| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 2012年第9期—背部肿物(已点评)
- 图1
- 图2
- 图3
- 图4
- 图5
- 图6
- 图7
- 图8
- 图9
- 图10
- 图11
- 图12
- 图13
- 图14
- 图15
- 图16
- 图17
- 图18
- 图19
- 图20
- 图21
- 图22
- 图23
- 图24
- 图25
- 图26
- 图27
- 图28
- 图29
- 图30
| 性别 | 男 | 年龄 | 65 岁 | 临床诊断 | 肿瘤? |
|---|---|---|---|---|---|
| 临床症状 | 患者于半年前无明显诱因发现背部一肿块约乒乓球大小,无明显疼痛,肿块浅黑色,无头痛,头昏,肿块渐增大,至今约鸡蛋大小,并相继在肩部、背部及颈部出现大小不等肿块十余个,一直未予注意。肩背部及颈部见多个肿块,肿块处皮肤呈咖啡色,大者约4×4×3cm,小者约0.5×0.5×0.5cm,活动差,无压痛。实验室检查无异常,影像学检查未见转移灶。 | ||||
| 标本名称 | 背部包块 | ||||
| 大体所见 | 送检梭形带皮组织5块共约7×6×5cm,每块组织均逐一切开,皮下分别见直径为3.5cm~0.3cm灰红灰白色结节12个,多数结节边界清楚,质嫩,其中最大结节边界不甚清楚,周围可见小卫星结节。 | ||||
免疫组化结果:CK8、CK19、CEA(+);EMA、P63部分瘤细胞(+);P53(-);Ki67:5%(+),且阳性细胞集中于肿瘤的区域;CK5(-)。
点评专家:中国医学科学院 、协和医科大学皮肤病研究所病理研究室:曾学思老师
专家介绍:http://teach.ipathology.cn/article/1565.html
点评专家:曾学思(50楼 链接:>>点击查看<< )
获奖名单:TK1905(3楼 链接:>>点击查看<< )
-
本帖最后由 草原 于 2012-09-24 08:44:33 编辑

- 人淡如菊,心素如简。
-
谢谢你们陪我容颜到老 离线
- 帖子:1
- 粉蓝豆:1
- 经验:3
- 注册时间:2012-02-22
- 加关注 | 发消息
-
本帖最后由 TK1905 于 2012-03-08 22:04:45 编辑
“晕倒,我建议您结合本例的图像再看看你的英文部分,请您指点本例那些图中可见顶浆分泌?我想我所指的是本例可以做免疫组化证明小汗腺起源,而你所要表达的是:不是所有的病例都是来源于小汗腺!完全是两码事情”
————————————————————————————————————————————————————————
我已经在后面的这句话“本例形态学见恶性转化的导管上皮胞浆非常丰富,嗜酸性、核空泡状,见显著中位核仁,导管成分像前述的形态学特征说不定就是大汗腺导管癌呢”中明显指出了可能是大汗腺分化!!!注意是说的可能,没说一定。本例核大空泡状,胞浆巨丰富的嗜酸性的恶性上皮细胞至少就我个人的有限经验是小汗腺的汗腺癌未见过这样的类似形态,这就是我说的有恶性顶浆分泌腺的特征,但是我不敢肯定,因为皮脂腺癌有类似的细胞学特征。正因为这个特征我在鉴别诊断里面首先想到了皮脂腺癌,其它很多网友也考虑了皮脂腺癌可能也是因为这个肿瘤的细胞学形态像皮脂腺分化的细胞,肿瘤中其它体积小的细胞可以视为皮脂腺肿瘤的原始生发细胞,成熟皮脂腺细胞由它们分化而来,但是皮脂腺癌毕竟不会见到导管分化,本例导管分化极其明显,所以可能性不大,最多是螺旋腺癌伴有皮脂腺分化。
我觉得本例有点像这篇文献的特点:
American Journal of Dermatopathology:
October 2008 - Volume 30 - Issue 5 - pp 436-441 doi: 10.1097/DAD.0b013e3181812729
Original Article
Spiradenoma and Spiradenocylindroma With an Adenomatous or Atypical Adenomatous Component: A Clinicopathological Study of 6 Cases
Abstract
We report 5 cases of spiradenoma and 1 case of spiradenocylindroma, which, in addition to areas of conventional growth, manifested an adenomatous component. This consisted of compactly situated, well-developed glands having small round lumens lined by inner pale to eosinophilic cells and surrounded by an outer well-formed peripheral layer of myoepithelial cells, which reacted with a variety of myoepithelial cell markers. In 1 case, apocrine secretion was evident in the glandular part of the lesion. In 4 of the 6 cases, the adenomatous component was a minor but significant portion of the tumors, but in 2 cases it was extensive, comprising approximately 20% of the tumor area. In 1 of these 2 cases, the luminal epithelium showed atypia including rare, atypical mitotic figures. In addition, there were foci of glands showing myoepithelial cell loss. As this alteration was limited and fairly well circumscribed within the tumor bulk, we regard it as an “atypical adenomatous component,” but we cannot exclude the possibility that this may represent an incipient apocrine carcinoma, despite uneventful follow-up. Three cases also manifested clear cell areas. Immunohistochemical studies demonstrated that myoepithelial proliferation and overgrowth accounted for the clear cell change in some of the lesions.
