| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B2187盆腔肿块
-
本帖最后由 于 2010-02-11 12:45:00 编辑
Agree with wfbjwt that it is like a mesothelail incusion cyst or benign muticystic mesothelioma. I like the term MULTILOCULAR PERITONEAL INCLUSON CYST (from Dr. Schully's paper in 1989- see floor 9) and do not like the term benign mesothelioma.
Based on his 25 cases of study he concluded that The clinical and pathologic data in this series suggest that the MPIC is a nonneoplastic reactive mesothelial proliferation
I do not notice there is a better paper in this area than his 1989 y paper.It is more than 20 years since his paper was published,
For above case
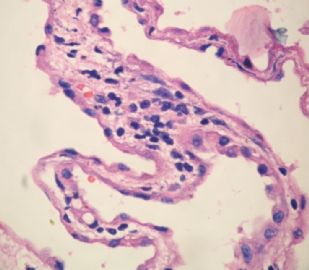
Order calretinin and CK to confirm the nature of the lining cells (mesothelial cells: both positive)
World J Surg. 2006 Apr;30(4):560-6.
Benign peritoneal cystic mesothelioma.
Søreide JA, Søreide K, Körner H, Søiland H, Greve OJ, Gudlaugsson E.
Department of Surgery, Stavanger University Hospital, Stavanger, N-4068, Norway. jon.soreide@kir.uib.no
BACKGROUND: Benign peritoneal cystic mesothelioma (BPCM) is a rare tumor of unknown origin, most frequently encountered in women of reproductive age. Etiology is unknown; definitions and terminology are confusing, and preoperative diagnosis is difficult. Several differential diagnoses must be considered. METHODS: Based on our own clinical experience and a review of the relevant literature, we address clinical challenges and controversies of importance. RESULTS: Current literature on BPCM is mostly based on small case reports. Complete surgical resection is recommended if possible. Nevertheless, recurrent disease is not uncommon. Clinical positive effects of various adjuvant medical treatments remain to be shown. CONCLUSIONS: Lack of consistent definitions, various treatment approaches, and mostly short follow-up times make it difficult to draw any firm conclusions from published reports. The natural history of this rare disease is less than well clarified. When possible, in an individual patient, surgical resection with curative intent seems to be the treatment of choice.
Pol J Pathol. 2005;56(2):81-7.
Mesothelial inclusion cysts (so-called benign cystic mesothelioma)--a clinicopathological analysis of six cases.
Urbańczyk K, Skotniczny K, Kuciński J, Friediger J.
Department of Clinical and Experimental Pathomorphology, Collegium Medicum, Jagiellonian University, Kraków.
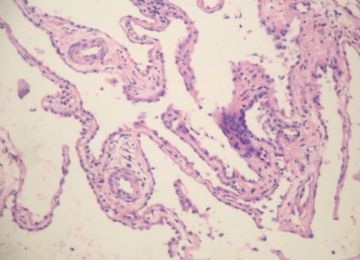
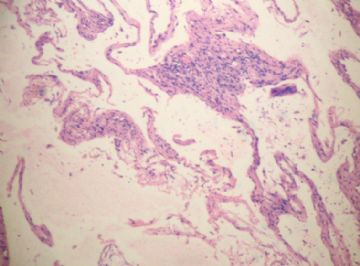
The report presents six cases of mesothelial inclusion cysts (MIC), detected in five females (22-53 years of age) and one male (47 years old). The lesions were unifocal (four cases) and multifocal (two cases), and were located on the surface of the peritoneum in the cul de sac, on the intestines, urinary bladder, uterine adnexa, also involved round ligament within the pelvis and in the inguinal canal (one patient). Additionally, in one female, small cysts, free-floating in the peritoneal cavity were present. In three patients, clinical signs resulted directly from the presence of MIC. One female had been 7 years previously operated on due to endometrioid ovarian cysts. Apart from MIC, three patients presented with concomitant diseases: appendicitis (two cases), peritoneal pseudomyxoma or primary ovarian carcinoma. Gross appearance: the lesions were polycystic, the surgical materials ranging from three fragments measuring 0.5 cm each to seven fragments, with the maximum size of 14x6 cm. The cysts were from microscopic size to 2 cm in diameter, the majority were thin-walled, semitranslucent, filled with clear or yellowish fluid or gelatinous contents. In one case, the cyst walls were thicker and showed intense inflammatory lesions and fibrinous exudate. Microscopically, the majority of cysts were lined with a single layer of flattened or cuboid mesothelial cells (CK+, calretinin+). In two patients, the mesothelium demonstrated diffuse squamous cell metaplasia; in one individual, the cells focally formed small papillae and were vacuolated. No mucus was observed either in the cytoplasm or outside the cells. Immunohistochemical reactions to CEA, ER, PR and MIB-1 were negative. Intramural proliferations and intracystic detached clumps of cells showed both mesothelial cells (without any mitotic activity and signs of atypia) and macrophages (CD68+). To date, the follow-up has been 7 years and 3 years in two individuals, and from 1 to 7 months in the remaining three patients--all of them are free from recurrent disease. One female failed to report for follow-up examinations. The report also presents the review of literature
Gynecol Oncol. 2004 Jan;92(1):334-6.
