| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
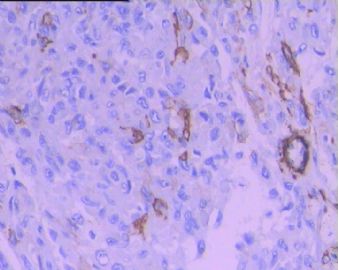
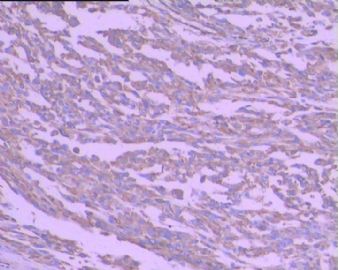
- 左足背肿瘤(免疫组化图像已上传)
| 姓 名: | ××× | 性别: | 女 | 年龄: | 60 |
| 标本名称: | 左足背肿瘤 | ||||
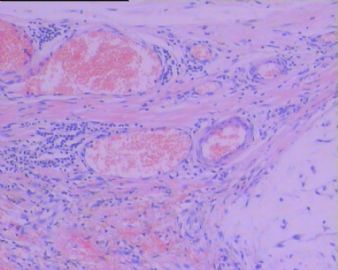
| 简要病史: | 左足背肿块一年,近期生长加快,有疼痛。手术所见:肿块位于肌腱深层,肌间隙肿块不规则形,肉样。 | ||||
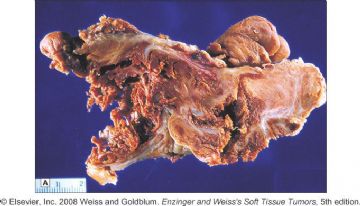
| 肉眼检查: | 肿块4.5*3.5*2.2厘米,表面结节状,切面部分灰白粘液感,部分暗红结节状,局部棕黄结节状,不同颜色区域分界较清,拼图样。肿块界清。 | ||||
-
本帖最后由 于 2010-07-13 17:44:00 编辑
-
本帖最后由 于 2010-07-14 01:06:00 编辑
- Fletcher, C.D.M., Unni, K.K. and Mertens, F. Pathology and genetics. Tumours of Soft Tissue and Bones. World Health Organization Classification of Tumours. IARC press, Lyon, 2002.
- Goldblum JR, Weiss SW. Benign soft tissue tumors and pseudotumors of miscellaneous type. In: Enzinger and Weiss's Soft tissue tumors. 4th ed. St Louis, Mo: Mosby; 2001.
- Hatano H, Ogose A, Hotta T, et al. Treatment of myxoid liposarcoma by marginal or intralesional resection combined with radiotherapy. Anticancer Res. 2003;23(3C):3045-9.
- Kapila K, Ghosal N, Gill SS, Verma K. Cytomorphology of lipomatous tumors of soft tissue. Acta Cytol. 2003;47(4):555-62.
- Kempson RL, Fletcher CDM, Evans HL, Hendrickson MR, Sibley RK. Atlas of Tumor Pathology: Tumors of Soft Tissue. Washington, D.C.: Armed Forces Institute of Pathology; 2001.
- Lin CN, Chou SC, Li CF, et al. Prognostic factors of myxofibrosarcomas: implications of margin status, tumor necrosis, and mitotic rate on survival. J Surg Oncol. 2006;15;93(4):294-303.
- Meis-Kindblom JM, Enzinger FM. Color Atlas of Soft Tissue Tumors. St Louis, Mo: Mosby-Year Book; 1996.
