated by simple mastectomy, radiotherapy and chemotherapy and died with disseminated disease three years after initial diagnosis. All other patients are well up to date (follow-up 1-9 years).
njwbhuang译:
乳腺血管性肿瘤临床病理分析:10例系列报道伴长期随访
1992-2001年间我们共遇到10例乳腺血管性肿瘤。女性9例,男性1例(年龄31-77岁,平均52岁)。6例表现为实质血管性病变(血管肉瘤1例,不典型血管瘤1例,小叶周围血管瘤3例,海绵状血管瘤1例),大小0.5-6cm。2例因乳腺纤维囊型病变伴微钙化在切除的标本上偶然发现。4例呈非实质性的血管病变,其中海绵状血管瘤3例(1例为男性),1例为血管脂肪瘤,最大直径为1.6cm。除了不典型血管瘤性单纯型乳腺切除术外,所有肿瘤均行肿块切除术。血管肉瘤病人行单纯性乳腺切除术、放疗和化疗,在初次诊断后3年死于全身扩散。所有其他病人随访到现在均无异常(随访时间1-9年)。
-
本帖最后由 于 2009-07-08 22:58:00 编辑
Histopathology. 2008 Jan;52(1):30-44.
-
Vascular proliferations of the breast.
Department of Histopathology, University College Hospital, Galway, Ireland. cmbrodie@gmail.com
Vascular proliferations of the breast are uncommon but potentially diagnostically challenging lesions. Clinically apparent processes are more likely to be malignant; however, a range of benign entities which must be differentiated from angiosarcoma also exists. This review discusses first, breast lesions of apparent vascular origin, then benign and histologically bland perilobular, cavernous and capillary haemangiomas. Subsequently, more diagnostically challenging, atypical haemangiomas, papillary endothelial hyperplasia, angiomatosis and angiolymphoid hyperplasia with eosinophilia (epithelioid haemangioma) are considered. In addition, lesions with low-grade malignant potential such as haemangiopericytomas and epithelioid haemangioendotheliomas may rarely present in the breast. However, primary angiosarcomas and radiation-associated vascular lesions are reviewed in depth, as these entities are of greatest clinical and pathological significance.
njwbhuang译:
乳腺的血管增生性病变
乳腺的血管性增生虽然少见,但有可能是在诊断上具有挑战性。临床上表现明显进程的多可能是恶性的,然而一些应与血管肉瘤区分的良性病变也可存在。这篇综述首先讨论了乳腺明显的血管来源的病变,然后介绍了良性和组织学温和的小叶周围、海绵状和毛细血管瘤。接着综述了诊断具有挑战性的病变如不典型血管瘤、乳头状内皮增生、血管瘤并和伴有嗜酸细胞浸润的血管淋巴样增生(上皮样血管瘤)。另外,罕见的低级别恶性潜能型病变如血管外皮细胞瘤和上皮样血管内皮细胞瘤可发生于乳腺。然而,原发性血管肉瘤和放射相关的血管性病变更进一步复习,因为这些疾病具有重要的临床和病理意义。
-
本帖最后由 于 2009-07-08 22:53:00 编辑
-
Department of Pathology, Memorial Sloan-Kettering Cancer Center, New York, New York 10021.
