| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 有趣而罕见的肾脏肿瘤
-
本帖最后由 于 2010-07-19 17:48:00 编辑
| 以下是引用xljin8在2010-7-19 8:36:00的发言:
如果是肾透明细胞癌与类癌组合是世界第二例、如果是神经内分泌癌转移到肾透明细胞癌则有数例报道。但确实非常罕见。 请参考文献: 1)Bressenot A, et al. Composite renal cell carcinoma with clear cell renal cell carcinomatous and carcinoid tumoral elements: a first case report. J Clin Pathol. 2010;63:174-6. 2)Ulamec M, et al. Neuroendocrine breast carcinoma metastatic to renal cell carcinoma and ipsilateral adrenal gland. Pathol Res Pract. 2008;204:851-5.
|

- xljin8
-
healthyguard 离线
- 帖子:9
- 粉蓝豆:1
- 经验:9
- 注册时间:2009-05-16
- 加关注 | 发消息
| 以下是引用xljin8在2010-7-19 9:07:00的发言:
|
J Clin Pathol 2010;63:174-176 doi:10.1136/jcp.2009.070292
· Case report
Composite renal cell carcinoma with clear cell renal cell carcinomatous and carcinoid tumoral elements: a first case report
1. A Bressenot1,
2. C Delaunay1,
3. G Gauchotte1,
5. G Boudrant3,
6. K Montagne1
+ Author Affiliations
1. 1Department of Pathology, Hopital de Brabois, CHRU Nancy, Nancy, France
2. 2Department of Radiology, Hopital de Brabois, CHRU Nancy, Nancy, France
3. 3Department of Urology, Hopital de Brabois, CHRU Nancy, Nancy, France
1. Correspondence to Dr A Bressenot, Service d'Anatomie et de Cytologie Pathologiques, CHU de Brabois, Allée du Morvan, 54511 Vandoeuvre-lès-Nancy Cedex, France; a.bressenot@chu-nancy.fr
· Accepted 1 September 2009
Abstract
Renal endocrine tumours are extremely rare, and carcinoid tumoral elements in renal cell carcinoma have never been reported. This is the first report of a composite renal cell carcinoma containing a clear cell renal cell carcinoma associated with carcinoid tumoral elements, in a patient with synchronous metastatic disease. In the absence of specific radiological and clinical manifestations, typical morphological features as well as an immunostaining profile of neuroendocrine differentiation were identified by microscopy. Secondary nodal and liver localisations were characterised by carcinoid elements only. Despite antiangiogenic therapy, liver metastasis progressed, suggesting that adjuvant therapy cannot be based on the presence of the clear cell renal cell carcinoma component. In this context, extensive tissue sampling is recommended to reveal the endocrine component that is the most aggressive element of such a composite carcinoma.
Clear cell renal cell carcinoma (RCC) is the most common tumour arising from the epithelium of renal tubules.1 Renal neuroendocrine tumours are considered distinct entities in the 2004 World Health Organization classification1 scheme, with histological features identical with those of endocrine tumours whatever their anatomic sites.2 The extreme rarity of renal endocrine tumours explains in part why the association between clear cell RCC and neuroendocrine tumoral elements has not previously been reported. We describe here, for the first time, a case of mixed clear cell RCC and well-differentiated neuroendocrine tumour.
Case report
A patient was admitted to our hospital for biological cholestasis. A solid mass in the right kidney and a metastatic liver lesion were identified by abdominal ultrasonography. Additional evaluation with CT revealed a 6 cm solid heterogeneous lesion of the right kidney, a metastatic liver lesion and multiple osteoblastic vertebral lesions (figure 1A). A right radical nephrectomy and a surgical biopsy of the liver lesion were performed. No manifestations suggestive of carcinoid syndrome were noticed. Blood neuron-specific enolase and chromogranin levels were normal. The patient received antiangiogenic treatment as adjuvant therapy. Six months later, the follow-up revealed an increase in the size of the liver metastasis.
View larger version:
Figure 1
(A) CT scan showing a 6 cm solid heterogeneous lesion of the right kidney located at the inferior pole (thin arrow) with osteoblastic vertebral lesion (thick arrow). (B) Gross morphology of nephrectomy specimen showing a well-circumscribed tumour, located at the inferior pole, with a heterogeneous aspect with white and yellow areas. Original magnification ×1.
Macroscopic features
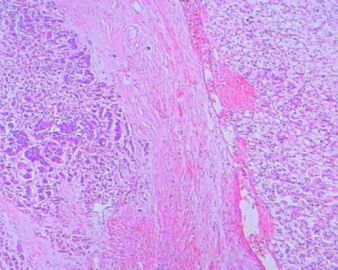
Examination of the nephrectomy specimen showed a well-circumscribed 5×4×3.5 cm tumour, located at the inferior pole of the kidney. A heterogeneous aspect due to white and yellow areas throughout the tumour was observed. The mass was confined in a discrete fibrous capsule without invasion into the perinephric soft tissue or sinus fat (figure 1B).