形态学真的是让人欢喜让人忧,比较Dr.笃行者者的这例,真的是不好分辨,提出粘液脂肪肉瘤的鉴别
http://www.ipathology.cn/forum/forum_display.asp?keyno=252438
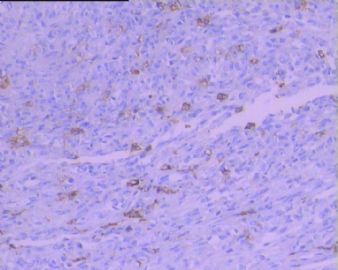
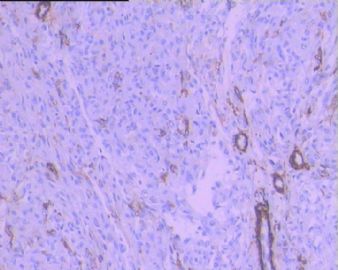
以下为脂肪肉瘤的免疫组化参考,s-100的阴性是否可以否定该瘤。
Positive stains
=========================================================================
● MDM2 and CDK4 (both together are sensitive and specific, AJSP 2005;29:1340)
● S100 (adipocytes in 2/3 of cases)
● CD34 (some spindle cells)
● usually p16 (Appl Immunohistochem Mol Morphol 2009;17:51)
Negative stains
=========================================================================
● HMB45
2010— January Case of the Month Updated January 11, 2010 CLINICAL SUMMARY: SOFT TISSUE View case with: PC users: ImageScope First-time use of ImageScope? * Download (required) ImageScope offers many additional features including: MAC/PC Users: WebViewer After reading the summary, try answering the three related multiple-choice questions below. A 48-year-old woman presented with a large painless thigh mass, which was excised. Grossly, the mass was a well circumscribed,lobulated 17.7 x 15.2 x 11.8 cm unencapsulated tumor with a slightly yellow and gelatinous cut surface and focal areas of hemorrhage. Archive Case and Diagnosis: This case first appeared as Performance Improvement Program in Surgical Pathology (PIP) 2007, Case 1 and is a myxoid liposarcoma. Criteria for Diagnosis and Comments: This is an example of myxoid liposarcoma, which is the most common subtype of liposarcoma. It is a variably cellular neoplasm that shows three characteristic microscopic features: lipoblasts in various stages of differentiation, a delicate capillary network, and an abundant myxoid matrix. Mast cells are also commonly observed. The proliferating cells of myxoid liposarcoma are relatively uniform lipoblasts that are most easily identified at the tumor periphery. In their earliest forms, they may appear as primitive mesenchymal cells but when mature they most