| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B1278Vulvar anaplastic large T cell lymphoma ALK-1 negative (cqz1)
| 姓 名: | ××× | 性别: | F | 年龄: | 65-70 |
| 标本名称: | Vulvar lesion | ||||
| 简要病史: | |||||
| 肉眼检查: | |||||
Just signed a case two weeks ago and like to share it with all friends here.
Vulvar mass 5 cm. No previous malignant history.
Fig Key:
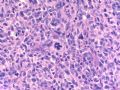
Fig 1. 2x
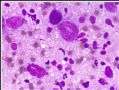
Fig 2. 20x juction
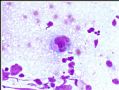
Fig 3. 20x tumor
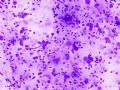
Fig 4. 40x tumor
Tumor shows similar morphology in different areas.
Please give your differential dx and the requirement for IHC stains if it is your case. What is your favor diagnosis based on the H&E slides?
I will have few weeks vocation and will poster the immunostain photos or results after I come back.
Thnaks,
-
本帖最后由 于 2009-02-25 09:47:00 编辑
| 以下是引用abin在2008-10-29 18:32:00的发言:
再次学习,并参考了陈国璋教授的讲课资料。 如果是淋巴造血系统肿瘤: LARGE CELL HEMATOLYMPHOID NEOPLASMS: Main considerations
Abundant pink cytoplasm: Histiocytic/ dendritic cell tumor
 |
Abin has done great job on this case and I am with him for differential diagnoses.
澄泉兄,别掉我们的胃口了,给个结果吧,我们都望眼欲穿了。
于北京机场等机厅

- 不坠青云之志,长怀赤子之心
那Granzyme B,EMA,CD56呢?从T细胞的表达上,我认为CD20应该是真阴性,但是在所提供的图片中没有见到阳性信号,好像这个染色不是很漂亮了,呵呵。
这个部位的T细胞淋巴瘤还真是少见。我前一段时间总结了80多例ALCL,没有一例是在宫颈的。现在的免疫表型确实可以诊断ALCL,但是还是想知道其他的免疫表型。还有一个问题就是:ALK-ALCL和PTCL-NOS怎么鉴别?PTCL也是可以表达CD30的。不知道老师在美国是怎么鉴别的?
谢谢老师提供的好病例。不过现在回过头来重新看病例,我还是会首先想到DLBCL,不会马上定位到ALCL,即使一些细胞形态很像,我仍然会首先想到这个部位常见的肿瘤(有点死脑筋噢),呵呵。再次感谢老师!
-
本帖最后由 于 2008-11-11 17:53:00 编辑
-
Peripheral T-cell Lymphoma With Follicular T-cell Markers.
To: Shiyan:
I am an gyn/breast pathologists and cytopathologist, very short of knowledge in hematopath. I am sure that you know much more than I know. I find a good paper PTCL. I can email you the full paper if you want to and told me your email.
Am J Surg Pathol. 2008 Sep 5. [Epub ahead of print]
-
本帖最后由 于 2008-11-11 17:58:00 编辑
thank all of you for your discussion. After I got the first IHC results, I sign-out the case as hemologic/lymphocytic malignancy and sent the case to our hemotopathologist for further evaluation. The final dx is ATCL , ALK neg.
Thank Abin's excellent analysis. I especially appreciate the first reviewer WY1992. You are great you can consider T cell lymphoma immediately. In fact Lymphoma is my last consideration. Ha ha.
I will present more follow-up data soon.
abin译:谢谢大家参与讨论。第一批IHC结果,我签发了造血/淋巴系统恶性肿瘤,然后转给我们的血液病理医生进一步分型。
最后诊断:ATCL,ALK阴性。
谢谢abin,分析非常好。特别赞赏第一个发表意见的WY1992,能立即考虑到T细胞淋巴瘤。实际上淋巴瘤是我的最后考虑,哈哈。我将提供更多随访资料。
-
本帖最后由 于 2008-11-12 22:27:00 编辑
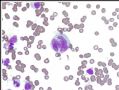
After the original dx of valvar lesion, an enlarged LN was found in pelvic area. FNA was performed.(外阴病变诊断后,发现盆部肿大淋巴结1枚,行FNA)
Fig 1-5 cytology of lymph node FNA. (图1-5为淋巴结FNA细胞学)
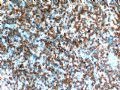
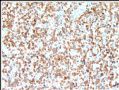
Fig 6: CD3
Fig 7: CD20
Fig 8: CD30
All other IHC results in cell block are the same as that in valvar lesion.
molecular analysis of ALK is negative. (细胞块其余IHC结果与外阴病变相同。分子学检测ALK阴性)
Above lymph node is inguinal LN.
This case was present by our GYN fellow in the dept conference. I share some of her summary with you.
¢ Primary extranodal lymphoma involving the female genital tract ranges from 0.2 to 1.1%.
l Cervix and ovaries most frequent, then uterine corpus and vagina, with vulva and fallopian tubes least common.