Multicystic benign mesothelioma of the peritoneum presenting as postmenopausal bleeding and a solitary pelvic cyst--a case report.
Academic Department of Obstetrics and Gynaecology, Birmingham Women's Hospital, Birmingham B15 2TG, UK. r.varma@bham.ac.uk
BACKGROUND: All non-invasive diagnostic algorithms suffer from diagnostic uncertainty in discriminating benign from malignant adnexal masses. CASE: We present a case where the identification of a large solitary multiloculated pelvic cyst in a woman with postmenopausal bleeding was shown to be multifocal multicystic benign mesothelioma (MBM) of the peritoneum at laparotomy. CONCLUSION: We wish to alert gynaecologists of this rare association and the unique appearance of mesothelioma lesions, which many would not instantly recognise. There is a lack of consensus on the treatment and follow-up of MBM. Most authorities consider curative treatment of MBM is achievable through complete disease cytoreduction (peritonectomy) as carried out in the case.
Hum Pathol. 2003 Apr;34(4):369-74.
Benign cystic mesothelioma of the peritoneum: a clinicopathologic study of 17 cases and immunohistochemical analysis of estrogen and progesterone receptor status.
Sawh RN, Malpica A, Deavers MT, Liu J, Silva EG.
Division of Pathology and Laboratory Medicine, The University of Texas M.D. Anderson Cancer Center, Houston, TX 77030, USA.
Benign cystic mesothelioma (BCM) is an uncommon lesion of the peritoneum occurring predominantly in women of reproductive age. Although most patients are managed by surgical resection, a reported high incidence of cyst recurrence has led to the use of hormonal therapy in isolated cases in an attempt to control cyst size and relieve local symptoms. To date, the estrogen receptor (ER) and progesterone receptor (PR) status of BCM has not been evaluated. Here we present our experience with 17 cases (13 women, 4 men) of BCM seen over a 19-year period, including an immunohistochemical analysis of ER and PR status in 14 cases. All lesions showed typical morphological features of BCM, and calretinin immunostaining was positive in 14 of 14 cases. Five patients experienced either 1 or 2 tumor recurrences, and no patients died of disease. One case was diffusely positive for ER only, 1 case was focally positive for PR only, and 1 case was focally positive for both ER and PR. Although immunohistochemical detection of female sex hormone receptors in BCM is uncommon, the focal presence of ER and/or PR in some lesions does provide weak biologic support for the use of hormonal manipulation as a therapeutic option. Hum Pathol 34:369-374.
-
This is a good paper from Dr. Scully.
Cancer. 1989 Sep 15;64(6):1336-46.
Multilocular peritoneal inclusion cysts (so-called cystic mesotheliomas).
Department of Pathology, Harvard Medical School, Boston 02114.
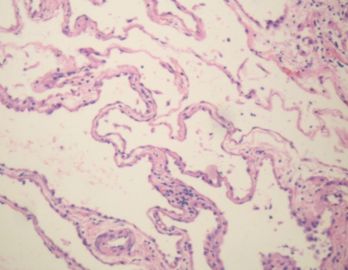
Twenty-five cases of multilocular peritoneal inclusion cysts (MPIC) were investigated. All but four cases were associated with a history of a previous abdominal or pelvic operation, or evidence of endometriosis or pelvic inflammatory disease, or combinations of these findings. All of the lesions were attached to pelvic organs, 44% also occupied the upper abdominal cavity, and 16% involved the retroperitoneum. In three cases free-floating cysts were present as well. The median diameter of the lesions was 13 cm. The cyst locules were lined by one to several layers of flat to cuboidal mesothelial cells that occasionally formed papillae, had a hobnail shape, or had undergone squamous metaplasia. The stroma was characterized by chronic inflammation and often acute inflammation. In most of the cases there was mural proliferation of the mesothelial cells, occasionally simulating a malignant mesothelioma. Twelve lesions were complicated by postoperative local recurrence; in four of these cases the recurrences were multiple; neither the size of the lesion nor the presence of mural mesothelial proliferation influenced the outcome. The clinical and pathologic data in this series suggest that the MPIC is a nonneoplastic reactive mesothelial proliferation.