often have a signet-ring morphology. They are occasionally multinucleate and are often S-100 positive. Although the tumor may grow rather aggressively, mitoses range from absent to very few. The main predictive factor for metastatic potential of this tumor is instead overall cellularity. Cellular areas consist of closely spaced primitive appearing round cells with a high N:C ratio and conspicuous nucleoli. Cytoplasm may be scant or relatively abundant. Myxoid stroma is typically absent in these areas. Such areas were previously termed "round cell liposarcoma" but it is now recognized that myxoid and round cell liposarcomas represent a histologic continuum with both patterns sharing a t(12;16)(q13;p11) translocation. The cellular/round cell areas are thought to represent the poorly differentiated end of the histologic spectrum. The presence of a significant round cell component, defined as greater than 5% in the current WHO classification, has been associated with an unfavorable outcome. The vascular component of this tumor is quite characteristic. It is a delicate plexiform network composed of narrow thin walled vessels. It is more prominent in neoplasms that retain their primitive characteristics and is less notable in those with a preponderance of maturing lipoblasts. Another unique vessel-related finding is the presence of hypocellular zones around small veins and arteries. The myxoid component contains glycosaminoglycans or mucopolysaccharides, which may be both extra and intracellular, and varies in both its amount and distribution. A colloidal iron stain will highlight hyaluronidase-sensitive myxoid material. There may be pooling of this material, imparting an almost cribriform or lacelike architectural pattern to the tumor. When this matrix is abundant it may also form cystic spaces filled with granular material. These "microcysts" can become quite large and architecturally complex. Their low power pattern is quite distinctive and has