| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 系统学病理及英语病理学之一
1a Chronic Pancreatitis
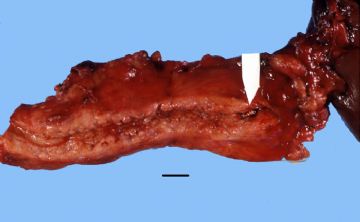
Chronic pancreatitis is characterized by patchy fibrous replacement of whole lobules or parts of lobules, focal fat necrosis in different stages, and chronic inflammation. Grossly, depending on the etiology and degree of injury, the gland may be slightly firm but have a normal outline, lobular pattern, and color. Severe cases may be smaller than normal, bosselated, rock-hard, and display foci of fat necrosis, calcification, or fully developed calculi.
Gross: This chronically inflamed pancreas is small and scarred. The dilated pancreatic duct contains a stone (arrow). Chronic Pancreatitis with stone
onmouseover="showMenu(this.id, 0, 1)"> X-ray: This is an example of chronic pancreatitis with marked calcification of the pancreatic parenchyma. This calcification could be demonstrated by an x-ray of the abdomen.
onmouseover="showMenu(this.id, 0, 1)"> Gross: These are cross sections taken through the head of the pancreas in chronic pancreatitis. The sections of pancreas which you have in your class sets were taken in a similar fashion. Notice that the dense white fibrous scarring has almost totally obliterated the lobular architecture of the pancreas.
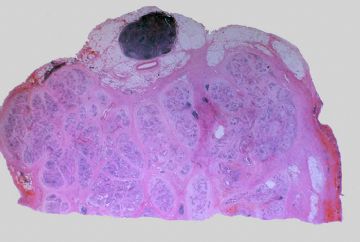
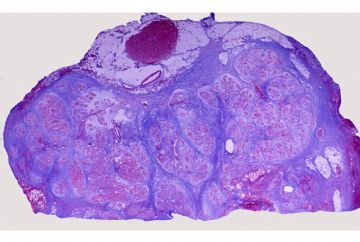
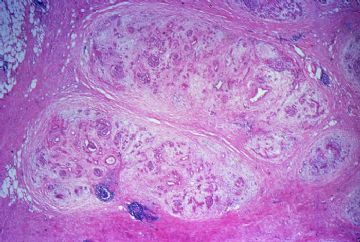
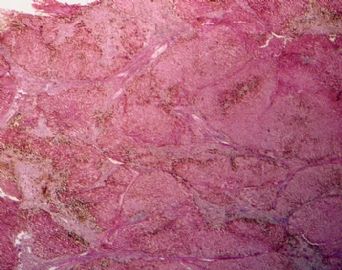
onmouseover="showMenu(this.id, 0, 1)"> This is a low magnification picture of the H&E slide of chronic pancreatitis in your class set. This particular patient had an obstructive type of pancreatitis due to carcinoma of the head of the pancreas. The lobular architecture of the pancreas is accentuated by broad bands of interstitial fibrosis.
onmouseover="showMenu(this.id, 0, 1)"> The fibrous scarring of the pancreas is highlighted with the Trichrome stain. The fibrous septa appear as blue bands surrounding the residual pancreatic lobules, which stain red.
The fibrous scarring of the pancreas is highlighted with the Trichrome stain. The fibrous septa appear as blue bands surrounding the residual pancreatic lobules, which stain red. Shows the dense interstitial fibrosis surrounding two pancreatic lobules. Note there is also an increase in intralobular fibrous tissue and there is chronic inflammation.
Shows the dense interstitial fibrosis surrounding two pancreatic lobules. Note there is also an increase in intralobular fibrous tissue and there is chronic inflammation.
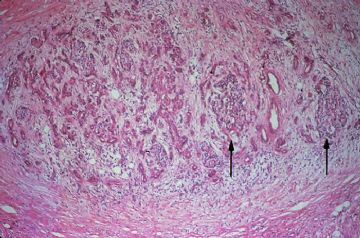
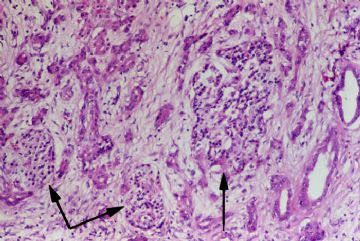
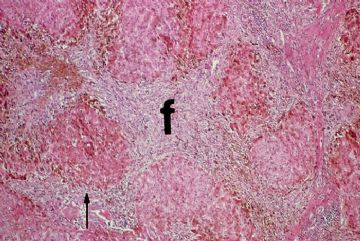
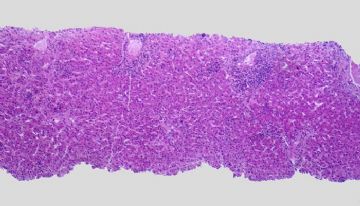
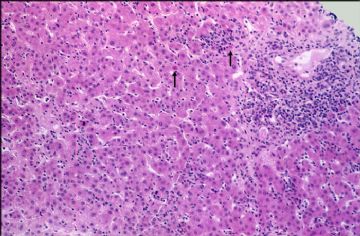
onmouseover="showMenu(this.id, 0, 1)"> The exocrine portion of the gland is most severely affected. There is almost total atrophy and fibrous replacement of pancreatic acini with relative preservation of the pancreatic ducts and islets of Langerhans (arrows). The intralobular pancreatic ductules are irregularly shaped and are embedded in chronically inflamed fibrous tissue. Several preserved islets are marked with arrows
The exocrine portion of the gland is most severely affected. There is almost total atrophy and fibrous replacement of pancreatic acini with relative preservation of the pancreatic ducts and islets of Langerhans (arrows). The intralobular pancreatic ductules are irregularly shaped and are embedded in chronically inflamed fibrous tissue. Several preserved islets are marked with arrows
Higher magnification shows preservation of the islets of Langerhans to better advantage (arrows).

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Hepatocellular Carcinoma
Slide 1
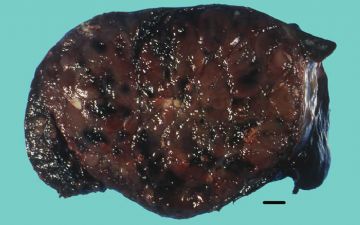
Gross: Hepatocellular carcinoma has a variable macroscopic appearance. This particular hepatocellular carcinoma grew as a predominantly solitary mass occupying most of the right lobe of the liver of a 69 year old white male. The tumor is predominantly tan-brown but you will notice focal areas of yellow necrosis as well as dark red areas of hemorrhage.
