| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
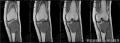
- 左胫骨近端肿块-上海市骨与关节肿瘤读片2013(2-4)-上海交大附属市六院提供
| 性别 | 女 | 年龄 | 22 | 临床诊断 | 骨巨细胞瘤? |
|---|---|---|---|---|---|
| 一般病史 | 患者无明显诱因下出现左膝肿胀、疼痛6月,活动受限。影像学:左胫骨近端偏心性椭圆形低密度病灶,中间有分隔,周围有硬化。考虑骨巨细胞瘤。入院行穿刺活检。 | ||||
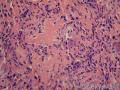
| 标本名称 | 左胫骨近端肿块活检。 | ||||
| 大体所见 | 如低倍镜下所见大小碎组织。 | ||||
-
本帖最后由 海上明月 于 2013-10-09 15:51:09 编辑

- 王军臣
相关帖子
有支持点但也有疑问之处:
髓内高分化骨肉瘤被新的WHO分类当做低级别中心性骨肉瘤的同义词,其组织学叙述中提到:有高达36%的例子可见到良性的多核巨细胞。而富于巨细胞的骨肉瘤我记得是分在传统型/普通型骨肉瘤里面而不是高分化或低级别里面,这产生了矛盾,这个富于巨细胞的修饰语似乎属于高级别骨肉瘤。
髓内高分化骨肉瘤经典HE图片是类似于纤维结构不良或骨旁骨肉瘤那种,当然也有其它变化的形态,如骨样基质数量范围不等,有软骨成分等等——本例就这些特征还是符合,所以本例HE形态不是经典那种,就本例来说能说一定是高分化吗?而原发恶性骨巨细胞瘤形态就是骨巨细胞瘤+肉瘤成分,肉瘤成分没有明确规定是什么类型,但以骨肉瘤和纤维肉瘤为多。髓内高分化骨肉瘤进展缓慢,很多年后有进展为高级别骨肉瘤或去分化骨肉瘤的特性,但刚开始总是一个惰性的肿瘤。影像学据说很多是溶骨性病变和或硬化同时存在,局部表现为云雾样硬化。有时候很难在影像学上认为是恶性,但骨皮质有缺损破坏并累及周围软组织影像学上应高度怀疑恶性。本例影像学符合。但原发骨巨细胞瘤恶变/恶性转化也有类似的影像学特征。见:All PMGCTs(Primary malignancy in giant cell tumor of bone ) appeared on plain films as osteolytic lesions with well-circumscribed margins in the epiphyses of long bones . An area of less distinct margins was present in two cases, and cortical breakthrough was observed in four cases. A soft tissue mass was seen on plain films in two of the five cases. A sclerotic component was present in two lesions. Two cases were radiographically determined to be worrisome for malignancy (defined as having a large mass permeating the bone and cortex, with extensive soft tissue involvement). The other three cases were identified by radiographs as Enneking Stage III giant cell tumors——所以仅从影像学还真不好和“恶性在骨巨细胞瘤中”鉴别
免疫组化看过文献MDM2和CDK4有帮助。那篇文献鉴别了纤维结构不良和骨化性肌炎,因为它们有形态重叠的地方。
P63在骨肿瘤表达存在争议,早先有文献指出P63鉴别骨巨细胞瘤和骨肉瘤、骨母、软组织腱鞘巨细胞瘤有帮助,后来有篇文献认为没有明显帮助,他们都表达,尽管存在表达率差异,倒是指出P63有判断预后价值,高表达预后差些。
预后有说原发比继发好,尤其是比放疗后继发骨巨恶变的那种好,但有的又认为预后一样。
PMGCT(原发恶性骨巨细胞瘤) should be differentiated from giant cell–rich osteosarcoma, but as in the mononuclear cells of giant cell–rich osteosarcomas, the cytologic evidence of malignancy in certain areas can be very subtle. Differentiation between these two lesions sometimes is difficult, and its clinical importance probably is limited. More important is the fact that both types of lesions can be difficult to differentiate from benign giant cell tumors. Diagnosis of PMGCT is difficult because it contains areas of benign giant cell tumor, such that a biopsy may not initially detect the malignant portion.骨巨细胞瘤恶变和富于巨细胞的骨肉瘤鉴别有时候很困难
Radiol Med. 2013 May 28. [Epub ahead of
print]
Giant cell-rich osteosarcoma in long
bones: clinical, radiological and pathological features.
Wang CS, Yin QH, Liao JS, Lou JH, Ding XY, Zhu YB.
Source
Department of Radiology, Ruijin
Hospital, Shanghai Jiao Tong University School of Medicine, No.197, Ruijin 2nd
Road, Shanghai, 200025, China.
Abstract
PURPOSE:
The purpose of
this study was to review the clinical presentation, imaging, pathology and
outcome of patients withgiant cell-rich osteosarcoma (GCRO) of
long bones.
MATERIALS AND METHODS:
Radiography (n=9),
magnetic resonance imaging (MRI) (n=6), computed tomography (CT) (n=3) and
clinical course of nine patients (five males and four females; mean age, 26
years) with pathologically confirmed GCRO were retrospectively reviewed.
Specific imaging findings, including size, eccentricity, ossification, lysis,
cystic change, expansile growth, periosteal reaction, cortical destruction,
soft tissue extension and joint involvement were documented.
RESULTS:
Presenting
symptoms were pain in six patients and pain and palpable mass in three. An
ill-defined margin surrounding a predominantly osteolytic lesion was detected
at the proximal tibia (n=7) or femur (n=2) on imaging studies. Seven cases
showed limited ossification. Three cases had tumours in the metaphysis and six
in the metaepiphysis. The average maximum tumour dimension was 4.7 cm×5.2
cm×7.8 cm. Microscopically, tumours were composed of atypical cells with scanty
osteoid formation and multinucleated giant cells. All patients
received chemotherapy, and surgery was performed in eight patients. Three
patients were dead and six were alive at the last follow-up.
CONCLUSIONS:
GCRO is a rarer
variant that has very close resemblance to giant cell tumour.
Patients usually present nonspecific symptoms of pain and palpable mass. It
usually shows an osteolytic lesion with locally spared new bone formation in
the metaphysis and/or metaepiphysis on imaging. Histologically, the atypical
tumour cells with osteoid formation and multinucleatedgiant cells are the
key factor in the diagnosis and differential diagnosis.

- 王军臣