been described as pulmonary-edema like. Clinically, myxoid liposarcoma presents as a large painless mass arising in muscle or deep soft tissue. The peak incidence is in the fifth decades; this tumor rarely develops in individuals less than 20 years of age. Myxoid liposarcoma has a very strong predilection for the thigh but may also be found in the popliteal fossa, groin, and buttock region. Other locations are extremely uncommon. The standard of care is surgical excision with wide margins. Post-surgical recurrence is uncommon and is usually local. However, these low-grade tumors may metastasize, most commonly to the lung, retroperitoneum or bone. Intramuscular myxoma is another neoplasm comprised of uniform cells in a myxoid stroma but lacking the characteristic vascular network and lipoblasts of myxoid liposarcoma. Intramuscular myxoma is also paucicellular, substantially less cellular than the least cellular myxoid liposarcomas. Lipoblastoma is another tumor with delicate plexiform vasculature, a myxoid matrix, and small immature fat cells, a pattern that makes it almost histologically indistinguishable from myxoid liposarcoma. This tumor can also contain microcystic spaces, as found in myxoid liposarcoma. However lipoblastoma occurs almost exclusively in infants making this a very important clue in their distinction. Myxoid liposarcoma only rarely occurs prior to the age of twenty. Other distinguishing factors include the lobular architecture, lack of more cellular areas, and superficial location of lipoblastoma. Lipoblastomatosis, like lipoblastoma, also occurs within the first three years of life and twice as often in boys than girls. Lipoblastomatosis refers to more diffuse and deeper or infiltrative lesions that meet the histologic criteria for lipoblastoma. For this reason, this entity offers the same diagnostic dilemma as its subcutaneous and circumscribed counterpart, lipoblastoma and the same factors are used to distinguish this