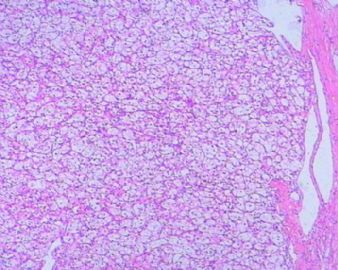
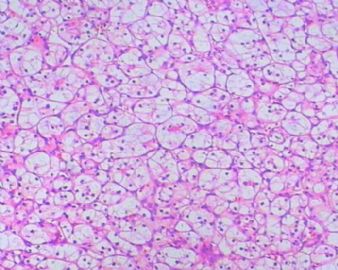
Microscopic features
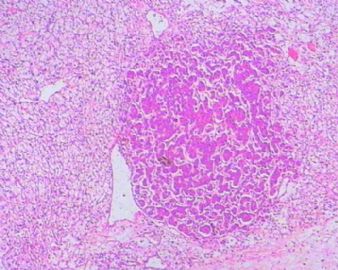
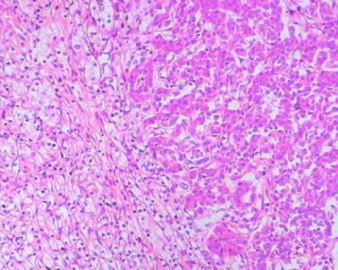
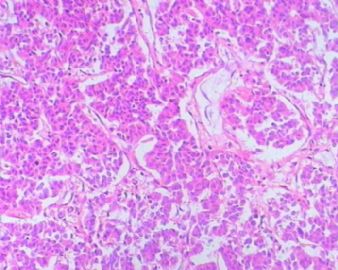
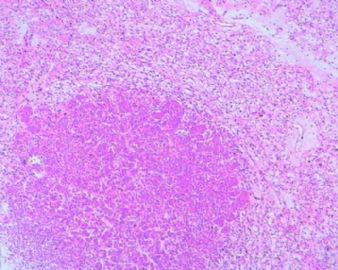
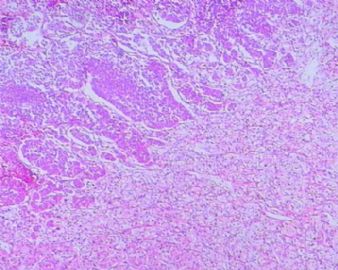
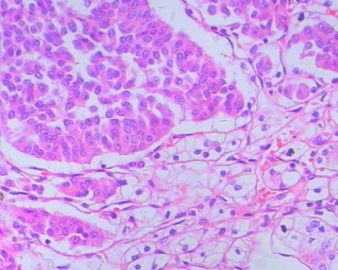
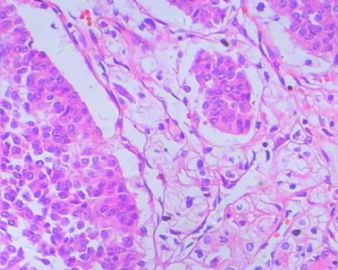
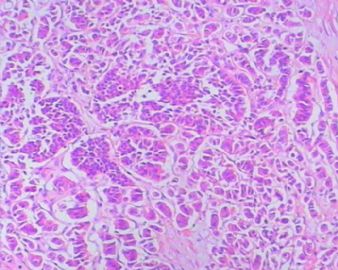
The tumour displayed two components: the major part of the tumour (90% of the tumoral mass) consisted of a classical clear cell RCC with tubules, cords or sheets of epithelial structures lined with clear cells of Fuhrman grade 2. This clear cell part was intimately mixed with another element (10% of the tumoral mass). The latter was characterised by packed cords and trabeculae of neoplastic cells within a minimal stroma. The nuclei were elongated and oval, situated along the perpendicular axis to the long axis of the cords and trabeculae. The nuclear chromatin was finely granular and dispersed with inconspicuous nucleoli (figure 2A,B) No mitoses/10 high-power fields (HPF) was observed in endocrine foci. Absence of necrosis was noticed. Examination of the liver biopsy specimen and one of the renal hilar lymph nodes revealed metastatic involvement exclusively consisting of well-differentiated endocrine tumoral elements. Tumour, node, metastases (TNM) staging was noted T1bN1M1.