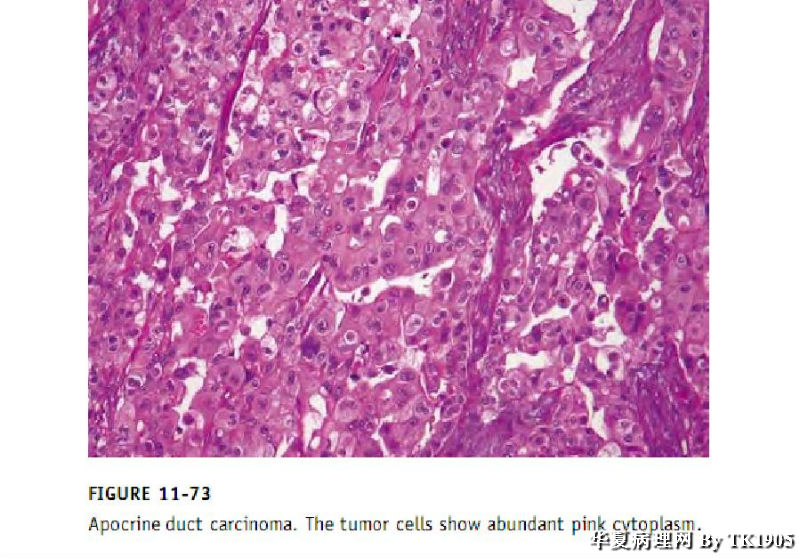
下面是一张大汗腺导管癌的图片可以与本例恶性上皮细胞做对比
本例最终如果做了工作证明有可能是大汗腺分化或皮脂腺分化的话,那么本例有可能是又一例验证一个假说(起源于毛囊-皮脂腺-大汗腺单位)的例子,这是后话,见后面的文献
===========================================================================================
ps:这篇文章应该是96年发在pathology research and practice上的文章,查了一下
· MedSci评语:杂志水平一般,也很冷门,关注人少,审稿周期可能也不一定快,如果文章质量不佳,或时间不紧的话,可以考虑考虑。近年来if大概1点多。
您隆重推荐的IKH-4我也查了下,是1998年的,总共只搜到1篇与汗腺有关的,看来实际工作中病理人用它的真的很少。很难说免疫组化对确定是小汗腺还是大汗腺起源有肯定的作用,很多提示有其它起源证据的文章并不是完全依靠免疫组化。您推荐的标记的文章如下:
J Cutan Pathol. 1998 Feb;25(2):100-5.
Staining of eccrine and apocrine neoplasms and metastatic adenocarcinoma with IKH-4, a monoclonal antibody specific for the eccrine gland.
Ishihara M, Mehregan DR, Hashimoto K, Yotsumoto S, Toi Y, Pietruk T, Mehregan AH, Mehregan DA.
Abstract
The histogenesis of apocrine and eccrine neoplasms has always interested dermatopathologists. In addition, the histologic differential diagnosis of eccrine carcinoma from metastatic adenocarcinoma is of practical importance. We describe a novel monoclonal antibody IKH-4 which stains the eccrine secretory coil, but not the apocrine secretory segment. Positive staining was observed in eccrine hidradenoma, eccrine poroma, eccrine spiradenoma, papillary eccrine adenoma, eccrine hidrocystoma, syringoma, eccrine carcinoma, and in 1 case of syringocystadenoma papilliferum. Negative staining was observed in apocrine adenocarcinoma, hidradenoma papilliferum, erosive adenomatosis of the nipple, and primary and metastatic adenocarcinomas. IKH-4 antibody was useful in differentiating eccrine from apocrine neoplasms and in differentiating eccrine carcinoma from metastatic adenocarcinomas.
同样对您的这篇文章的杂志评价是这样的:
MedSci评语:杂志水平一般,也很冷门,关注人少,审稿周期可能也不一定快,如果文章质量不佳,或时间不紧的话,可以考虑考虑。
本人有不同观点,重看了图片发现良性腺体与恶性腺体之间貌似有过渡,交叉分部,提示两种腺体可能来源相同,因此首先考虑小汗腺来源的,如果按照上面哥们的看法提出的鉴别诊断的话,我觉得更加有必要做IKH-4了,因为这个不仅能够转移性癌,而且能够鉴别大小汗腺来源肿瘤!如果+那就还是小汗腺来源的了!- 的情况俺现在还不考虑,- 的话真就不好搞了,不过我坚持认为IKH-4做出来应该是阳性!
2种腺体当然来源相同,正因为有良恶性过渡本例才诊断螺旋腺癌啊!没有良恶性的过渡本例会是疑难病例,很容易误诊为其它如转移癌、滑膜肉瘤、皮脂腺癌、基底细胞癌伴有什么分化等等。良恶性过渡正好是分析和诊断的线索又是诊断的重要依据之一。您不要先入为主认为良性的那个形态就一定是小汗腺起源,我们重点分析恶变的细胞学形态是不是有大汗腺导管癌的可能?
IKH-4+就是一定是小汗腺?就那篇文章极其有限的样本研究您敢绝对地说一定是只有小汗腺表达大汗腺不可能表达?IHC没有绝对地,只有相对,病理学只靠一个IHC标记就确定那真是太容易了。我还看见别人证明大汗腺用CK15这个标记呢,螺旋腺瘤/圆柱瘤呈部分肿瘤细胞表达
J Dermatol. 2006 Jan;33(1):2-9.