entity from myxoid liposarcoma. Myxoid chondrosarcoma is in the differential diagnosis of myxoid liposarcoma in that it also is a tumor comprised of uniform cells with a myxoid stroma. Rarely myxoid liposarcoma may also have chondroid differentiation. However myxoid chondrosarcoma has a lobulated architecture, with intervening fibrous septa, in which the tumor cells are typically at the periphery of the lobules. The characteristic lipoblasts and capillary network of the myxoid liposarcoma are not found in the myxoid chondrosarcoma. Myxoid dermatofibrosarcoma protuberans (DFSP), a locally aggressive tumor believed to be of fibroblastic origin, may have a myxoid background, as seen in myxoid liposarcoma; however, its cutaneous location helps distinguish this diagnostic entity. DFSP possesses a very characteristic storiform architectural pattern that is not present in myxoid liposarcoma. The storiform architecture may be lost in myxoid areas, but strong CD34 staining in DFSP differentiates it from myxoid liposarcoma. Myxoid malignant fibrous histiocytoma (myxofibrosarcoma/MFH), another aggressive tumor which may be associated with previous radiation exposure, also has a myxoid stroma and rich capillary network which may present a diagnostic challenge in distinguishing it from myxoid liposarcoma. The mucopolysaccharide containing cells of myxoid MFH may also be confused with the primitive lipoblasts of myxoid liposarcoma. To distinguish these entities it is important to note that the mucopolysaccharide vacuoles in myxoid MFH do not distort the nucleus and that the material within these vacuoles is of the same color and density as the background myxoid stroma. In myxoid liposarcoma the cytoplasmic vacuoles are clear and usually of the signet ring type pushing the nucleus eccentrically and indenting it. Myxoid MFH typically arises in subcutaneous tissue, a very uncommon site of myxoid liposarcoma and is also pleomorphic in contrast to the more uniform