Slide 2
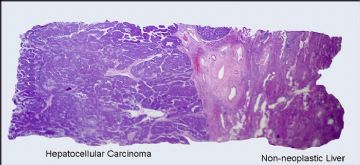
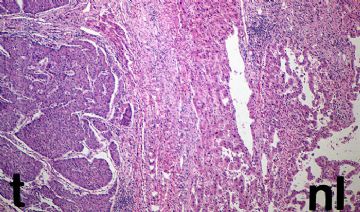
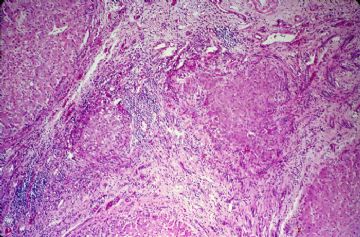
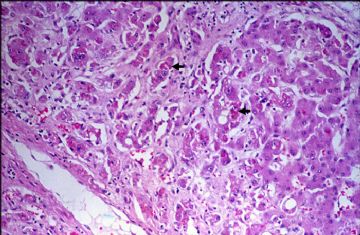
The histologic section in your class set was taken at the junction of the tumor and the non-neoplastic liver.
Slide 3
The junction of tumor and normal liver is seen to better advantage at higher power. The hepatic parenchyma at the edge of the tumor is compressed, giving the false impression that the carcinoma is encapsulated.
Slide 4
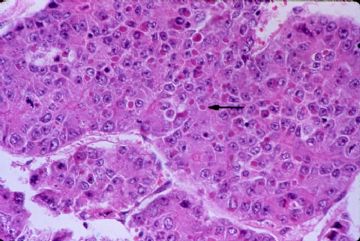
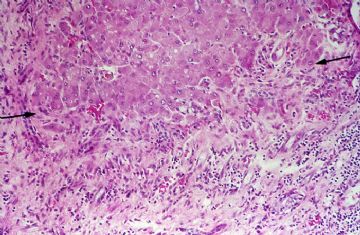
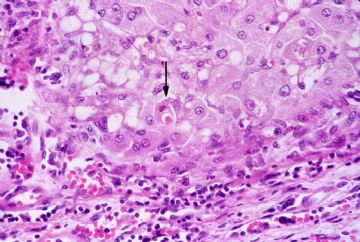
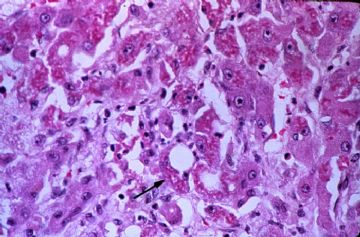
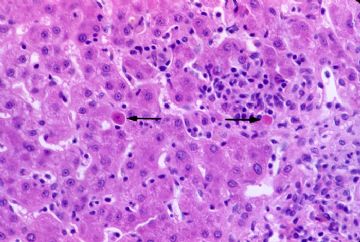
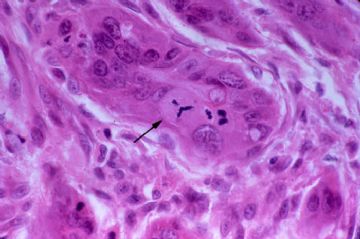
The histologic appearance of hepatocellular carcinoma is also extremely variegated. Many different histologic patterns may be seen, but most are only important to surgical pathologists. This particular carcinoma is growing in nests and thick cords that are separated form one another by thin-walled sinusoids. Cytologically, the tumor cells bear some resemblance to normal hepatocytes, but they are slightly larger, have more irregular nuclei, and prominent nuclei. There are also numerous mitotic figures. You may also notice that many of the tumor cells contain intracytoplasmic violaceous, hyaline globules (arrow) that represent proteins produced by the tumor cells. Occasionally, these hyaline globules represent collection of alpha-fetoprotein or alpha-1-antitrypsin.
Slide 5
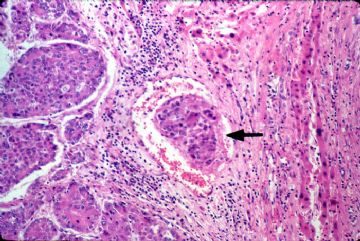
Hepatocellular carcinoma shows a marked tendency to spread by intrahepatic veins, both hepatic and portal. Most of the slides in your class sets will show tumor thrombi within portal vessels (arrow).

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Cavernous Hemangioma of the Liver
The cavernous hemangioma is the most common benign tumor of the liver, occurring at all ages and in both sexes. The majority are asymptomatic, but occasionally they may cause vague abdominal symptoms following episodes of thrombosis. Even more rarely, they may rupture and cause intraperitoneal hemorrhage.
Slide 1
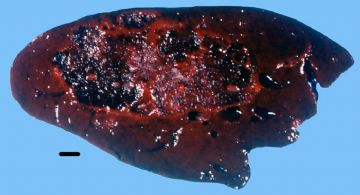
Grossly, most hemangiomas are solitary and under 5 cm in size. This is a particularly large one, measuring about 9 cm. in greatest dimension. It is a soft pulpy, hemorrhagic mass with a spongy consistency.
Slide 2
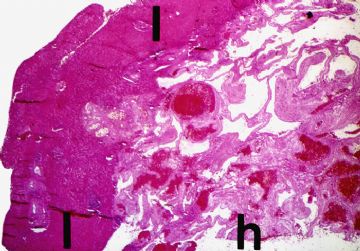
This is a low power view showing the junction of the normal liver (L) at the left with the hemangioma (h) at the right.
Slide 3
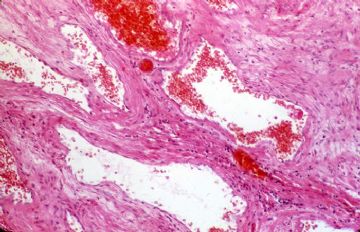
The tumor is composed of endothelial-lined, blood-filled cavernous spaces separated by a fibromyxoid stroma.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Liver Following Prolonged Extrahepatic Obstruction
Extrahepatic obstruction in adults may be due to a number of causes, including inflammatory fibrous strictures of the extrahepatic ducts, impacted calculi, or neoplasms of the extrahepatic ducts or head of the pancreas. The pathologic changes that are seen in the liver are dependent on the duration of the obstruction, but long-standing obstruction will eventually progress to micronodular cirrhosis. The histologic section of liver that you have in your class set was obtained from a patient who had obstruction of the intrapancreatic portion of the common bile duct of several months duration due to a carcinoma in the head of the pancreas。
Slide 1
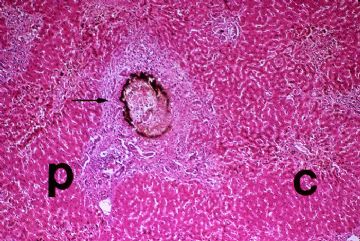
It can be seen at low power that this patient already has some portal scarring of the liver, but does not yet have cirrhosis. There are histopathologic changes in both the portal (P) and central (C) areas of this liver that you should be careful to examine.
Slide 2
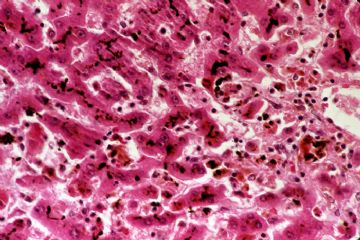
One of the earliest visible changes seen in the liver following extrahepatic obstruction is bile stasis. This is typically most severe in the centrilobular areas. The bile pigment is present as fine granules in the cytoplasm of hepatocytes and as very prominent bile plugs in the biliary canaliculi. Note that the biliary canaliculi between the hepatocytes are stuffed with dark green bile pigment.