Cytokeratin 15 expression in apocrine mixed tumors of the skin and other benign neoplasms with apocrine differentiation.
Division of Dermatology, Department of Internal Medicine, Faculty of Medicine, Saga University, Saga, Japan. misago@post.saga-med.ac.jp
Abstract
To clarify the features of apocrine mixed tumors (AMT) of the skin among benign neoplasms with apocrine differentiation in their relationship to follicular stem cells, we investigated the immunohistochemical expression of CK15 (LHK15 and C8/144B), which is a relatively specific marker of hair follicle stem cells in the bulge, in 35 cases of eight different benign neoplasms with presumed apocrine differentiation. All eight cases of AMT of the skin showed CK15 immunostaining of the neoplastic cells, and all four cases of syringocystadenoma papilliferum, all five cases of spiradenoma, and both cases of cylindroma also showed a focally positive reaction to CK15. None of the other benign neoplasms with presumed apocrine differentiation showed CK15 expression. In AMT of the skin, the proportion of CK15-positive cells in the follicular or sebaceous differentiation group (78.8%, average of four cases) was significantly higher than the group without this differentiation (8.8%, average of four cases). AMT of the skin are unique among benign neoplasms with apocrine differentiation in their substantial and constant CK15 expression, suggesting that they derive from multipotent epithelial stem cells in the bulge. AMT of the skin with follicular or sebaceous differentiation are considered to show an immature stage of apocrine differentiation still rich in stem cells or to originate from stem cells with an incompletely established apocrine fate. The partially positive reaction for CK15 in syringocystadenomas papilliferum and spiradenoma/cylindroma may depend on the ability to express CK15 in stem cells with an apocrine fate or result from the follicular and apocrine nature of this neoplasm.
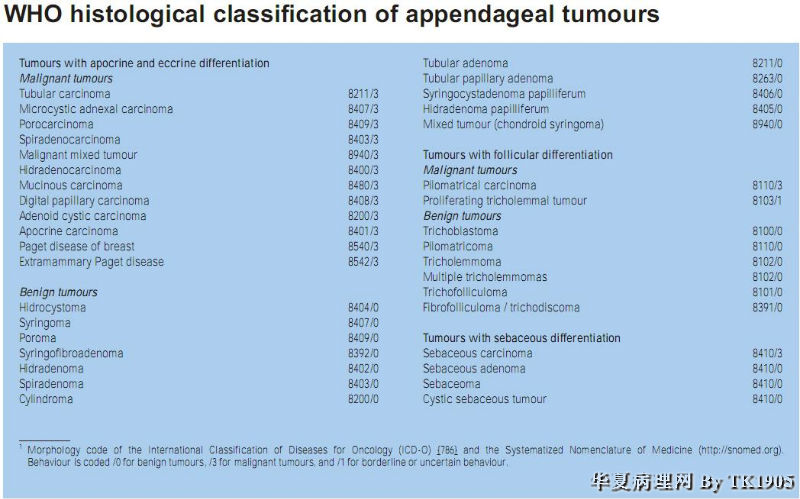
WHO皮肤组织分类把大汗腺小汗腺分化的汗腺肿瘤一起讲,螺旋腺瘤或癌前面已经没有加小汗腺这个词了
下面的分类表可以看到螺旋腺瘤或螺旋腺癌前面去掉小汗腺修饰,后面有讲去掉小汗腺螺旋腺瘤或癌前面的修饰词“小汗腺”的原因
WHO对螺旋腺瘤的定义及组织学起源讨论:
Spiradenoma:
Definition :Spiradenoma is a benign dermal neoplasm that can show either eccrine or apocrine differentiation, and significant morphologic overlap with cylindroma. Historical annotation Chandeluz, in 1882, probably first described this tumour . Unna first coined the term spiradenoma. In 1956 Kersting and Helwig published the classic paper on spiradenoma in 136 patients . Additional series of spiradenoma have since been published.
请重点看下面的关于组织起源的讨论描述
Histogenesis:
The histochemical and immunohistochemical studies have not clarified the histogenesis of spiradenoma. The frequent association of spiradenoma and cylindroma, a likely apocrine neoplasm,and the sporadic association of spiradenoma with neoplasms with follicular differentiation such as trichoepithelioma{2500}, support an apocrine line of differentiation for spiradenoma on the basis of the common embryologic origin for the three elements of the folliculo-sebaceous-apocrine unit. This is furthermore supported by some examples of spiradenoma that show decapitation secretion in the cells lining the luminal border of the tubular structures. Therefore, the qualifying term of “eccrine” that almost invariably is applied to spiradenoma is inaccurate.