cells of myxoid liposarcoma. Finally, although the arborizing vascular network of myxoid MFH may be reminiscent of myxoid liposarcoma, it does not possess the characteristic hypocellular zones found around small vessels in myxoid liposarcoma. Myxoid MFH is immunoreactive for factor XIIIa and CD68 and negative for S-100 protein. Spindle cell lipoma is a benign circumscribed tumor characterized by an admixture of mature fat and collagen-forming spindle cells. This histologic variant of the common lipoma primarily occurs in middle-aged to elderly men with a male to female predominance of 9:1. Related Links • Case of the Month Overview • Case Archives
• Ability to view multiple slides
concurrently; synchronize
panning/zooming.
• Facility to author annotations.
• Capability to run analysis
algorithms, and display results.
• Modify image brightness,
contrast, color balance,
etc.
• Generally faster and more
responsive.
It may possess adipocytes that resemble signet ring cells and a myxoid stroma, which could be confused with those features of myxoid liposarcoma. However the rich vascular network of myxoid liposarcoma is not a feature of spindle cell lipoma, which additionally has coarse collagen and spindled cells with elongate nuclei. Finally the anatomic sites of these tumors are very different with the spindle cell lipoma favoring superficial locations of the back, neck, and shoulder.
• Performance Improvement
Program in Surgical Pathology
Author:
2007
Colleen Ann Murphy, MD
Berkshire Medical Center
Pittsfield, MA
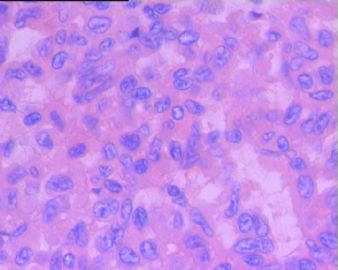
| 以下是引用学浅在2010-7-12 20:45:00的发言: 我初步考虑一种少见的肿瘤:粘液性炎症性纤维母细胞肉瘤。特点:肢端,结节状,可见炎症细胞,可见色素性绒毛状滑膜炎的区域,可见核仁明显的细胞(但似乎不太符合“病毒样细胞”)。 |
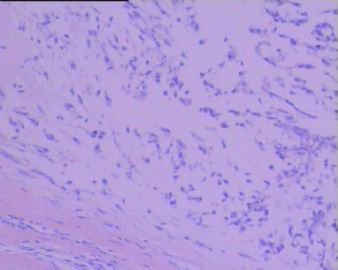
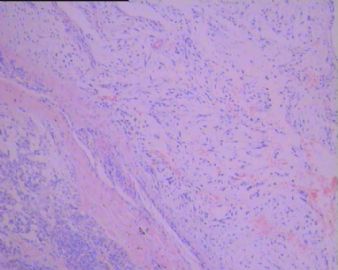
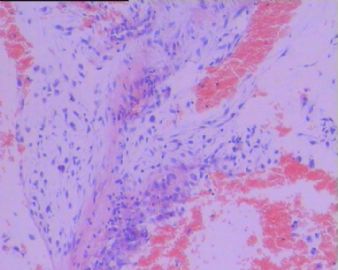
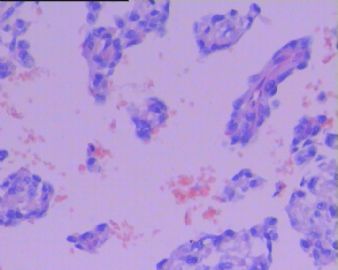
巨检:直径1-8cm,切面灰白色,纤维性和粘液区相间。
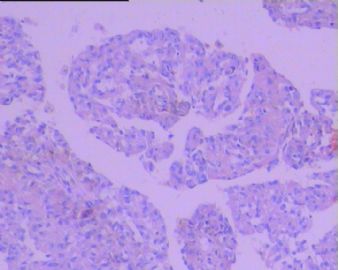
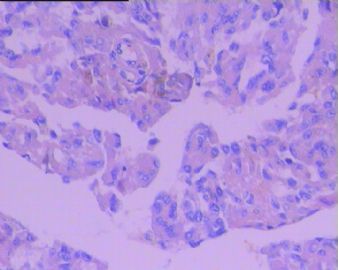