Slide 3
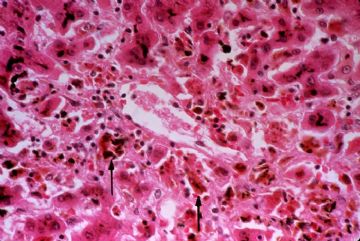
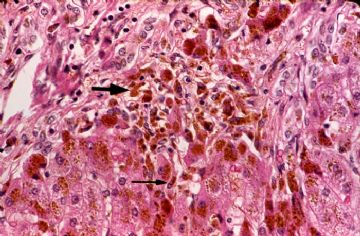
The bile pigment is toxic to hepatocytes which become swollen, showing rarefaction of the cytoplasm referred to as feathery degeneration. Some of these hepatocytes will die and be phagocytized by Kupffer cells which then become latent with bile pigment. This picture is taken from the centrilobular region of the liver and you will see a large central vein in the center of the photograph. Note that many of the pericentral hepatocytes have died and have been phagocytized by Kupffer cells (arrows) which contain bile pigment.
Slide 4
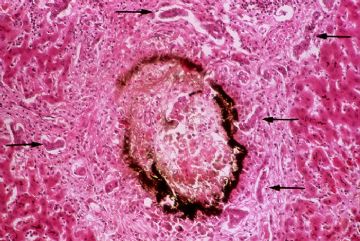
With time, the cholestasis progresses and may be seen in the periportal parenchyma. Occasionally, focal collections of dead, bile stained hepatocytes may be seen. These are called bile infarcts (arrow). They are usually seen in the periportal parenchyma.
Slide 5
Shows a higher magnification a periportal bile infarct. After several weeks of unrelieved obstruction, bile ductular proliferation (arrows) may be seen. With time there is progressive portal fibrosis. Eventually, these fibrous septa link to completely circumscribe islands of hepatic parenchyma and the patient will develop cirrhosis

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Primary Hemochromatosis of the Liver
The basic pathologic feature in hemochromatosis is the deposition of massive amounts of iron in various organs of the body. Because the liver is the major storage site for iron and plays a key role in all conditions of iron overload, it is often severely affected. The deposition of iron in hepatic parenchymal cells leads to tissue damage, fibrosis, and eventually cirrhosis. The actual molecular mechanism by which iron causes hepatic damage is not known, but it is felt that iron alters oxidative phosphorylation. Hemochromatosis may be primary (hereditary) or secondary (increased dietary intake; multiple transfusions; hemolytic conditions). The changes in the liver in primary hemochromatosis depend on the stage of disease. In the early stages there is deposition of iron in the hepatic parenchymal cells but no alteration of the hepatic architecture. The liver is large and may have a rust or dark brown color。
Slide 1
The example of hemochromatosis in your class set is an example of the late stages of the disease. Bands of fibrosis have completely circumscribed regenerating nodules of hepatic parenchyma. This is an example of cirrhosis caused by a metabolic disease.
Slide 2
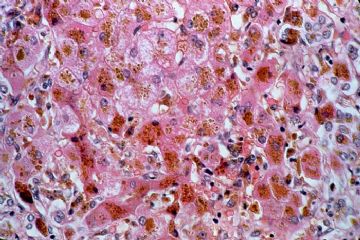
Higher magnification shows these chronically inflamed bands of fibrosis (F) surrounding islands of regenerating hepatic parenchyma (arrow). Note that the regenerative nodules lack central veins. Even at this magnification you may be able to appreciate the dark-brown hemosiderin pigment distributed throughout the liver.
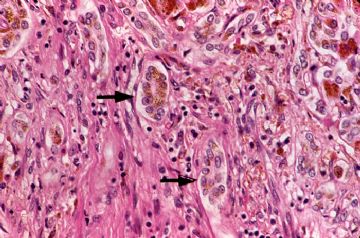
The golden-brown refractile hemosiderin granules are present within hepatocytes (Slide 3), within bile duct epithelium (Slide 4: Arrows), within Kupffer cells (Slide 5: Skinny Arrow) and within portal macrophages (Slide 5: Fat Arrow).
Slide 3
The golden-brown refractile hemosiderin granules are present within hepatocytes.
Slide 4
The golden-brown refractile hemosiderin granules are present within bile duct epithelium (Arrows).
Slide 5
The golden-brown refractile hemosiderin granules are present within Kupffer cells (Skinny Arrow) and within portal macrophages (Fat Arrow).

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Slide 1
Gross: You will recall from your lecture that cirrhosis is a chronic disease of the liver characterized by diffuse destruction and regeneration of hepatocytes, as well as subsequent fibrous scarring that results in disorganization of the lobular architecture. Put more simply, cirrhosis is characterized by fibrosis of the liver and regenerative parenchymal nodules. Cirrhosis may be divided morphologically into two basic types: micronodular cirrhosis and macronodular cirrhosis. The micronodular pattern has uniform regenerative nodules of lobular size or smaller (3 mm in diameter and less) and in the U.S. is usually caused by alcohol. In macronodular cirrhosis, the regenerative nodules are large and irregular in size and shape. The fibrous septa are often broad. Macronodular cirrhosis corresponds loosely to the older terms "post-necrotic" or "multilobular" cirrhosis and in the U.S. is most often seen following chronic active viral hepatitis. This is an example of cirrhosis caused by hepatitis C.
Slide 2
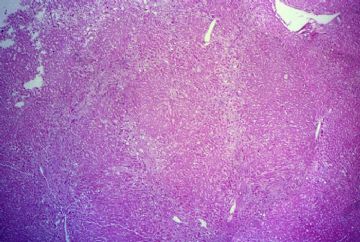
Is a low power view of the actual slide in your class set. The hepatic architecture is disturbed by broad bands of fibrosis that completely circumscribe irregularly sized and shaped nodules of regenerating hepatic parenchyma. These nodules range in size from less than 1 mm in diameter to greater than 5 mm in diameter。
Slide 3
Shows at higher power the broad fibrous septa which completely surround regenerating nodules of hepatic parenchyma. This patient's cirrhosis resulted from chronic active hepatitis C and there is ongoing chronic inflammation and necrosis in this liver.
Slide 4
Is taken at the margin of a regenerative nodule and a fibrous scar (double arrows). Note the irregular contour of the regenerative nodules and the intense necroinflammatory activity (“piecemeal necrosis”) at the interface of the fibrous septa and the hepatic parenchyma
Slide 5
If you look carefully you may be able to find ongoing apoptosis of infected hepatocytes. The arrow indicates an acidophilic body
Slide 6
You may be puzzled to note that many of the hepatocytes within the center of the regenerative nodules are shrunken and more eosinophilic. These centrally located hepatocytes have undergone ischemic necrosis. You will recall from your syllabus that the fibrosis and regenerative nodules of cirrhosis destroy the hepatic architecture and disrupt blood flow through the liver. Often the hepatocytes at the center of the regenerative nodules are only marginally supplied with blood. Should the patient suffer a hypotensive episode, as typically occurs from bleeding esophageal varices, the centers of the regenerative nodules will infarct.