-
本帖最后由 TK1905 于 2012-03-08 22:02:23 编辑
其它关于螺旋腺瘤的组织起源发生假说、猜想的一些文献:
American Journal of Dermatopathology:
February 2005 - Volume 27 - Issue 1 - pp 27-33
Extraordinary Case Report
Brooke-Spiegler Syndrome: Report of a Case with Combined Lesions Containing Cylindromatous, Spiradenomatous, Trichoblastomatous, and Sebaceous Differentiation
Kazakov, Dmitry V MD, PhD*; Soukup, Roman MD†; Mukensnabl, Petr MD*; Boudova, Ludmila MD, PhD*; Michal, Michal MD*
![]() <!--[endif]-->
<!--[endif]-->
Abstract
Brooke-Spiegler syndrome is an autosomal dominantly inherited disease with predisposition to cutaneous adnexal neoplasms, most commonly cylindromas and trichoepitheliomas. We report a patient in whom 11 lesions were removed from the scalp and face for various reasons over a period of 3 years. The histopathological survey revealed a plethora of benign adnexal neoplasms showing apocrine, follicular, and sebaceous differentiation occurring independently and conjointly. The histopathological spectrum in our patient included cylindromas, spiradenomas, trichoepitheliomas, small nodular trichoblastomas, and lymphadenomas. Many lesions had hybrid features of two or more neoplasms. By far the most common composite tumor was spiradenocylindroma. Some spiradenocylindromas demonstrated prominent sebaceous or trichoblastomatous differentiation or both. We suggest the terms “sebaceous spiradenocylindroma” and “trichospiradenocylindroma” for these lesions. The occurrence of sebaceous and trichoblastic differentiation in spiradenocylindromas is a further proof that spiradenoma and cylindroma are not eccrine tumors but neoplasms of the folliculosebaceousapocrine unit.
piradenocylindromas of the skin: Tumors with morphological features of spiradenoma and cylindroma in the same lesion: Report of 12 cases
Twelve cases of spiradenocylindromas, which revealed features of both spiradenoma and cylindroma in the same tumor mass, are presented. Nine female patients had multiple neoplasms occurring mostly on the scalp, and two female and one male patient had a solitary cutaneous lesion. Three of the female patients with multiple cutaneous tumors had a familial history of similar cutaneous neoplasms. In one of the patient’s family, the multiple cutaneous tumors were known to occur in multiple family members in four consecutive generations. One patient with multiple cutaneous lesions was known to have associated multiple kidney cysts as confirmed by computed tomography. Histologically, spiradenocylindromas are composed of intermixed areas that are either of typical spiradenoma in appearance or of typical cylindroma appearance. Apocrine and trichoepitheliomatous differentiation seen in two cases in the present series points to spiradenomas, as well as cylindromas, having complex hair follicle (folliculo- sebaceous apocrine) rather than eccrine differentiation. The presence of lymphoid tissue was a histological feature in the present series, which was prominent in all the spiradenomatous parts of the tumors and which was scanty or practically absent in all the cylindromatous parts. The selective presence of lymphocytes in spiradenoma and an absence in cylindroma suggest that spiradenomas have the unique property of attracting lymphocytes. The malignant tumors arising in three patients in the present series had the morphology of a poorly differentiated epithelioid neoplasm. Three patients died of the disease and the other patients were either free of disease or alive with disease 1–30 years on follow up.
Am J Dermatopathol. 1997 Apr;19(2):154-61.
Spiradenoma and dermal cylindroma: comparative immunohistochemical analysis and histogenetic considerations.
Source
Department of Pathology, University of Bonn, F.R.G.
Abstract
We carried out an immunohistochemical analysis of nine spiradenomas and seven cylindromas. Our findings underscore the histomorphological similarities of the two adnexal neoplasms-namely, the expression of S-100 protein ascribed to eccrine differentiation within the tubular and large, pale-staining cells of both entities. Human milk fat globulin (HMFG) and lysozyme, two markers associated with apocrine differentiation, are expressed by tubular cells in spiradenomas and cylindromas. Lysozyme is also expressed in cylindromas by large, pale-staining cells. In addition, antibodies to alpha-smooth muscle actin strongly characterized the small basaloid cells of both types of neoplasm. Both spiradenomas and cylindromas expressed identical cytokeratin patterns. As with the various regions of eccrine and apocrine units, the expression by spiradenomas and cylindromas of keratins 7, 8, and 18 indicates differentiation toward the secretory tissue, whereas the expression of keratin 14 in some of the neoplastic cells points toward ductal differentiation. Malformed ductal and glandular structures in continuity with evolving spiradenomas and cylindromas in two of our cases also suggest that these tumors might arise from abortive adenxal anlagen.
A Rare Case of Multiple Segmental Eccrine Spiradenomas
April 2011
Laura Englander, MD
Abstract
Eccrine spiradenoma is a benign adnexal neoplasm that has been historically designated as a tumor of eccrine differentiation, although current reconsideration indicates an apocrine process. It usually presents on the trunk and extremities as a tender dermal or subcutaneous papule or nodule frequently with a pink or blue hue. The clinical picture is often not distinct and biopsy is required for diagnosis. Eccrine spiradenoma can present in a variety of ways, including as tumors arranged in zosteriform/dermatomal and/or blaschkoid distributions, often precluding a straightforward diagnosis. Proper diagnosis of eccrine spiradenoma is important due to the occurrence of potentially life-threatening malignant transformation. This article illustrates a rare presentation of eccrine spiradenoma with a concise review for the dermatologist. (J Clin Aesthet Dermatol. 2011;4(4):38–44.)