¢ Disseminated lymphoma secondarily involves the female genital tract in 7 to 30% of cases.
l Ovary most commonly, then uterus.
¢ Patients with vulvar lymphoma tend to be older than patients with lymphoma at other sites, mean 60 years.
¢ DLBCL is the most common lymphoma affecting the female genital tract (except in fallopian tube).
¢ In vulva, DLBCL is most frequent, with follicular lymphoma next.
ALCL, ALK Positive
¢ Accounts for approximately 3% of adult non-Hodgkin lymphomas.
l 10-20% of childhood.
¢ ALK-positive is most frequent first three decades of life, and shows male predominance.
¢ Usually involves LN and extranodal sites.
l Most frequent skin (21%), bone (17%), soft tissue (17%), lung (11%), and liver (8%).
¢ Bone marrow involvement 10% with H&E.
l Increased to 30% when immunostains for CD30, EMA and/or ALK applied.
¢ Broad morphologic spectrum.
¢ All show cells with eccentric, horseshoe- or kidney-shaped nuclei = “hallmark cells”.
¢ Multiple nuclei may occur in a wreath-like pattern.
¢ In general, more abundant cytoplasm than most lymphomas.
¢ CD30 positive in a membranous pattern.
¢ Translocation t(2;5)-NPM/ALK is most frequent genetic alteration.
l Shows nuclear and cytoplasmic staining.
l Fusion of ALK protein, usually transmembrane with NPM, nuclear transport protein.
¢ ALK expression virtually specific for ALCL.
¢ Absent from most other human neoplasms.
l Rare DLBCL.
l Rare cases of rhabdomyosarcoma.
l Inflammatory myofibroblastic tumors.
¢ Majority positive for EMA.
¢ Vast majority express one or more T-cell antigens; CD4+/CD8-.
¢ Variably positive for CD45.
¢ Most positive for cytotoxic-associated antigens TIA1, granzyme B, and/or perforin.
¢ 90% show clonal rearrangement of T-cell receptor.
¢ EBV is always absent.
ALCL, ALK Negative
¢ Included as provisional entity in most recent WHO.
l “CD30+ T-cell neoplasm not reproducibly distinguishable on morphological grounds from ALCL, ALK+”.
l Older median age and more aggressive clinical course than ALK+ ALCL.
¢ Considered distinct from peripheral T-cell lymphoma, NOS, but distinction is not always straightforward.
¢ Peak incidence 40-65 years.
¢ Male predominance, 1.5:1.
¢ Involves lymph nodes and extranodal sites, but less commonly than ALCL, ALK+.
¢ Tumor cells larger and more pleomorphic.
¢ More than half of cases express one or more T-cell markers; CD4+/CD8-.
¢ More likely to be positive for CD2 and CD3.
¢ Fewer positive for EMA.
¢ Majority show cytotoxic-associated markers.
¢ Most show clonal rearrangement of T-cell receptor.
¢ No recurrent cytogenetic abnormalities.
ALCL, ALK Negative DDx
¢ Differential diagnosis
l Primary cutaneous ALCL
l Other primary cutaneous CD30+ lymphoproliferative disorders
• But lymphomatoid papulosis (LyP) is, by definition, limited to skin
l Peripheral T-cell lymphoma, NOS
¢ Primary cutaneous ALCL
l Disease is limited to skin at time of diagnosis.
l Extracutaneous dissemination may occur, mainly to regional lymph nodes.
l Predominantly in adults and elderly.
l T-cell phenotype with variable loss of CD2, CD5 and/or CD3; CD30 expression >75% cells.
l Most cases negative for EMA and ALK.
l Overall 5-year survival rate of 90%.
¢ Peripheral T-cell lymphoma, NOS
l May be nodal or extranodal; skin and GI tract most common.
l Abnormal medium to large lymphocytes often admixed with inflammatory cells.
l Sinus pattern of LN infiltration is absent.
l T-cell phenotype; CD4+/CD8-.
l More likely to be positive for CD2, CD3.
l CD30 may be seen, but usually with variable intensity, and not in strong, homogeneous, membranous pattern.
Conclusions
¢ Lymphoma, primary or secondary, is rare in the vulva.
¢ Most common type is DLBCL.
¢ Tend to occur in older women.
¢ ALCL, systemic and primary cutaneous types.
l ALCL, ALK-negative provisional entity in new WHO.
l Evidence that ALK+ ALCL, ALK- ALCL, and PTCL, NOS are distinct entities.
¢ Lymphoma should be included in the differential diagnosis of vulvar mass.
We did not find valvar ALCL report in literature serach. I asked the fellow to write a case report.
Now you see all of the case already.
Thank for discussion and reviewing of this case.