Slide 7
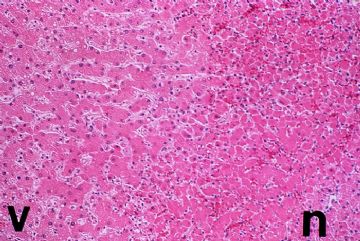
Shows at higher power, the demarcation between the peripherally located, viable (V) hepatocytes and the more centrally located, necrotic (N) hepatocytes.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Slide 1
The hepatic architecture is disturbed by portal and sinusoidal (pericellular) fibrosis. Some of the fibrous bands are just beginning to link-up to circumscribe nodules of hepatic parenchyma. This patient not only has very early cirrhosis but also acute alcoholic hepat
Slide 2
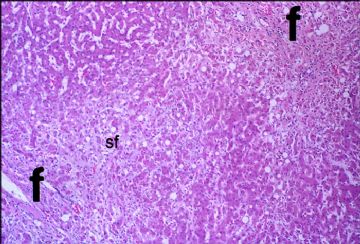
Shows portal fibrosis (f) and sinusoidal fibrosis (sf). The latter may be especially common in the livers of patients with severe alcoholic and non-alcoholic types of steatohepatitis.
Slide 3
Shows prominent pericellular fibrosis (individual and small clusters of hepatocytes completely surrounded by fibrous tissue). This sinusoidal or pericellular fibrosis is usually most severe in centrilobular regions and is a common feature of alcoholic hepatitis. Note that many of the hepatocytes contain Mallory bodies.
Slide 4
Mallory bodies (arrow) appear as violaceous, ropy, hyaline inclusions located in the perinuclear region of the cytoplasm of the hepatocytes. They are composed of degenerated intermediate (cytokeratin) filaments of the cytoskeleton of the liver cells. Mallory bodies are chemotactic for neutrophils, and polymorphonuclear inflammation is characteristic of alcoholic hepatitis. As a matter of fact, some investigators feel that enzymes released by polymorphonuclear leukocytes may be responsible for the pericellular fibrosis seen in alcoholic liver disease. You will remember that the inflammation in acute viral hepatitis, on the other hand, is predominantly mononuclear.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Slide 1
Is a low power view of the needle biopsy. Even at low power magnification you can see that the portal tracts are expanded by an inflammatory infiltrate of lymphocytes
Slide 2
Is a higher magnification of a portion of one classic hepatic lobule. The portal tract shown in the upper right hand corner is expanded by a chronic inflammatory infiltrate of lymphocytes. Clusters of lymphocytes and hyperplastic Kupffer cells are scattered throughout the hepatic lobule as well. There is also focal apoptosis of individual hepatocytes (arrows). The constellation of findings of chronic inflammation, cell death, and regeneration has been termed by pathologists: "lobular disarray".
Slide 3
The body rids itself of the hepatitis virus by killing virus-bearing hepatocytes. Cytokines released by immune cells induce infected hepatocytes to undergo programmed cell death, or "apoptosis". The cytoplasm of apoptotic hepatocytes becomes densely eosinophilic, and the nuclei become shrunken, pyknotic, and fragmented. Also known as acidophilic bodies, apoptotic bodies, or Councilman bodies (arrows), these intensely eosinophilic dead hepatocytes are engulfed by Kupffer cells and digested. In most cases, viral hepatitis is self-limited and the liver is regenerated without complication.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Slide 1
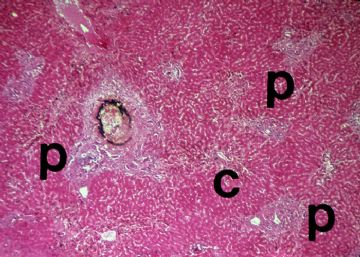
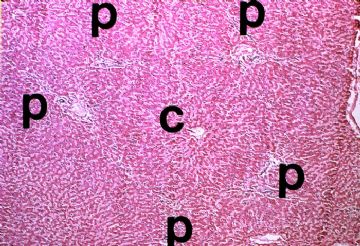
The hepatic architecture may be anatomically defined (the classic hepatic lobule) or functionally defined (Rappaport's acinus). The classic hepatic lobule consists of a central vein (C) with its surrounding hepatocytes and 4-6 portal tracts (P). The hepatic plates are typically one cell thick and radiate away from the central vein like spokes of a wheel.
Slide 2
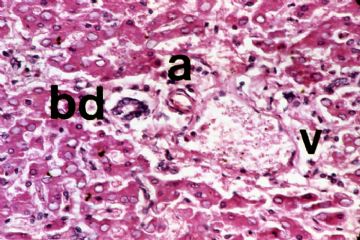
Each portal tract should contain a bile duct (BD) lined by a single layer of cuboidal or columnar cells, a branch of the hepatic artery (A) and a branch of the portal vein (V), all of which are invested by fibrous stroma. Scattered chronic inflammatory cells are normally found within the portal tracts and unless significantly increased they are of no importance.
Slide 3
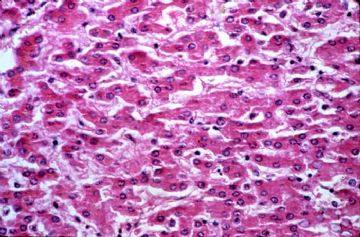
The hepatocytes are typically arranged in single cell plates. They are large polygonal cells with granular, eosinophilic cytoplasm and round, vesicular nuclei that are often nucleolated. The smallest biliary radicles, the canaliculi, are formed by the apposing plasma membranes of two adjacent hepatocytes. The sinusoids are lined by endothelial cells and Kupffer cells. Kupffer cells are derived from the monocyte-macrophage system and are actively phagocytic. They are larger than the endothelial cells and often have a bean-shaped nucleus. If you have a good eye, you should be able to identify them in your slide of normal liver. They become much more prominent when they contain phagocytosed material and you will be able to see them very well in your example of hemochromatosis.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Adenocarcinoma of the Colon
Gross: The patient who harbored the two pedunculated adenomas that you just saw also had a huge fungating adenocarcinoma of the cecum. The histologic section in your class set was taken at the junction of carcinoma and normal mucosa in the plane of the large black bar.
Slide 2
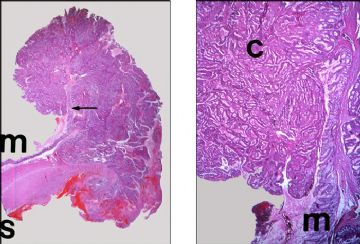
The left panel is a low power view of the slide in your class set showing the normal colonic mucosa (M) and the raised, overhanging margin of the exophytic carcinoma. As is unfortunately too often the case in resected carcinomas, the tumor extends throughout the entire thickness of the bowel wall. The field marked by the arrow shows both normal and carcinomatous epithelium that is shown at higher magnification in the right panel..The normal colonic mucosa (M) is composed of the typical straight tubular glands. Note the granular crowding and the complex glandular pattern of the carcinoma (C).