Eccrine spiradenoma (ES), first described in 1956, is an uncommon, benign, dermal tumor of apocrine differentiation derived from cutaneous sweat glands.[1] It classically presents in the 2nd to 4th decades of life as a small, painful, grey to pink nodule on the upper ventral aspect of the body. Most presentations of ES are solitary, comprising more than 97 percent of cases. The incidence of ES is roughly equivalent in men and women.[2–4] Multiple ES is a rare phenomenon, comprising less than two percent of all cases and appears to be predominant among women.[5,6] Approximately 37 cases of multiple ES, including those in zosteriform/dermatomal and/or blaschkoid distributions, have been reported in the literature.[2,4,6–28] Given the rarity of multiple ES in a linear distribution and the uncommon risk of malignant transformation, the authors present this case for interest, review, and awareness.
Case Report
A 55-year-old Caucasian man presented to the authors’ outpatient dermatology clinic complaining of a 20-year history of painful lesions on the right chest and arm. Of patient concern, the lesions were recently more painful and had increased in size and number. His past medical history was unremarkable. He denied any family members with similar skin findings or any history of skin cancers. Physical exam revealed multiple, well-circumscribed, subcutaneous, blue-grey nodules in a dermatomal distribution across the right chest and arm (Figure 1). The nodules were tender, firm, and fixed to the overlying skin and ranged in size from 0.5 to 6cm in diameter. Surgical excision of the most prominent, painful nodule of the right arm was sent for histological analysis (Figure 2).
Histological findings demonstrated sharply delineated dermal nodules comprising basaloid cells arranged in a trabecular pattern surrounded by eosinophilic fibrous strands (Figure 3). Small, dark, basaloid cells with hyperchromatic nuclei, larger cells with pale nuclei in the center of the clusters, and numerous scattered lymphocytes were also seen throughout, consistent with a diagnosis of ES (Figure 4). Typical spiradenoma features, as well as small areas with a cylindroma-like “jigsaw puzzle” pattern, were also appreciated. No evidence of malignant transformation was noted.
The patient underwent surgical excision with complex, linear closure of multiple chest and arm nodules given the significant pain experienced while wearing a seatbelt during driving. Excellent cosmetic and functional results were seen and the patient was advised to return for future excisions in the case of increasingly painful or rapidly growing lesions. While there was no evidence of malignant transformation in this patient, continuous follow up is necessary given the rapid evolution and possibility of malignant transformation within long-standing lesions.
Etiology. The exact etiology of ES still remains controversial. ES has never been observed on glabrous skin, as it is an undifferentiated or poorly differentiated benign adnexal neoplasm historically designated as a tumor of eccrine lineage. However, both ES and cylindroma can sometimes display tubular differentiation with a “decapitation” pattern as would be expected in an apocrine neoplasm.[47,48] Thus, recent assessment has indicated an apocrine process. As previously described, ES commonly occurs jointly with other cutaneous appendage tumors, such as cylindroma, trichoepithelioma, and trichoblastoma, which points toward the development of folliculosebaceous-apocrine lineage rather than eccrine differentiation.[49,50] Further, if ES were truly eccrine, occurrence on the palm or sole would be paramount rather than rarely seen. In Brooke-Spiegler syndrome, a defective tumor suppressor gene, CYLD on chromosome 16q, results in numerous cutaneous appendage tumors suggesting kinship rather than disparate lineages.[46,51] The most recent hypothesis is suggestive of an abnormal multipotent stem cell in the folliculosebaceous-apocrine unit, although some reports have suggested trauma as the inciting factor.[43,52] p53 expression in malignant ES is also suggestive of an underlying abnormality of tumor suppression or innate surveillance, but the significance of this observation is currently unclear.
The histogenesis of spiradenomas remains in question, but many lesions demonstrate apocrine differentiation. The term eccrine spiradenoma may join the list of other misnomers in dermatology, including mycosis fungoides and granuloma faciale. Lesions usually manifest as solitary, 1-cm-diameter, gray, pink, purple, red, or blue nodules on the upper half of the ventral side of the body. Spiradenomas can be painful, often in paroxysms. Multiple spiradenomas have been reported. Their initial elaboration is attributed to Kersting and Helwig.[1]
Spiradenomas are usually benign. It can occur in infancy but most commonly arises in persons aged 15-35 years. About 15 cases of linear/zosteriform/nevoid/blaschkoid multiple spiradenomas exist in the literature.[2, 3] About 50 case reports of malignant spiradenoma exist in the literature. Dabska[4] first described malignant spiradenoma in 1972.
Spiradenomas can occur in Brooke-Spiegler syndrome, which manifests withcylindromas, spiradenomas, and trichoepitheliomas. In this syndrome, lesions can have combined features of both cylindromas and spiradenomas.[5, 6]
Pathophysiology
A defective tumor suppressor gene is believed to result in the development of spiradenomas. In Brooke-Spiegler syndrome, of which spiradenomas are a manifestation, the defective gene is the CYLD gene on chromosome 9. Work remains to be performed on the genetic defect causing isolated and sporadic spiradenomas. The CYLD seems to be a hot spot of mutations as novel mutations continue to be reported.[7]
The expression of p53 in malignant spiradenomas seems to be increased.
The cells of origin of spiradenomas appear to have apocrine and trichoepitheliomatous differentiation, ie, they have complex hair follicle (folliculosebaceous apocrine) differentiation rather than eccrine differentiation.
In cases of linear/zosteriform/nevoid/blaschkoid multiple spiradenomas, an abnormal clone arising during embryogenesis is postulated to produce the multiple abnormal cells that result in such spiradenomas.