Eighteen patients with vascular tumors of the breast that exhibited characteristics raising the question of but not qualifying for a diagnosis of low-grade angiosarcoma were reviewed. We had previously referred to these lesions as "atypical" hemangiomas because of concern regarding the diagnosis and the risk of the later development of angiosarcoma. Significant features, variably present, included small size (less than 2.0 cm), relative circumscription, broadly anastomosing vascular channels, and endothelial hyperplasia. Destructive invasion, solid areas, and hemorrhage or necrosis unrelated to a needle localization procedure were absent. Four distinct histological patterns were observed: cavernous, compact capillary, capillary budding, and a combined cavernous and compact capillary type. The age of the patients varied from 19 to 82 years (mean 60 years). Eleven tumors were detected mammographically. The size of the lesion ranged from 0.4 to 2.0 (mean 0.9) cm. The diagnostic biopsy was the only treatment in nine (50%) cases. Reexcision was performed in seven and mastectomy was done in two cases. Follow-up ranged from 1 to 140 (mean 44) months. There have been no local or systemic recurrences. Hemangiomas with diverse histological patterns have been detected clinically with the increasingly widespread use of mammography. Further follow-up indicates that the lesions originally referred to as "atypical" are benign and not associated with an appreciable risk of the development of angiosarcoma. Complete excision alone is recommended to treat these tumors, which may be diagnosed as hemangiomas and subclassified according to growth pattern
njwbhuang译:
伴有不典型组织学特征的乳腺血管瘤:证实它们良性特征的组织学亚型的进一步分析
对18例组织学形态显示有疑问但未符合低级别血管肉瘤诊断的乳腺血管性肿瘤进行复习。由于担心这个诊断和以后发展成血管肉瘤的风险,我们以前将这些病变称为“不典型”血管瘤。有意义的组织学特征如病变小(不到2.0cm)、相对境界清楚、广泛相互沟通的血管网和内皮细胞增生等不同程度存在,而破坏性浸润、实性区域,与穿刺无关的出血或坏死均未见。可有4种独特的组织学构型:海绵状、致密毛细血管、毛细血管芽和复合性海绵状和致密毛细血管型。病人年龄19-82岁(平均60岁)。11个病例行乳腺摄影检查。病变大小从0.4到2.0cm(平均0.9cm)。9例(50%)行诊断活检并作为唯一治疗方法。7例行肿块再次切除,2例行乳腺切除术。随访时间1到140月(平均44月)。没有局部或全身复发。随着乳腺摄影逐渐广泛使用,伴不同组织学构型的血管瘤临床上检出率增加。深入随访显示当初称为“不典型”的这些病变是良性,与发展成血管肉瘤的已知的风险无关。这些肿瘤可诊断为血管瘤和根据生长构型而确定的亚分类,并建议将肿块单独完整切除。
Am J Surg Pathol. 1992 Jun;16(6):553-60.
Hemangiomas of the breast with atypical histological features. Further analysis of histological subtypes confirming their benign character.
-
本帖最后由 于 2009-07-08 22:51:00 编辑
I discussed and convinced my chief. I went to the quality control office to ask the person to change my diagnosis (all changes of pathology report must be made by them). I called the primary physician again to notice the change of the report and the reasons. Finally I released the changed dx report----Atypical vascular lesion with a long comment, excisional biopsy suggested for definitive dx.
I feel good to call atypical vascular lesion for this core biopsy case. If it is a sarcoma by excisional bx pt can have mastectomy in next procedure. If it is still borderline lesion in excisional bx, the pt can avoid total mastectomy.
What lessions I have learned from this case (also suggestion to young pathologists in China):
1. Think over for some difficult case, especially for the subspecielty you are not famililar. Do not rush yourself. Keep one day and you may have different oppinion for your case in the second day.
2. You must be 100% sure or agree the dx before you release your cases. No matter what other people say, your chief, your chair, consulting exports. You will take the responsibility when your name is prsent in the pathology report.
3. Consider the possible follow-up procedures the clinicians will take when you make your dx.
If this were a mastectomy case, I will send the case to soft tissue expert pathologists for the second oppinion.
Ok, I think I complete the presentation and discussion for this case. Thank all of you for reading and discussing for this case.
cz
njwbhuang译:
我与主任讨论并是他信服了。我去质控办公室请一个人帮我改变我的病理诊断(所有病理报告修改必须由他们完成)。我再次打电话给初诊医生,提醒他我们修改了病理诊断并说明了理由。最后我签发了一个修改的病理报告——不典型血管性病变,并有一个长的注解,建议切开活检以明确诊断。我对这例粗针活检病例称为不典型血管病变比较满意。如果切开活检证实为肉瘤,病人ke 下一步进行乳腺切除术。如果仍然是交界性病变,那病人可免除乳腺全切除术。
从这个病例我吸取的教训是(也是对中国年轻医师的建议):
1.认真考虑一些疑难病例,特别是你不熟悉的亚专业病例。发报告不要急,保留一天,第二天你可能有不同的意见。
2.在发报告前你必须有100%把握或同意你的诊断。无论什么人如科主任、主席、会诊转接等告诉你什么,你要对病理报告中你的名字负责。
3.当你做出诊断时,你要想到临床医生将要可能采取的措施。如这个病例是乳腺部分切除,我将把这个病例送到软组织病理医生那里,看看他们的诊断。
好了,我想我完成了这个病例的介绍和讨论。谢谢所有参与这个病理的讨论者。
-
本帖最后由 于 2009-07-08 22:49:00 编辑
I felt happy to fisnished one day's work and would go home at that day. I told another pathologist that i just released the case with co-signature of the chief. He said he was not sure of this case and he would not like to co-sign this case with him. I caould not sleep well that night due to this case and my collegure's concern. If the core bx was diagnosed as angiosarcoma the patient should have a total mastectomy by the standard care. In the second day I came to the office very early and ordered some IHC including ki67. I checked the literature and read several related papers including Rosen's paper Drs. quyibal and abin mentioned above. I also called radiologist to review the x-film to confirm the size of the lesion (0.7 cm, with no infiltration). I got the IHC 3'0'clock in the same day and noticed very low ki67 proliferative index of the tumor. I though over this case. It is true that the morphologic features of the case look like a low grade angiosarcoma. However the facts aginst the dx included small lesion, demarcated margin, very low ki67 positivity.