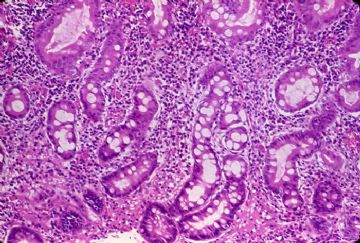
Slide 3
Left Panel: By now you are an expert at recognizing the histologic features of adenocarcinoma. The carcinomatous glands are arranged back-to-back and there is gland-within-gland formation. The walls of the carcinomatous glands are thicker and and more cellular than the normal colonic mucosa on the right.
Right Panel: The carcinoma shows an increased nuclear-to-cytoplasmic ratio in the adenocarcinoma cells. The nuclei show chromatin clumping and prominent nucleoli. There are also numerous mitotic figures. The cells are still differentiated enough to produce mucin, however, which collects within the center of the lumens as granular eosinophilic material. For this reason, this is a moderately differentiated adenocarcinoma.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
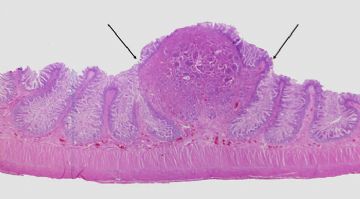
Adenoma of the Colon
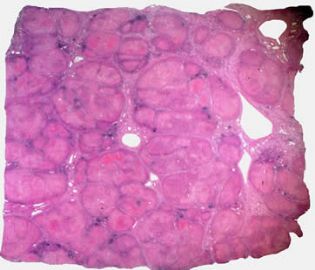
Slide 1
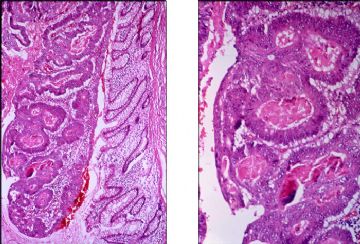
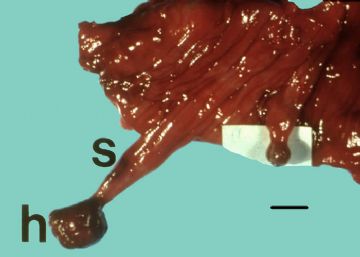
Adenomas are neoplastic polyps. Although by definition benign, carcinoma may arise in adenomas and for this reason they are considered to be premalignant lesions. Adenomas may be sessile or pedunculated, the two in this photograph being examples of the latter. Notice that each of these adenomas has a neoplastic, polypoid head (H) attached to a long stalk (S) of normal colonic mucosa. The sections in your class set were taken through the larger polyp on the left (Slide 2).
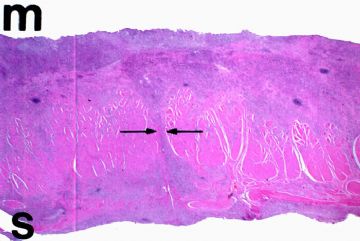
Slide 2
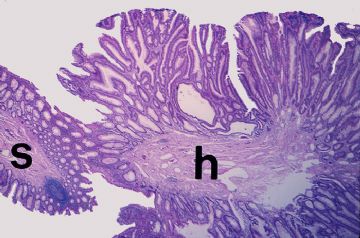
This is a low power view of the glass slide in your class set. You can easily recognize the polypoid head (H) attached to the long stalk (S) of normal colon.
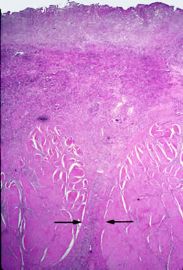
Slide 3
Is a higher magnification of the junction of the stalk and the head of the adenoma. Note the hypercellularity of the adenomatous epithelium. The mucosa of the head of the polyp is considerably thicker than that of the stalk of the adenoma. The mucosa of the head of the adenoma shows elongated tubular structures as well as occasional villus formations, and for this reason this adenoma would be classified as a tubulovillous adenoma. Also notice the complex granular pattern of the adenoma. The adenomatous glands display lateral branching from the middle and upper regions of the crypts unlike normal crypts which increase in number by bifurcation at their bases, and some cystically-dilated glands are present as well.
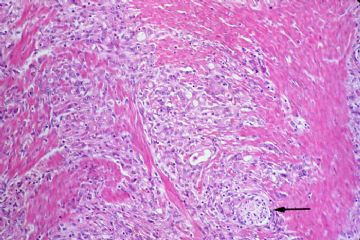
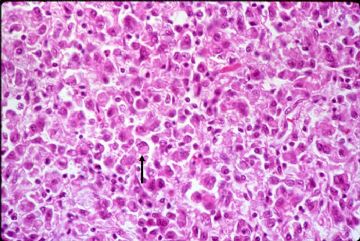
Slide4
Left Panel: Pay particular attention to the cytology of the adenomatous glands. The adenomatous glands show cell crowding with stratification and hyperchromasia of cellular nuclei. Numerous mitotic figures may be seen at all levels of the crypt. In addition, there is impaired differentiation and some glands show diminished numbers of goblet cells.
Right Panel: Compare and contrast the cytologic features of normal and adenomatous glands in this higher power view. The normal glands show a single layer of epithelium with basally oriented nuclei and numerous goblet cells. The adenomatous glands on the other hand show marked cellular hyperplasia with stratification and hyperchromatic nuclei, increased mitotic figures and diminished numbers of goblet cells.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
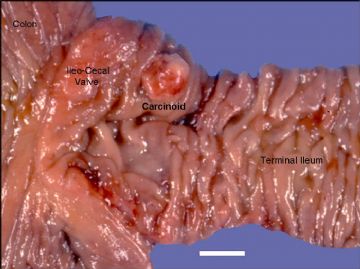
Carcinoid Tumor of the Ileum
Slide 1
Gross: Grossly, most intestinal carcinoids are small, round to plaque-like, submucosal elevations measuring 2 - 3.5 cm. in diameter. On cut section, they are typically yellow or gray-brown
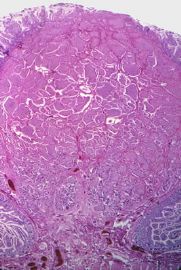
Slide 2
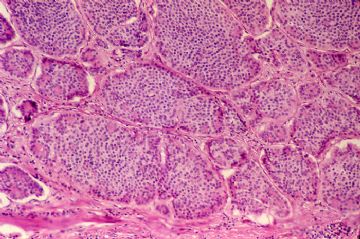
This low power section of the glass slide in your class set shows the typical histologic appearance of a submucosal carcinoid tumor.
Slide 3
Histologically, carcinoids typically grow as multiple solid nests of tumor cells.