In a cytogenetic study, Dijkhuizen et al[8] found a spiradenoma and 2 lymph node metastases, with a growth pattern and microscopic appearance typical for benign spiradenoma, a 46,XY-5,del(16)(q22),+mar(t(?;5)(?::5q13----5qter)) karyotype.
These similar genetic defects seem to support a relationship between the chromosomal abnormalities and the clinical malignant action of this benign-appearing neoplasm.
Brooke-Spiegler syndrome: report of a case with combined lesions containing cylindromatous, spiradenomatous, trichoblastomatous, and sebaceous differentiation.
Source
Sikl's Department of Pathology, Charles University, Medical Faculty Hospital, Pilsen, Czech Republic.
Abstract
Brooke-Spiegler syndrome is an autosomal dominantly inherited disease with predisposition to cutaneous adnexal neoplasms, most commonly cylindromas and trichoepitheliomas. We report a patient in whom 11 lesions were removed from the scalp and face for various reasons over a period of 3 years. The histopathological survey revealed a plethora of benign adnexal neoplasms showing apocrine, follicular, and sebaceous differentiation occurring independently and conjointly. The histopathological spectrum in our patient included cylindromas, spiradenomas, trichoepitheliomas, small nodular trichoblastomas, and lymphadenomas. Many lesions had hybrid features of two or more neoplasms. By far the most common composite tumor was spiradenocylindroma. Some spiradenocylindromas demonstrated prominent sebaceous or trichoblastomatous differentiation or both. We suggest the terms "sebaceous spiradenocylindroma" and "trichospiradenocylindroma" for these lesions. The occurrence of sebaceous and trichoblastic differentiation in spiradenocylindromas is a further proof that spiradenoma and cylindroma are not eccrine tumors but neoplasms of the folliculosebaceousapocrine unit.
Expression of stem-cell markers (cytokeratin 15 and nestin) in primary adnexal neoplasms-clues to etiopathogenesis.
Mahalingam M, Srivastava A, Hoang MP.
Department of Dermatology, Boston University School of Medicine, MA, USA.
Abstract
BACKGROUND:
The overlap in histopathologic features and immunoprofile of eccrine and apocrine neoplasms confounds basic issues relating to lineage of these entities.
METHODS:
We evaluated expression of follicular stem-cell markers, cytokeratin (CK) 15 and nestin, in 78 benign and 23 malignant adnexal neoplasms.
RESULTS:
CK15 and nestin expression were noted in 39 of 78 (50%) and 36 of 78 (46%) cases in the benign group, respectively (8 cutaneous mixed tumor, 10 hidradenoma papilliferum, 9 apocrine cystadenoma, 11 cylindroma and/or spiradenoma, and 9 poroma/dermal duct tumor). CK15 and nestin expression were noted in 11 of 23 (48%) and 7 of 23 (30%) cases in the malignant group, respectively (6 microcystic adnexal carcinoma, 7 porocarcinoma, and 9 eccrine carcinoma). Except 1, both markers were negative in 4 syringocystadenoma papilliferum, 10 hidradenoma, 1 syringofibroadenoma, 10 syringoma, 1 eccrine adenoma, 8 poroma/dermal duct tumor, 5 eccrine hidrocystoma, and 1 apocrine carcinoma.
CONCLUSIONS:
Given that follicular germinative cells give rise to the folliculosebaceous apocrine unit, expression of CK15 and nestin in the majority of cutaneous mixed tumor, hidradenoma papilliferum, apocrine cystadenoma, and cylindroma/spiradenoma is suggestive of an apocrine origin/differentiation of these neoplasms. Reinforcing this and a novel finding of our study is the preferential expression of nestin in myoepithelial cells of these lesions.
-
本帖最后由 TK1905 于 2012-03-07 21:12:51 编辑
鉴别转移癌不用IKH-4还有更好的方法:
Mod Pathol.
2010 May;23(5):713-9. Epub 2010 Feb 26.
The diagnostic utility of immunohistochemistry in distinguishing primary skin adnexal carcinomas from metastatic adenocarcinoma to skin: an immunohistochemical reappraisal using cytokeratin 15, nestin, p63, D2-40, and calretinin. Mahalingam M, Nguyen LP, Richards JE, Muzikansky A, Hoang MP.
Source Dermatopathology Section, Department of Dermatology, Boston University School of Medicine, Boston, MA 02114, USA.
Abstract
Often the distinction of primary adnexal carcinoma from metastatic adenocarcinoma to skin from breast, lung, and other sites can be a diagnostic dilemma. Current markers purportedly of utility as diagnostic adjuncts include p63 and D2-40; however, their expression has been demonstrated in 11-22% and 5% of metastatic cutaneous metastases, respectively. Both cytokeratin (CK) 15 and nestin have been reported as follicular stem cell markers. We performed CK15 and nestin, as well as previously reported stains (such as p63, D2-40, and calretinin) on 113 cases (59 primary adnexal carcinomas and 54 cutaneous metastases). Expressions of p63, CK15, nestin, D2-40, and calretinin were observed in 91, 40, 37, 44, and 14% of primary adnexal carcinoma, respectively, and in 8, 2, 8, 4, and 10% of cutaneous metastases, respectively. p63 appeared to be the most sensitive marker (with a sensitivity of 91%) in detecting primary adnexal carcinomas. CK15 appeared to be the most specific marker with a specificity of 98%. Using chi(2) analysis, statistically significant P-values (<0.05) were observed for p63, CK15, nestin, and D2-40 in the distinction of primary adnexal carcinoma versus cutaneous metastases. In logistic regression and stepwise selection for predicting a primary adnexal carcinoma, statistical significance was observed for p63, CK15, and D2-40 (P-values: <0.001, 0.0275, and 0.0298, respectively) but not for nestin (P-value=0.4573). Our study indicates that diagnostic sensitivity and specificity are significantly improved using a selected panel of immunohistochemical markers, including p63, CK15, and D2-40. Positive staining with all three markers argues in favor of a primary cutaneous adnexal neoplasm.