View larger version:
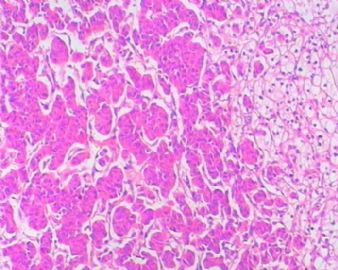
Figure 2
Light microscopy findings on the tumour. The tumour was composed of clear cell renal cell carcinoma (left side of images) admixed with carcinoid tumoral elements (right side of images). H&E, original magnification (A) ×100, (B) ×400. (C) Carcinoid tumoral component shows strong reactivity with synaptophysin (original magnification ×100). (D) Clear cell RCC component was strongly positive for CD10 in contrast with endocrine elements (original magnification ×100).
Immunohistochemical examination confirmed the presence of two different tumoral constituents. The first was characterised by a typical immunoreactive profile of clear cell RCC including a positive expression of vimentin (V9; 1:6000; DakoCytomation, Trappes, France), CD10 (56C6; 1:20; Novocastra, Newcastle-upon-Tyne, UK), cytokeratin AE1AE3 (AE1AE3; 1:400; DakoCytomation), human epithelial membrane antigen (E29; 1:100; DakoCytomation) and an absence of endocrine markers. Conversely, the second part of the tumour displayed strong positivity for synaptophysin (SY38; 1:1500; DakoCytomation), CD56 (1B6; 1:40; Novocastra) and chromogranin A (LK2H10+PHE5; 1:1000; Neomarkers, Fremont, California, USA), and an absence of reactivity to EMA, vimentin and CD10 (figure 2C,D). Ki67 (MIB-1; 1:400; DakoCytomation) staining confirmed low proliferative activity in both epithelial constituents. Taken together, these observations are consistent with a mixed clear cell RCC and well-differentiated neuroendocrine tumour, the latter being classified as carcinoid tumour according to the 2004 World Health Organization classification.1
Discussion
RCC is composed of highly heterogeneous histological subtypes. The most common cases involve clear cell RCC, but several subtypes with different morphological features can be found.1 Endocrine tumours have been reported in a wide range of organs, most commonly lungs and gastrointestinal tract.3 They can occur in a pure form or be admixed with non-endocrine components, such as adenocarcinoma or squamous cell carcinoma.4 However, a kidney location is extremely rare.5 Moreover, their origin has been debated because enterochromaffin cells are not found in normal renal parenchyma.6 This may explain why the association of a renal neuroendocrine tumour with a clear cell RCC has not previously been reported. In the literature, there is only one case report of a renal composite carcinoma with endocrine elements consisting of an admixture of a chromophobe clear cell RCC with a small-cell endocrine carcinoma.4
In the present case report, preoperative diagnosis of the neuroendocrine part was not achieved, probably because, firstly, the patient did not present any manifestations of carcinoid syndrome and, secondly, CT failed to identify the mixed tumour pattern. Furthermore, gross morphological examination revealed typical features of clear cell RCC, without any suspicion of neuroendocrine differentiation. It is likely that the small size of the neuroendocrine tumoral islets explains the typical appearance of clear cell RCC. Finally, only a careful microscopic examination was able to detect the minor component of well-differentiated neuroendocrine tumour. The neuroendocrine compartment was characteristic in its morphological appearance of the commonly observed neuroendocrine tumour. The immunohistochemical profile was consistent with endocrine differentiation.
Despite the fact that carcinoid tumoral components only accounted for 10% of the tumour mass, they were the only elements found in liver and lymph node metastases. Furthermore, the presence of osteoblastic vertebral lesions, characteristic of endocrine tumour bone metastasis,7 suggested an endocrine origin, as clear cell RCC usually produces osteolytic lesions.8 Clinical observations suggest aggressiveness, which can be attributed to the carcinoid tumoral part of the mixed RCC. This also confirms previous observations that renal carcinoid tumours, although considered low-grade endocrine tumours, may have a poor prognosis.4 However, extensive tissue sampling is recommended to understand the presence of such endocrine differentiation. Antiangiogenic therapy is assumed to be effective in cases of typical clear cell RCC.1 In the present case, progression of liver metastases was reported, indicating the failure of the antiangiogenic treatment to deal with the carcinoid tumoral elements. Treatment of this kind for composite malignancy is problematic as the endocrine tumoral elements are probably the most damaging component of the disease. Because most of the literature on carcinoid tumours is based on case reports and small case series, their management and prognosis are unclear. No adjuvant therapy has been clearly established in the case of metastatic carcinoid tumours.4
In conclusion, finding and characterising endocrine tumoral elements in a rare but aggressive composite RCC should trigger consideration of a modified treatment for this kind of renal carcinoma.
-
echohanxiao 离线
- 帖子:367
- 粉蓝豆:1
- 经验:386
- 注册时间:2010-01-09
- 加关注 | 发消息













 好病例,难得见到的好病例,养眼了,谢谢!
好病例,难得见到的好病例,养眼了,谢谢! 
 学习了
学习了 