Slide 4
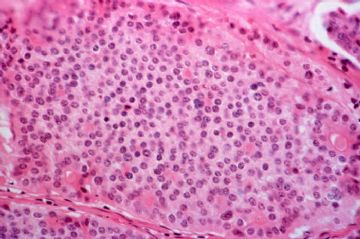
These nests are composed of closely packed, very uniform round cells with small, centrally located nuclei that show little pleomorphism, hyperchromasia, or mitotic activity. The cytoplasm is slightly eosinophilic or amphophilic, but cell borders are often indistinct
Slide 5
At higher power note the lack of cytologic pleomorphism and mitotic activity. It is important to remember that the biologic behavior of carcinoids cannot be assessed histologically. Despite their innocuous cytologic appearance, it is not unusual for GI carcinoids to involve all coats of the bowel wall and to metastasize to distant organs, particularly the liver.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
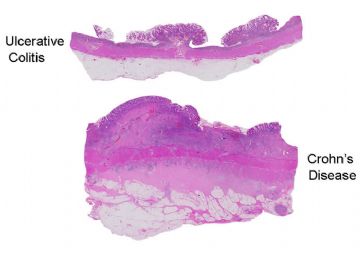
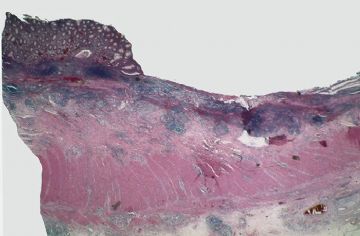
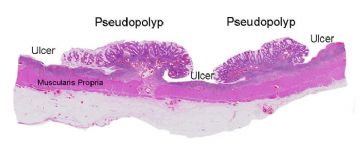
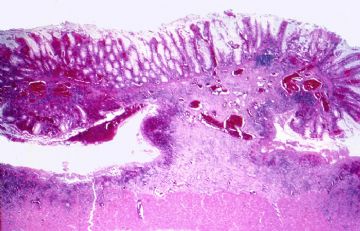
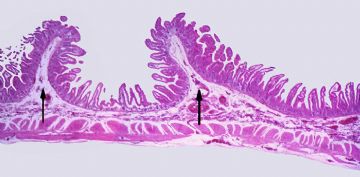
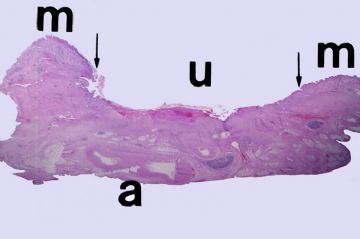
A whole mount preparation showing a histologic section of chronic ulcerative colitis with pseudopolyps (Top Panel) and a classic case of Crohn's disease of the colon (Lower Panel). A number of differences are readily apparent. The most obvious difference is that the colonic wall in Crohn's disease is considerably thicker than that in chronic ulcerative colitis. This is for a number of reasons. First of all, the inflammation in Crohn's disease is transmural; that is, it involves all coats of the colonic wall whereas the inflammation in ulcerative colitis is usually limited to the mucosa and submucosa. The collections of chronic inflammatory cells in all levels of the colonic wall, as well as the inflammatory edema and subsequent fibrosis of the submucosa and serosa in Crohn's disease, account for the increased thickness of the colonic wall. Linear ulcers are present in Crohn's disease as well as in ulcerative colitis, and you can see one in the center of the colonic mucosa in the Crohn's disease below. Whereas the ulcers in ulcerative colitis are usually shallow, the ulcers in Crohn's disease are often fissuring, knife-like ulcers that penetrate deep into the colonic wall. Pseudopolyps are much more common in ulcerative colitis than in Crohn's disease.
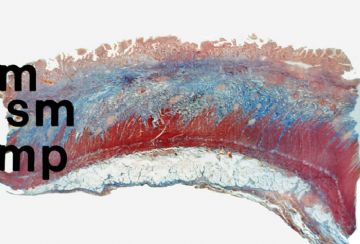
The transmural inflammation in Crohn's disease results in a fibrous reparative response in the submucosa and quite often in the serosa. This Trichrome preparation shows a marked increase in fibrous connective tissue (blue) in the submucosa (SM).
Gross - ileum: The fibrous reparative reaction in Crohn's disease causes marked thickening of the bowel wall and stenosis of the lumen (Rubber hose or lead pipe bowel). This is a classic example of Crohn's disease of the terminal ileum showing marked thickening with a loss of pliability of the wall and narrowing of the lumen.
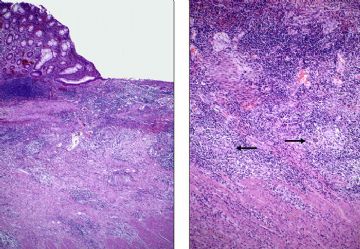
This low power view of Crohn's colitis shows mucosal ulceration and transmural inflammation.
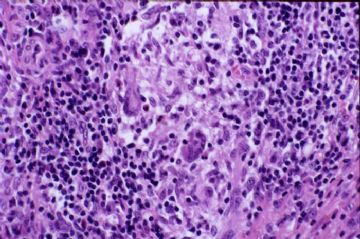
A medium power view shows the mucosal ulcer to better advantage in the left panel. There is prominent submucosal inflammation with scattered non-caseating granulomas. These sarcoid-like granulomas are found in many cases of Crohn's disease (hence the alternate name "granulomatous colitis"). They are not found in ulcerative colitis. These granulomas are shown at higher power in the right panel.
A high power view of a non-caseating Crohn’s granuloma with epithelioid giant cells.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Ulcerative Colitis and Severe Ulcerative Colitis With Pseudopolyps
Gross: This colectomy was performed for idiopathic ulcerative colitis. The mucosa is hyperemic, friable, and granular due to capillary dilatation and congestion in the lamina propria. The entire colon from the cecum to the anus is involved, a presentation which gastroenterologists refer to as universal colitis or pancolitis. About 1/2 of patients with ulcerative colitis will have pancolitis: the remainder will have disease limited to the left colon and rectum.
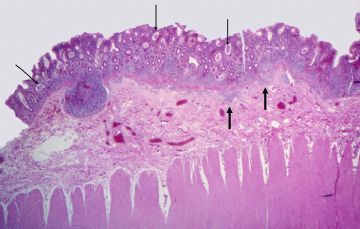
A low power view of the example of mild ulcerative colitis in your class set. The changes which you need to see are limited to the mucosa (M). The large round purple structures present in the submucosa, two of which are marked with arrows, are lymphoid aggregates.
A higher magnification of the mucosa and submucosa. There is marked chronic inflammation that is largely limited to the lamina propria of the mucosa and only focally spills across the muscularis mucosae to involve the submucosa (large arrows). Notice that many of the colonic crypts are dilated (skinny arrows).
These dilated crypts represent "crypt abscesses" which are clusters of polymorphonuclear leukocytes located in the depths of the crypts. The crypt epithelium typically shows depletion of goblet cells and reactive nuclear changes (nuclear enlargement; vesiculation of chromatin; appearance of nucleoli; increased mitoses).
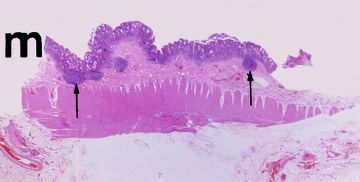
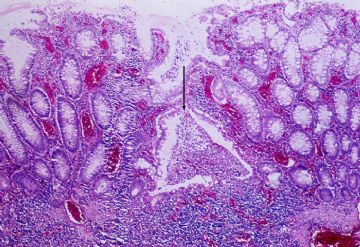
As the crypt abscesses of ulcerative colitis increase in size, they undermine the adjacent mucosa, which sloughs to form numerous, closely placed, shallow ulcers covered by fibrinopurulent exudate (U). Almost total ulceration occurs in severe cases, in which the surface is intensely hemorrhagic. Healing of extensively ulcerated areas is initiated by granulation tissue. Residual inflamed mucosa and exuberant granulation tissue often form nodules elevated above the surrounding mucosa that are called "inflammatory pseudopolyps" (P). A histologic section taken across the pseudopolyps and ulcers in the plane of the black bar would have the appearance shown in the next.