- Registry of Soft Tissue and Skin Tumors, Šikls Department of Pathology, Charles University, Pilsen, Czech Republic
- Received 1 December 1995. Revised 15 April 1996. Available online 3 November 2011.
- Author: Noah S Scheinfeld, MD, JD, FAAD; Chief Editor: Dirk M Elston, MD
关于名称:小汗腺螺旋腺癌(Eccrine spiradenocarcinoma)有很多类似名称,恶性螺旋腺瘤(malignant spiradenoma)、螺旋腺瘤恶性转化(The malignant transformation of spiradenoma)、螺旋圆柱癌(spiradenocylindrocarcinoma)、起源于相关腺瘤的导管癌、癌在圆柱瘤和或螺旋腺瘤中等等。
螺旋腺瘤或癌一定是小汗腺起源吗?楼上有网友建议用IKH-4(这个标记本人不熟悉)证明本例是否为小汗腺起源,我觉得没有必要,因为小汗腺螺旋腺癌这个诊断专有名词可能是个误称,有很多文献报道螺旋腺瘤或它对应的癌不一定是小汗腺分化或起源,一部分被证实是大汗腺分化或起源,所以前面加个小汗腺或强调是小汗腺起源没有多大意义。引:
Spiradenoma Associated with Apocrine Adenoma Component
We present a case of spiradenoma associated with an apocrine adenoma component. The transitions between the spiradenoma and apocrine adenoma components were gradual. It could be observed that the small dark cells seen at the peripheries of the cell nodules of the spiradenoma component were replaced by the peripheral flat myoepithelial cell layer in the apocrine component. Similarly, the large pale cells within the centers of the cell nodules of the spiradenoma component were replaced by the brightly eosinophilic secretory cells with decapitation secretion in the apocrine component of the tumor. The reported case proves that at least some spiradenomas are tumors with distinct apocrine instead of eccrine differentiation
Spiradenoma
The histogenesis of spiradenomas remains in question, but many lesions demonstrate apocrine differentiation. The term eccrine spiradenoma may join the list of other misnomers in dermatology
本例形态学见恶性转化的导管上皮胞浆非常丰富,嗜酸性、核空泡状,见显著中位核仁,导管成分像前述的形态学特征说不定、就是大汗腺导管癌呢
关于:皮下局灶毛源性病变。个人认为那里够不上毛囊皮脂腺囊性错构瘤。病变上皮不是毛囊漏斗部,也没有显著的囊性扩张,皮脂腺分离与毛上皮无关联。典型结构不是这样。相反我认为那残余的毛结构可能是基底细胞样毛囊错构瘤,但这个不是重点,重点是汗腺的病变。
关于IHC有补充:螺旋腺瘤典型的特征就是有3种细胞,胞浆淡染的体积较大的导管上皮细胞(亮细胞)、导管上皮细胞外周的体积小的染色深的基底样细胞(暗细胞Dark cell),还有就是间质背景散在的小淋巴细胞,据研究都说是T细胞,表达CD3。组织结构低倍结节状、多结节状,高倍可见导管结构(亮细胞排列而成)、间质可因为发病时间长短、外伤等呈现出或硬化、或出血、或囊性变,以至于有时候镜下形态像血管球瘤、血管瘤、淋巴管瘤。螺旋腺瘤认识清楚了诊断螺旋腺癌也相对容易了,有良恶过渡区就很容易诊断,没有过渡区那就是疑难病例,幸好本例很典型,有明显良恶2种成分过渡
其它标记:CEA导管上皮表达,ER可以局灶阳性,P53在恶性转化的区域呈现出强表达,非恶性区阴性,Ki-67也是。PAS染基底膜样物。CD3证实背景淋巴细胞是有用的。
晕倒,我建议您结合本例的图像再看看你的英文部分,请您指点本例那些图中可见顶浆分泌?我想我所指的是本例可以做免疫组化证明小汗腺起源,而你所要表达的是:不是所有的病例都是来源于小汗腺!完全是两码事情,看似有理的论据,貌似经不起推敲呀,既然是读片俺就是就本病例发表看法,不是在准备论文答辩,不管对与错,呵呵这种学术氛围很好!在我们科里是很难见到的!
ps:这篇文章应该是96年发在pathology research and practice上的文章,查了一下
- Registry of Soft Tissue and Skin Tumors, Šikls Department of Pathology, Charles University, Pilsen, Czech Republic
- Received 1 December 1995. Revised 15 April 1996. Available online 3 November 2011.