I need to do sth now and will come back to finish the story later.
njwbhuang译:
我很高兴地完成了一天的工作并准备回家。我告诉另一个医生,我刚刚和主任共同签发了这个病例的病理报告。他说他对这个病例不太确信,他可能不会与主任共同发这个报告。由于这个病例和同事的话,我那天晚上无法入睡。如果粗针活检诊断为血管肉瘤,病人将进行全乳房切除术。第二天我非常早地来到办公室并做了一些免疫标记包括Ki-67。我查阅了一些文献并看了一些相关的文章包括quyibal和abin上面提到的Rosen的文章。我也请放射科医生看了X光片证实病变大小(0.7cm,没有浸润)。同一天3点钟我拿到了免疫组化切片,注意到Ki-67增殖指数非常低。我反复考虑这个病例。形态学上的确像低级别血管肉瘤,然而不支持该诊断的是病变小,境界清楚,非常低的Ki-67增殖指数。我现在需要做一些事情,以后再回来完成这个故事。
-
本帖最后由 于 2009-07-08 22:47:00 编辑
Ok. I am telling the story about this case.
Again I am gynecologic/breast pathologist and know a little about soft tissue tumors. I check a lot books and classic photos for vascular lesions when I had the case. The sections of the lesion demonstrate anastomosing vascular channels, endothelial cells nuclei with mild atypia and some with hyperchromatic. Solid and spindle cell foci are present. My cases are very similar to some of the angiosarcoma photos in Rosen breast book. I felt that it was an angiosarcoma case. I showed my case in our daily slide review conference. Our chief (about twenty hospitals in UPMC; all pathologist belong one large dept; we have one dept Chair; the haeds in pathology dept in each hospital are called chiefs or directors) and some pathologists agreed my angiosarcoma dx. My chief thought it was sarcoma without any question and would like to co-sign the case with me. I discussed the case with primary doctor of the patient and suggested the patient should see the breast sugeon. So I released the case as angiosarcoma-low grade with a long comment at 6 0'clock in the same day. We release case electronically in the computer. The related physicians will receive the pathology reports very quickly by automatical fax system when we release the case in computer. Also we cannot change the reports by ourselve after the cases were signed out.
njwbhuang译:
好了,我现在告诉你有关这个病例的故事
再次声明,我是一个妇科/乳腺病理医生,对软组织肿瘤知之甚少。当我遇到这个病例时,我查阅了许多书和典型图片。该病例切片显示有相互沟通的血管网,轻度不典型的内皮细胞核,部分细胞核深染。可见灶性实性和梭形细胞区域。我的病例非常相似于Rosen乳腺书中的一些血管肉瘤的图片。我认为这例应该是血管肉瘤,并将本例提交到科室每天病理读片会上。我们的主任(UPMC有20家医院,所有的病理医生属于一个大的病理科,我们有一个病理科主席,每个医院病理科的头子称为主任)和一些医生同意我的血管肉瘤的诊断。我的主任认为它是肉瘤没有问题,并且愿意与我一同签发这个报告。我与这个病人的初诊医生进行了沟通,建议这个病人应看乳腺外科医生。我在同一天6点签发了低级别血管肉瘤的病理报告,并写了一个较长的注解。我们在电脑上发报告。相关医生将很快通过自动传真系统收到病理报告。而且我们在报告发出后不能对报告进行修改。
Thank 漫游人's introduction.
I heard the spot diagnosis is for clinical patholgy, such as some blood work, urine exam. I never heard its usage in surgical patholog. Anatomic pathology related issues include frozen, on site evaluation in fine needle aspiration.
I am 孤陋寡闻. spot dx for surgical specimen is not easy, but you can get train well for your logic thinking.