A low power view of the actual slide in your class set which shows two pseudopolyps separated by shallow ulcers. Note that the ulcers do not penetrate into the muscularis propria.
A pseudopolyp at higher magnification. The overlying mucosa of the polyp is hyperplastic. The connective tissue core of the polyp is chronically inflamed. It shows active granulation tissue characterized by the dilated capillary vessels

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
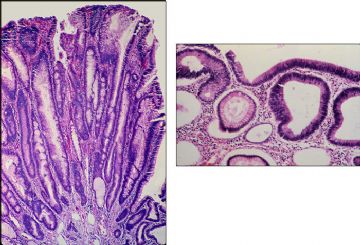
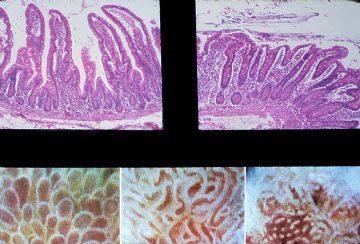
Montage: A histologic section of normal jejunum is seen in the upper left panel. With the dissecting microscope these villi have the appearance of that seen in the lower left panel. A histologic section and a dissecting microscopic view of gluten enteropathy are shown in the upper right and lower right panels respectively.
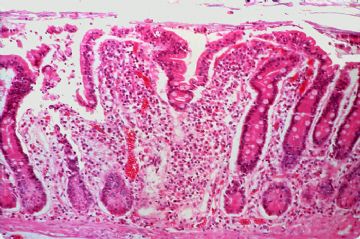
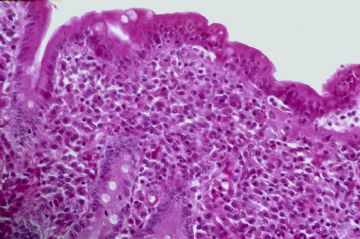
This is a histologic section of the slide in your class set. Gluten enteropathy or celiac disease is believed to be due to a hypersensitivity response of the intestinal mucosa to gliadin, a component of gluten, which is the major protein in wheat, rye, barley and oats. The mechanism of the disease is unclear, but some immunological basis is thought to be likely. Hypersensitivity to gluten results in destruction of the villus epithelial cells. The increased rate of cell loss results in an adaptive mucosal response that is characterized by hyperplasia and increased replication of the crypt epithelium. The crypts thus become elongated. When the adaptive capacity of the crypt cell population has been exhausted through more cell division, more rapid migration, and an increase in crypt cell numbers, a point will be reached where the proliferative compartment is incapable of reproducing the normal villus pattern of the mucosa, and the villus contours become simplified or atrophic. Celiac disease is an example of crypt hyperplastic villus "atrophy." The crypts, however, are markedly elongated such that the total mucosal thickness is not markedly decreased. There is also an increase in crypt cell mitoses.
As mentioned above, the cause of celiac disease is a hypersensitivity response of the intestinal mucosa to gluten. The lamina propria particularly shows a marked increase in the number of plasma cells and lymphocytes and transepithelial migration of lymphocytes across the surface epithelium (arrow) is common. Upon withdrawal of gluten, recovery is gradual and the villus morphology will return to normal in several months.
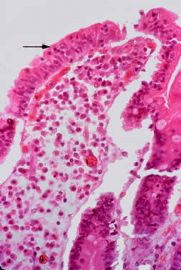
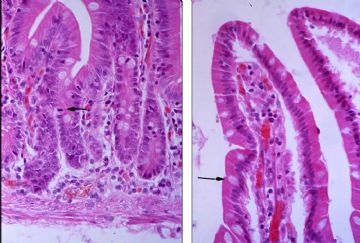
This is another endoscopic biopsy of celiac disease that shows total crypt hyperplastic villous atrophy with complete flattening of the mucosal surface. Note the intense lymphoplasmacytic inflammation in the lamina propria
The surface epithelium of this biopsy contains numerous intraepithelial lymphocytes.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
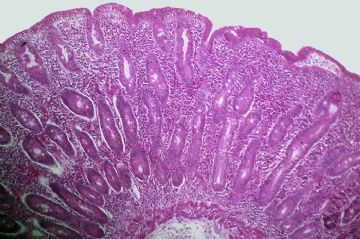
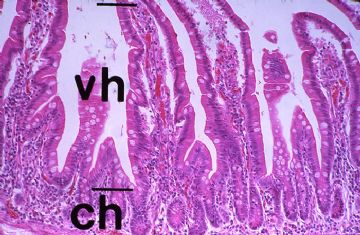
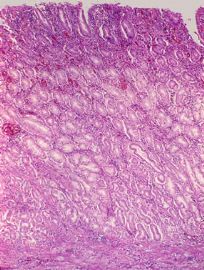
A low power view of the glass slide in your class set. The mucosa of the jejunum is thrown into plical folds (arrows) which are covered with the intestinal villi that measure 0.5 to 1.5 mm in length.
Regularly spaced in the valleys between the villi, and numbering some 2-3 per villus, are the straight, tubular intestinal glands or crypts of Lieberkuhn. Given individual variation, the average villus height (VH) to crypt height (CH) in the jejunum is about 6:1. This ratio should always be assessed when evaluating small bowel biopsies because many malabsorptive diseases are characterized by villus atrophy with subsequent decrease in the villus height to crypt height ratio.
The left panel shows the intestinal crypts at high magnification. The lower half of the crypts contains mostly undifferentiated cells with a high mitotic rate. One mitotic figure is noted by the arrow. As the villus epithelium of the intestine is shed, there is upper displacement and differentiation of cells generated from the undifferentiated basal epithelium. The entire process of cell division, migration, and maturation takes about 2-6 days.The right panel shows the villous epithelium at high magnification. As the undifferentiated cells of the crypt migrate up into the villus, they differentiate into the absorptive cells covered by a microvillus brush border and into mucin-secreting goblet cells (arrow). Note the lacteal in the central core of the villus.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Gross: Linitis plastica carcinoma diffusely infiltrates the entire gastric wall without forming an intraluminal mass. The wall of the stomach is typically thickened to about 2-3 cm. and has a leathery, inelastic consistency.
A low power view of the slide in your class set. Poorly differentiated carcinoma arises from the mucosa and diffusely infiltrates all layers of the gastric wall.
This is a higher magnification showing effacement of the lamina propria of the gastric mucosa by adenocarcinoma.
A higher magnification showing the malignant epithelial cells extending through the muscularis propria.
Higher magnification of the carcinoma shows it to be composed of diffuse sheets of loosely cohesive, slightly pleomorphic epithelial cells with large nuclear-to-cytoplasmic ratios. This is a poorly differentiated adenocarcinoma in that no glands are formed, but you will notice that some of the cells contain a mucin vacuole that displaces the nucleus to the periphery to form the so-called "signet cell" (arrow).