, then uterus
-
本帖最后由 于 2008-11-12 23:00:00 编辑
| 以下是引用cqzhao在2008-11-12 11:30:00的发言并翻译:
上述淋巴结为腹股沟淋巴结。 病例由我们的妇科病理同事在科室讨论会上提供。我把她的一些总结和大家分享。 ¢ 累及女性生殖道的原发性结外淋巴瘤:0.2 to 1.1% l 宫颈和卵巢最常见,其次是宫体和阴道,外阴和输卵管最少 ¢ 累及女性生殖道的继发性结外淋巴瘤: 7 to 30% 例 l 卵巢最常见,其次是子宫
¢ 外阴淋巴瘤患者倾向于比其它部位发生者年龄更大,平均60岁 ¢ DLBCL是最常见的累及女性生殖道的淋巴瘤(输卵管除外) ¢ 外阴DLBCL最常见,其次为滤泡性淋巴瘤
ALCL, ALK Positive
¢ 约占成人NHL的3% l 10-20%为儿童 ¢ ALK阳性最常见于30岁之前,多为男性 ¢ 通常累犯LN和结外 l 皮肤最常见(21%), 骨(17%), 软组织(17%), 肺(11%), 肝 (8%). ¢ HE染色观察到10%累犯骨髓 l 运用IHC染色CD30, EMA和/或ALK后增加到30% ¢ 宽广的形态学谱系 ¢ 所有病例均显示细胞核偏心、马蹄形或肾形=特征性细胞 ¢ 可出现多核,花环样 ¢ 一般比大多数淋巴瘤更富于胞浆 ¢ CD30呈膜阳性 ¢ t(2;5)-NPM/ALK 易位是最常见的遗传学改变 l 显示核和胞浆着色 l ALK蛋白融合,通常与NPM形成跨膜蛋白 ¢ ALK表达实际上是ALCL的特征 ¢ 不见于其他人类肿瘤 l 罕见DLBCL l 罕见横肉 l 炎性肌纤母细胞肿瘤 ¢ 大部分EMA阳性
¢ 绝大多数表达一种以上的T-cell抗原; CD4+/CD8-. ¢ CD45表达不一 ¢ 大多数表达细胞毒性标记物:TIA1, 粒酶B, and/or 穿孔素. ¢ 90%呈T-cell受体克隆性重排 ¢ 通常无EBV
ALCL, ALK Negative
¢ Included as provisional entity in most recent WHO. l “CD30+ T-cell neoplasm not reproducibly distinguishable on morphological grounds from ALCL, ALK+”. l Older median age and more aggressive clinical course than ALK+ ALCL. ¢ Considered distinct from peripheral T-cell lymphoma, NOS, but distinction is not always straightforward. ¢ Peak incidence 40-65 years. ¢ Male predominance, 1.5:1. ¢ Involves lymph nodes and extranodal sites, but less commonly than ALCL, ALK+. ¢ Tumor cells larger and more pleomorphic. ¢ More than half of cases express one or more T-cell markers; CD4+/CD8-. ¢ More likely to be positive for CD2 and CD3. ¢ Fewer positive for EMA. ¢ Majority show cytotoxic-associated markers. ¢ Most show clonal rearrangement of T-cell receptor. ¢ No recurrent cytogenetic abnormalities.
ALCL, ALK Negative DDx ¢ Differential diagnosis l Primary cutaneous ALCL l Other primary cutaneous CD30+ lymphoproliferative disorders • But lymphomatoid papulosis (LyP) is, by definition, limited to skin l Peripheral T-cell lymphoma, NOS ¢ Primary cutaneous ALCL l Disease is limited to skin at time of diagnosis. l Extracutaneous dissemination may occur, mainly to regional lymph nodes. l Predominantly in adults and elderly. l T-cell phenotype with variable loss of CD2, CD5 and/or CD3; CD30 expression >75% cells. l Most cases negative for EMA and ALK. l Overall 5-year survival rate of 90%. ¢ Peripheral T-cell lymphoma, NOS l May be nodal or extranodal; skin and GI tract most common. l Abnormal medium to large lymphocytes often admixed with inflammatory cells. l Sinus pattern of LN infiltration is absent. l T-cell phenotype; CD4+/CD8-. l More likely to be positive for CD2, CD3. l CD30 may be seen, but usually with variable intensity, and not in strong, homogeneous, membranous pattern. Conclusions ¢ Lymphoma, primary or secondary, is rare in the vulva. ¢ Most common type is DLBCL. ¢ Tend to occur in older women. ¢ ALCL, systemic and primary cutaneous types. l ALCL, ALK-negative provisional entity in new WHO. l Evidence that ALK+ ALCL, ALK- ALCL, and PTCL, NOS are distinct entities. ¢ Lymphoma should be included in the differential diagnosis of vulvar mass.
我们在文献中没有搜索到外阴 ALCL,我要同事写一篇病例报道。 现在你已经看到这个病例的全部内容。
谢谢讨论和浏览。 接着,是子宫 |
sorry!
翻译这些对我来说太难了,因为我不懂淋巴瘤。其余的内容要请其他朋友帮助一下。谢谢
abin

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
Thank abin for the excellent translation.
Fellow does not mean colleaque. In the US you need four years of pathology residency training after the medical school. Most people will do one or two fellowship training in some subspecieties. It needs one year of fellow training. So fellow means one subspecilty training after residency training. Pathology fellows include many subspecieties, GI, gynecology, breast, derm, hematology, GU, ENT et al.