Anyway, thank for share.
-
本帖最后由 于 2009-06-17 10:41:00 编辑
Thank you all for your input and Dr. Huang's translation.
To answer 漫游人:
I have never used pericyte stain. You can share your knowledge if you used the stain.
Ki67 positive cells should be <5%.
You said you cannot sign out case indipendently. Are you a reisident or fellow? I like your discussion a lot. You like an experienced pathologists.
Welcome to share your knowledge here.
-
本帖最后由 于 2009-07-08 22:44:00 编辑
| 以下是引用quyibl在2009-6-15 20:22:00的发言:
沉了,顶上来! KI67阳性率不超过5%,肿瘤大小0.7*0.5cm,无放射史。这些都不支持诊断恶性。没经验,搬个板凳学习中....等待老师的讲解。 |
Good. I am waiting you and others' final diagnosis.
Now you know all information for this pt. How would you sign out this case if it were your pt. Then I will tell you my report.
Of cause my report does not mean correct one.
abin译:
很好。我在等着你和别人的最终诊断。
现在你知道了患者的所有信息。如果是你的病例,你会怎样签发报告?然后我会告诉你,我是怎样签发的。
当然我的报告并不意味着一定正确。
-
本帖最后由 于 2009-07-08 22:40:00 编辑
http://www.ipathology.cn/forum/forum_display.asp?keyno=143381
Dr. wfbjwt had an interesting breast vascular lesion case above with a lot of discussion. You can compare the two cases for study purpose if you are interested.
abin译:
http://www.ipathology.cn/forum/forum_display.asp?keyno=143381
这个链接是Dr.wfbjwt提供的一例关于乳腺血管病变的有趣病例,有很多讨论。如果有兴趣,作为学习目的,你可以比较这两个病例。
-
本帖最后由 于 2009-06-09 21:45:00 编辑
Thank all discussion above. Very good. This is the way for discussion.
When we make a diagnosis we should consider the sample types. Generally our diagnosis will guide the next surgical procedure. The standard care is that the women should have total masterectomy if we call angiosarcoma.
To answer Dr. 漫游人 's question: The location of the lesion is 11 o'clock, parenchyma. You analysis is excelelnt.
Dr. Rosen's paper quyibl mentioned is a good one in term of benign or malignant breast vascular lesion.
I had ki67 stain. Will take a photo and paste here.
Welcome more people to share the oppinion. Thanks, cz
quyibl译:
谢谢上面精彩的讨论。这才是讨论的方式。
当我们做出一个诊断时我们应当考虑标本的类型。通常我们的诊断将指导下一步的外科手术方式。如果我们诊断血管肉瘤,标准的处理方式是这位女士做全乳腺切除。
回答“漫游人”医生的问题:肿块位于11点,乳腺实质内。你的分析很精彩。
Rosen的论文是一个不错的鉴别乳腺血管肿瘤良恶性的方法。我做了ki67的染色,会采集照片贴在这的。
欢迎更多的人参与讨论。谢谢,CZ。
-
本帖最后由 于 2009-06-07 17:47:00 编辑
I remeber we had a breast vascular lesion case in this web with a lot of debatable discusion.
Above is a my case three weeks ago. Patient has no cancer or radiation history. She did have a breast core biopsy in the same breast two years ago. The diagosis was small papilloma and ducatal hyperplsia. I reviewed the previous breast core slides and agree with the interpretation. I called the radiologist to review the current and previous imaging films to confirm current lesion and the biopsy lesion two years ago were different areas. I felt difficult to sign out the breasst core biopsy case. Just wonder how you guys would sign out the case if it were yours.
I am on service for FNA on site evaluation for surgeons (several lung mass patients) this weekend. Now we are waiting for patient and I have time to send you this case. Enjoy your weekend
cz
quyibl译:
我记得网上有过一个存在很大争议的乳腺血管性病变的病例。
上面这个是我三周前的一个病例。病人没有乳腺癌或放射线照射史。两年前同侧乳腺做过活检,诊断是小的乳头状瘤伴导管增生。我复习了原先的乳腺活检切片,同意当时的诊断。我请放射科医师复验现在和原先的影像片,确定两次病变不在同一位置。我感到签出这个病例很困难,非常想知道如果这是你的病例,你会怎么签发这个报告。
这个周末, 我在为外科医生做现场的FNA(几个肺部包块的病人),现在正在等待病人,所以有时间发送给你们这个病例。 周末愉快!cz