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
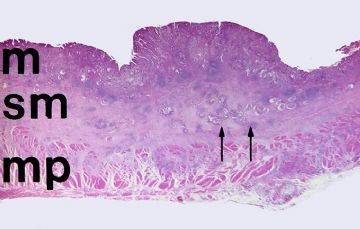
A low power photograph of the slide in your class set. The mucosa "M", submucosa (SM), muscularis propria (MP), and serosa are all readily apparent. At this magnification you can see an adenocarcinoma that extends into the submucosa (double arrows).
The left panel shows a moderately differentiated adenocarcinoma arising from the mucosa. The islands of malignant cells in the submucosa have invaded into lymphatic channels (arrows).
Higher magnification in the right panel shows that the gastric mucosa has been largely replaced by adenocarcinoma. The malignant gland that is marked by the double arrows is seen at higher magnification in Slide 3.
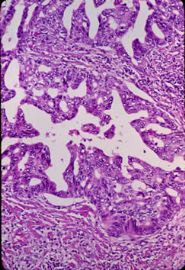
Note the complex pattern of this malignant gland. Whereas a benign gland is lined by a single layer of cells, the malignant gland is hypercellular. This results in the stratification of malignant cells with the formation of an irregular, thickened gland wall. Small, accessory glandular lumina form in the wall of the major gland to form the so-called "gland-within-gland" pattern. Also note the irregular size and shape ("pleomorphism") of the nuclei of the malignant cells and the increased mitoses.
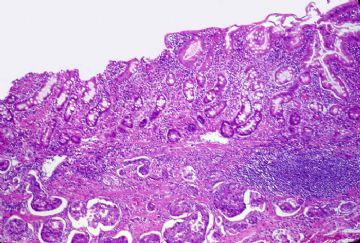
The gastric mucosa adjacent to the carcinoma shows chronic inflammation, glandular atrophy and distortion, and intestinal metaplasia. These findings are typical for chronic atrophic gastritis. As you know, atrophic forms of gastritis with intestinal metaplasia show an increased incidence of gastric cancer.
Shows the intestinal metaplasia of the gastric mucosa at higher power. Note that the foveolar epithelium of the gastric mucosa has been replaced by absorptive cells and mucin-secreting goblet cells typical of the intestinal mucosa. There is also intense chronic inflammation of the lamina propria

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Gross: Chronic peptic ulcers are typically small (less than 4 cm in diameter), round, sharply punched-out lesions with perpendicular walls and a clean base. Fibrous contracture of the base of the ulcer may cause puckering of the surrounding mucosal folds such that they radiate away from the ulcer in spoke-like fashion. A perpendicular histologic section taken through the plane of the yellow bar would appear like that show in the next.
A low power view of the gastric ulcer in your class set. The ulcer (U) lies between the arrows. The intact, but chronically inflamed, gastric mucosa (M) is on both sides. Note that the base of the ulcer extends all the way to the serosa of the stomach. Large arteries (A) are present at the base of the ulcer. Erosion into one of these large arteries could result in massive hematemesis.
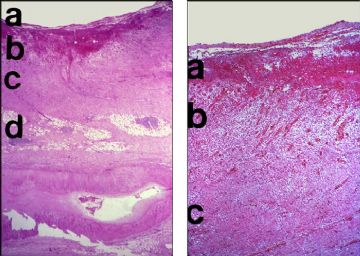
The left panel is a low power view of the full thickness of the gastric wall in the region of the ulcer. This ulcer shows ongoing necrosis, inflammation, and fibrous repair that can be divided into 3 layers. "A" represents the superficial layer of necrotic debris and acute inflammation. Just below this superficial layer is a zone of active granulation tissue (B), which in the deeper layers matures into a fibrous scar (C). The fibrotic subserosal adipose tissue is noted by the letter "D". Again, notice the large artery at the base of the ulcer.
The right panel shows the layers of the ulcer at higher magnification. "A" represents the superficial zone of necrosis and active inflammation, "B" the zone of active granulation tissue, and "C" the deep fibrous scar.
The mucosa adjacent to the ulcer shows chronic gastritis. Note the discrete band of chronic inflammation in the most superficial portion of the mucosa.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Gross: This is an example of an ulcerated squamous cell carcinoma of the esophagus. It differs from a benign peptic ulcer of the esophagus because it is much larger and it has irregular borders, rather than being sharply punched-out. Note the perforation in the center.
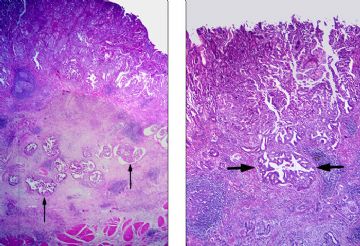
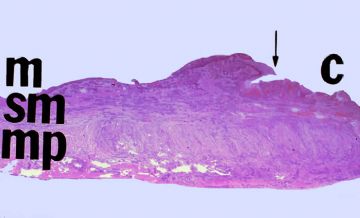
It is a low power view of the histologic section in your class set. (M = mucosa; Sm = submucosa; Mp = muscularis propria). The intact mucosa is to the left of the arrow; the ulcerated carcinoma (C) is to the right.
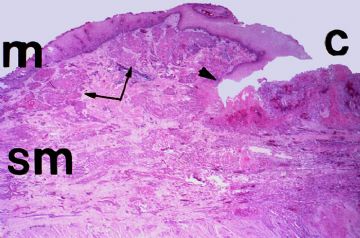
It is taken at the juncture (arrow head) of the normal mucosa (M) and the ulcerated carcinoma (C), and it shows another common feature of esophageal cancer. The gross margins of the cancer are often misleading because the tumor frequently spreads longitudinally within submucosal lymphatics (double arrows).
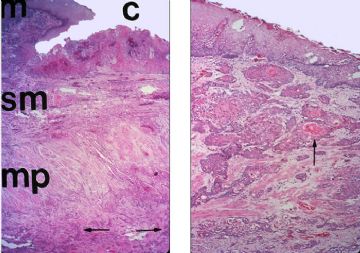
This left panel shows a histologic section taken through the full thickness of the esophageal wall. Carcinomas of the esophagus are typically deeply infiltrating lesions and this one has extended through the muscularis propria (arrows).
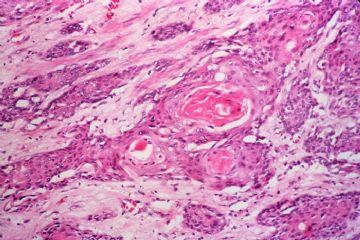
The right panel shows nests of malignant squamous cells within the submucosa. This is a moderately differentiated squamous cell carcinoma which shows keratin production. The malignant cells show a common feature of malignancy, namely altered polarity. The differentiating squamous cells within the submucosal nests cannot slough keratin to the luminal surface. Instead, the keratin accumulates in the center of the nests as spherical keratin "pearls" (arrow).
Shows the moderately differentiated squamous cell carcinoma with keratin pearls at higher power.
Mitotic figures are usually common in malignant tumors and often they are abnormal. This is a tripolar mitosis. If you look carefully, you can see 3 mitotic spindles.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