- Author: Noah S Scheinfeld, MD, JD, FAAD; Chief Editor: Dirk M Elston, MD
关于名称:小汗腺螺旋腺癌(Eccrine spiradenocarcinoma)有很多类似名称,恶性螺旋腺瘤(malignant spiradenoma)、螺旋腺瘤恶性转化(The malignant transformation of spiradenoma)、螺旋圆柱癌(spiradenocylindrocarcinoma)、起源于相关腺瘤的导管癌、癌在圆柱瘤和或螺旋腺瘤中等等。
螺旋腺瘤或癌一定是小汗腺起源吗?楼上有网友建议用IKH-4(这个标记本人不熟悉)证明本例是否为小汗腺起源,我觉得没有必要,因为小汗腺螺旋腺癌这个诊断专有名词可能是个误称,有很多文献报道螺旋腺瘤或它对应的癌不一定是小汗腺分化或起源,一部分被证实是大汗腺分化或起源,所以前面加个小汗腺或强调是小汗腺起源没有多大意义。引:
Spiradenoma Associated with Apocrine Adenoma Component
We present a case of spiradenoma associated with an apocrine adenoma component. The transitions between the spiradenoma and apocrine adenoma components were gradual. It could be observed that the small dark cells seen at the peripheries of the cell nodules of the spiradenoma component were replaced by the peripheral flat myoepithelial cell layer in the apocrine component. Similarly, the large pale cells within the centers of the cell nodules of the spiradenoma component were replaced by the brightly eosinophilic secretory cells with decapitation secretion in the apocrine component of the tumor. The reported case proves that at least some spiradenomas are tumors with distinct apocrine instead of eccrine differentiation
Spiradenoma
The histogenesis of spiradenomas remains in question, but many lesions demonstrate apocrine differentiation. The term eccrine spiradenoma may join the list of other misnomers in dermatology
本例形态学见恶性转化的导管上皮胞浆非常丰富,嗜酸性、核空泡状,见显著中位核仁,导管成分像前述的形态学特征说不定、就是大汗腺导管癌呢
关于:皮下局灶毛源性病变。个人认为那里够不上毛囊皮脂腺囊性错构瘤。病变上皮不是毛囊漏斗部,也没有显著的囊性扩张,皮脂腺分离与毛上皮无关联。典型结构不是这样。相反我认为那残余的毛结构可能是基底细胞样毛囊错构瘤,但这个不是重点,重点是汗腺的病变。
关于IHC有补充:螺旋腺瘤典型的特征就是有3种细胞,胞浆淡染的体积较大的导管上皮细胞(亮细胞)、导管上皮细胞外周的体积小的染色深的基底样细胞(暗细胞Dark cell),还有就是间质背景散在的小淋巴细胞,据研究都说是T细胞,表达CD3。组织结构低倍结节状、多结节状,高倍可见导管结构(亮细胞排列而成)、间质可因为发病时间长短、外伤等呈现出或硬化、或出血、或囊性变,以至于有时候镜下形态像血管球瘤、血管瘤、淋巴管瘤。螺旋腺瘤认识清楚了诊断螺旋腺癌也相对容易了,有良恶过渡区就很容易诊断,没有过渡区那就是疑难病例,幸好本例很典型,有明显良恶2种成分过渡
其它标记:CEA导管上皮表达,ER可以局灶阳性,P53在恶性转化的区域呈现出强表达,非恶性区阴性,Ki-67也是。PAS染基底膜样物。CD3证实背景淋巴细胞是有用的。
其实前面有人提到转移性腺癌的鉴别诊断,俺觉得用IKH-4也能对其进行很好的鉴别!
对于 13 楼 TK1905哥们提到的
本例形态学见恶性转化的导管上皮胞浆非常丰富,嗜酸性、核空泡状,见显著中位核仁,导管成分像前述的形态学特征说不定、就是大汗腺导管癌呢
本人有不同观点,重看了图片发现良性腺体与恶性腺体之间貌似有过渡,交叉分部,提示两种腺体可能来源相同,因此首先考虑小汗腺来源的,如果按照上面哥们的看法提出的鉴别诊断的话,我觉得更加有必要做IKH-4了,因为这个不仅能够转移性癌,而且能够鉴别大小汗腺来源肿瘤!如果+那就还是小汗腺来源的了!- 的情况俺现在还不考虑,- 的话真就不好搞了,不过我坚持认为IKH-4做出来应该是阳性!
-
本帖最后由 勇敢一点 于 2012-03-07 22:10:28 编辑
诊断结果:考虑皮脂腺癌
诊断依据:根据镜下特点,先为肿物定性。
1.临床症状为无痛性多发肿物,位于颈肩背部
2.低倍镜下,见到肿瘤主要呈不规则的小叶状结构,其中见显著增生的血管组织;
3.高倍镜下,肿瘤细胞主要包括两种类型,一种为分化较好的泡沫状细胞,胞核卵圆形,多位于细胞中央,胞浆淡染;一种为分化 较差的肿瘤细胞,胞浆嗜碱性为主,胞核异型性明显,可见核分裂像。
鉴别诊断:1 螺旋腺瘤及螺旋腺癌
2 恶性混合瘤
免疫组化;CK广,EMA ,Ki67,AR等

- 真正的美玉总是存在瑕点,哪怕是极其微小的;只有赝品才美得让人无可挑剔.