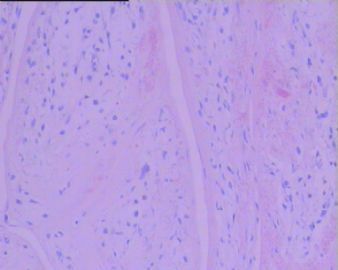
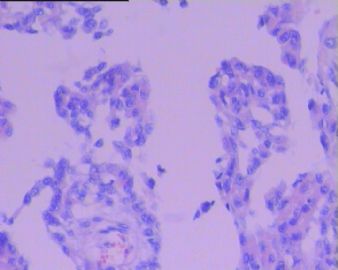
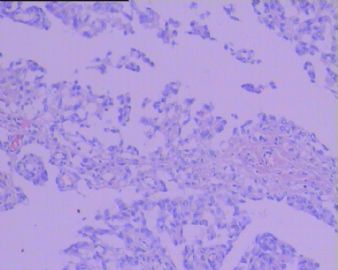
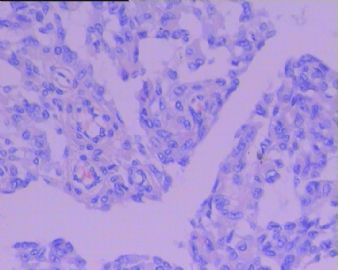
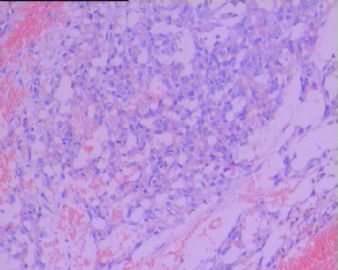
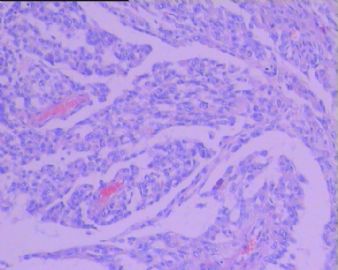
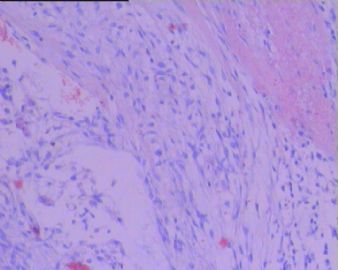
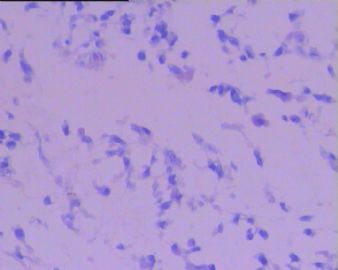
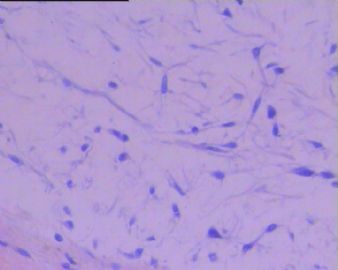
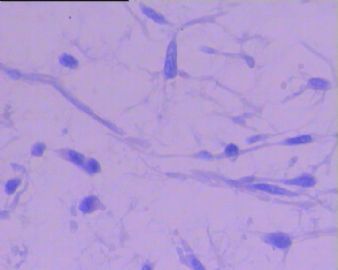
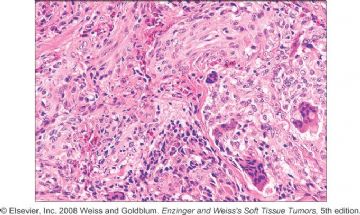
镜检:玻璃样和粘液样间质相间的背景中有大量急、慢性炎症细胞和巨噬细胞浸润,病变中有三种类型的肿瘤细胞:梭形细胞、神经节细胞样细胞和脂母细胞样细胞。
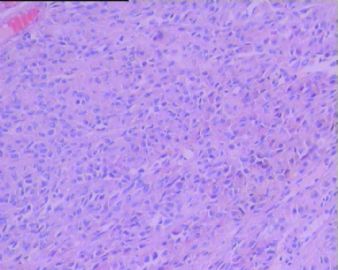
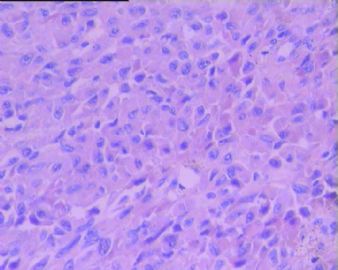
同意Dr.zhanglei意见。我也是首先考虑弥漫型腱鞘巨细胞瘤。这个肿瘤无论是从大体形态还是从组织结构及其细胞形态都看不出有明显恶性的形态学表现。
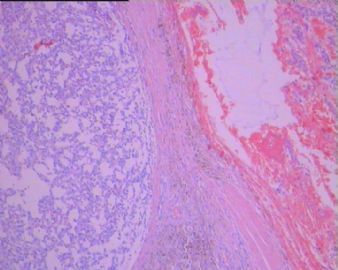
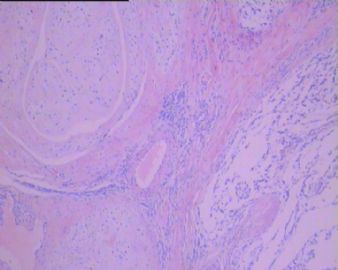
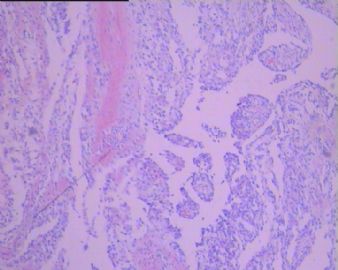
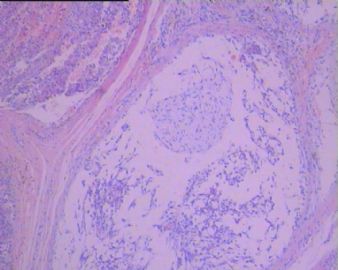
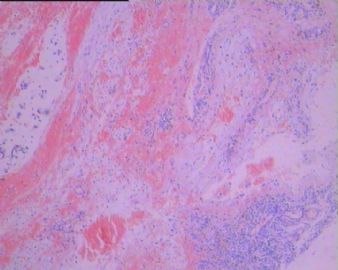
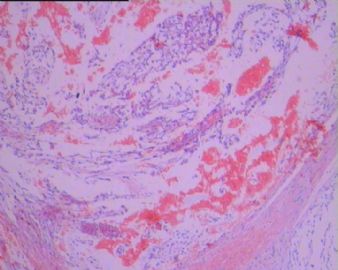
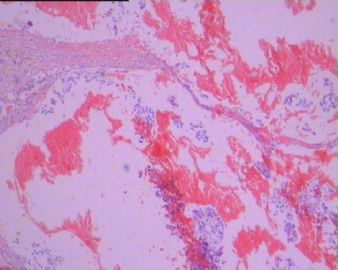
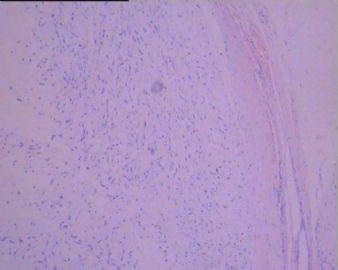
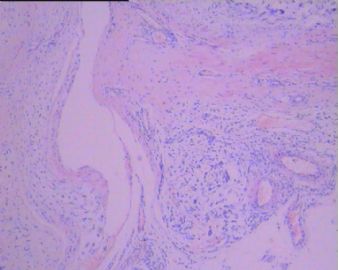
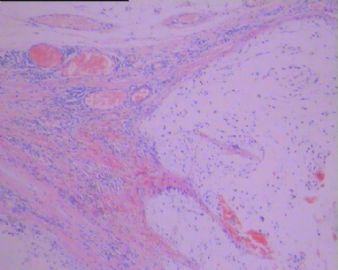
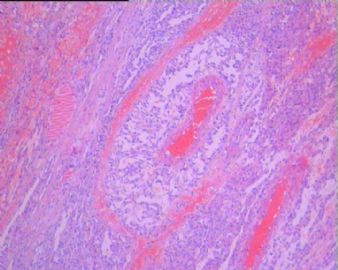
从大体上看呈多结节状,切面显示呈灰白、灰褐、灰黄色不同界清区域,看上去粘滑,可见暗褐色出血区域,有大片灰白浅黄色实性区。
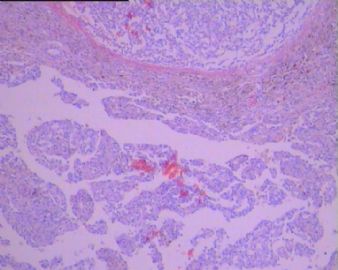
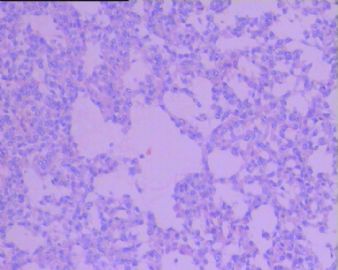
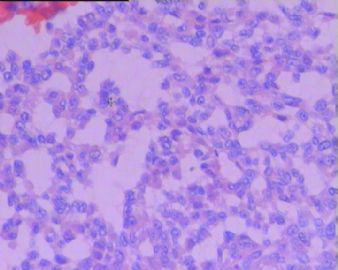
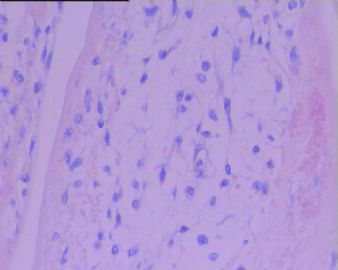
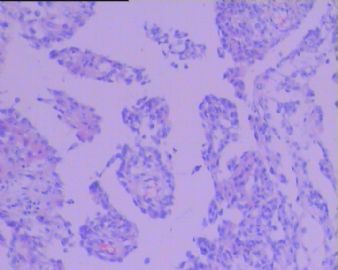
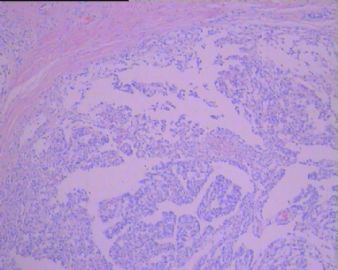
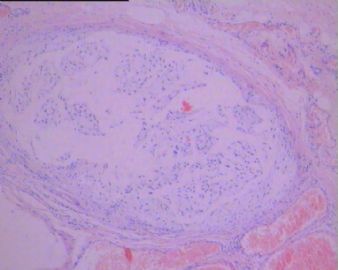
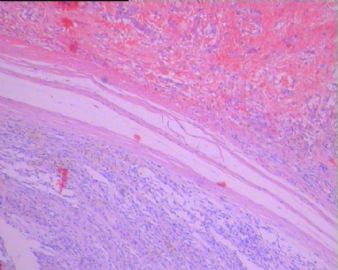
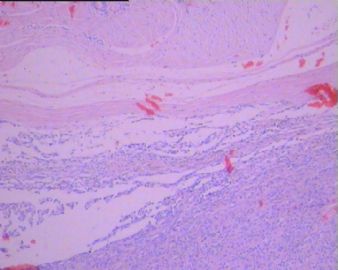
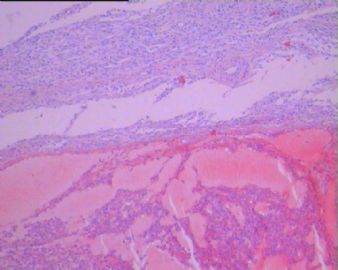
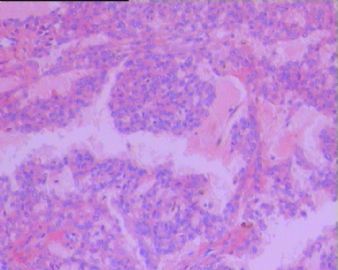
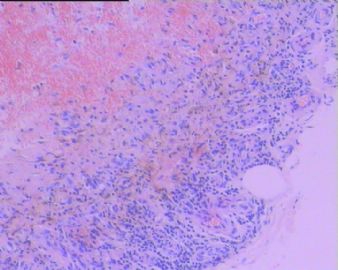
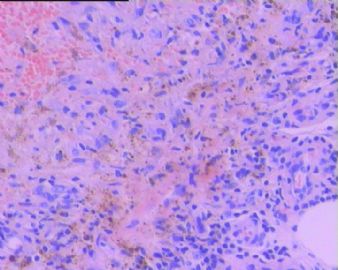
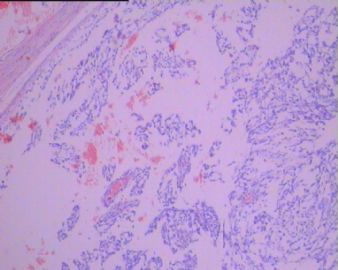
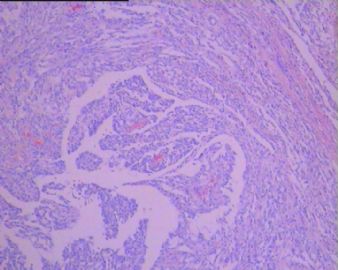
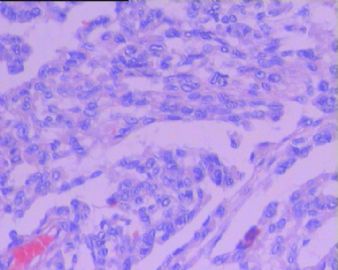
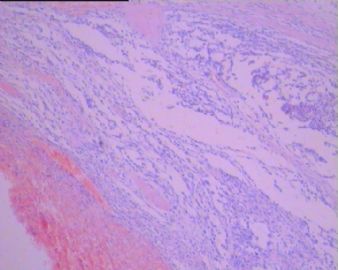
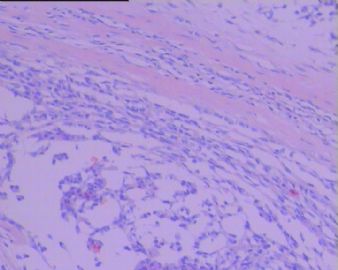
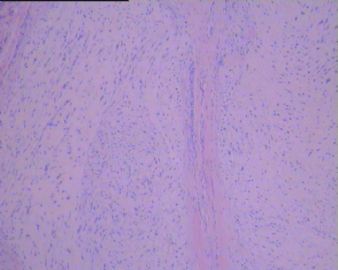
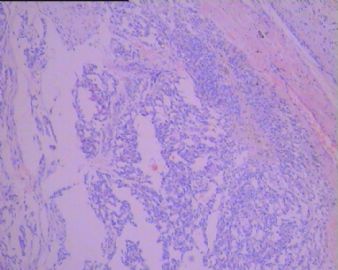
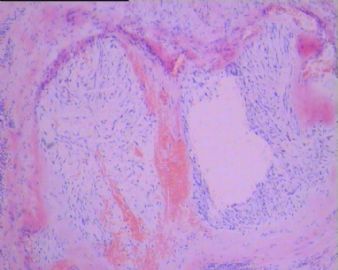
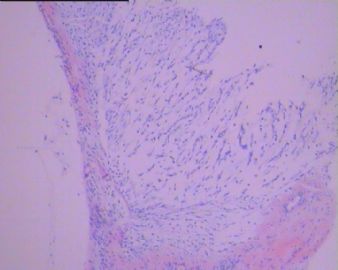
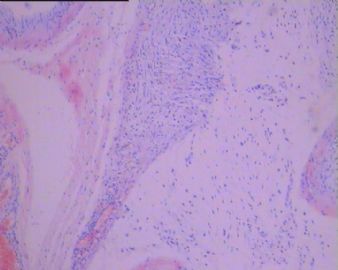
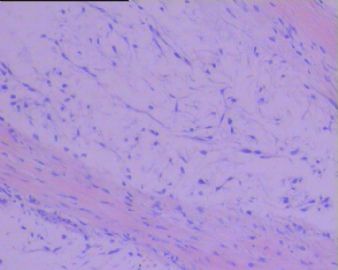
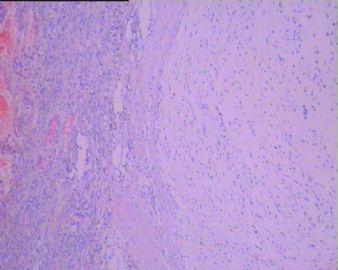
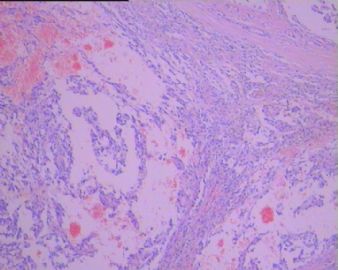
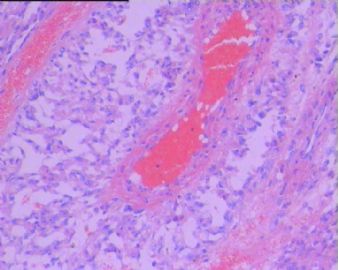
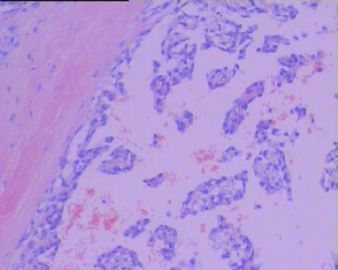
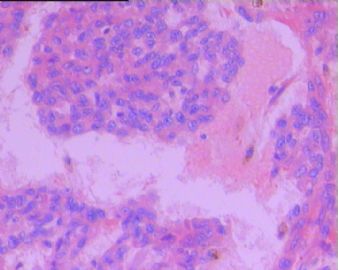
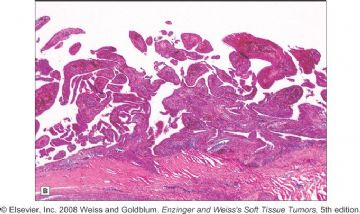
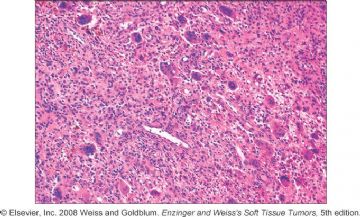
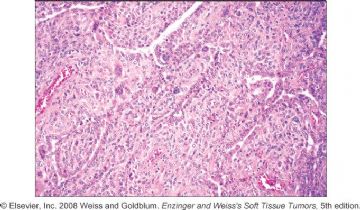
从镜下看,结节分叶状。结节边界清晰。部分结节富含粘液样基质(软骨样基质)。肿瘤主要由滑膜样细胞构成,多呈肥大的滑膜绒毛样结构。瘤细胞小圆形或卵圆形,咖啡豆样细胞核,异型性不是很明显。有的区域可见灶性含铁血黄素沉积。肿瘤边缘的结构类似滑膜结构,灶区富于血管。
总体下来,呈良性肿瘤特征,所以综合上述考虑为:弥漫型腱鞘巨细胞瘤。

- 王军臣
-
本帖最后由 于 2010-07-13 11:54:00 编辑
弥漫型腱鞘巨细胞瘤(diffuse-type giant cell tumor),旧称为色素性绒毛结节性滑膜炎。本病主要累及大关节及其附近的附属结构,以膝关节常见,依次为膝关节、髋关节,也可累及肩关节和肘关节,其它关节区也可见(脊柱关节等)。本例发生在足背部,邻近的大关节为踝关节和许多小关节。踝关节发生的少见。
诊断该病时,病史很重要。一般患者以青年女性多见,常主诉局部疼痛,病史相对较长。本例老年女性,比较特殊。老年女性不一定不发病。但考虑到局部细胞比较丰富,在弥漫型腱鞘巨细胞瘤前,加一个前缀或后缀“富于细胞”可能比较好。

- 王军臣
弥漫型腱鞘巨细胞瘤的预后一般较好,只有1/4的患者可能复发。需要注意的是:富于细胞的弥漫型腱鞘巨细胞瘤(增生性色素性绒毛结节性滑膜炎)与低度恶性滑膜肿瘤很难鉴别。本例由于发生在老年,而且局部细胞丰富,需要多取材观察有无侵袭、坏死和病理性核分裂存在,寻找有无恶变的依据。
弥漫型腱鞘巨细胞瘤恶变罕见,但有恶变的文献记载与报道。究竟是在弥漫型腱鞘巨细胞瘤基础上恶变还是与之无关的情况下后发的恶性滑膜源性肿瘤?由于病例少,暂无定论。
金主任列出了系列鉴别诊断,请参考相关肿瘤特征予以鉴别。
总之,本例倾向富于细胞的弥漫型腱鞘巨细胞瘤。
需要多取材观察并结合影像学鉴别是否恶变。即便恶变了,也只是低度恶性的,只要切净了,除了复发可能之外,预后比较好。

- 王军臣
-
本帖最后由 于 2010-07-14 22:08:00 编辑
本病例大体标本特点:
1)富含粘液的多个囊腔(粘液瘤?);
2)大片灰白色实质性肿瘤(良性-交界性-恶性肿瘤?);
3)小块黄褐色实质性区域(腱鞘巨细胞瘤?);
显然,这与典型的弥漫性腱鞘巨细胞瘤(色素性绒毛结节性滑膜炎)不同。临床上病人无长期滑膜炎病史。形态学上细胞并不很丰富;大量粘液软骨样组织也不能用滑膜巨细胞瘤来解释。
请比较 图1(本病例)和 经典教科书上的弥漫性腱鞘巨细胞瘤 图2-8(Weiss & Enzinger soft tissue tumors, 5th Ed, 2008,p778-780)

- xljin8
| 以下是引用xljin8在2010-7-13 7:46:00的发言:
本病例大体标本特点: 1)富含粘液的多个囊腔(粘液瘤?); 2)大片灰白色实质性肿瘤(良性-交界性-恶性肿瘤?); 3)小块黄褐色实质性区域(腱鞘巨细胞瘤?);
显然,这与典型的弥漫性腱鞘巨细胞瘤(色素性绒毛结节性滑膜炎)不同。临床上病人无长期滑膜炎病史。形态学上细胞并不很丰富;大量粘液软骨样组织也不能用滑膜巨细胞瘤来解释。 |
 这个病例形态复杂,很难用某个单一肿瘤来解释。
这个病例形态复杂,很难用某个单一肿瘤来解释。
它会不会是两种软组织肿瘤的混合:富细胞性弥漫型腱鞘巨细胞瘤+关节旁粘液瘤?

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。