| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
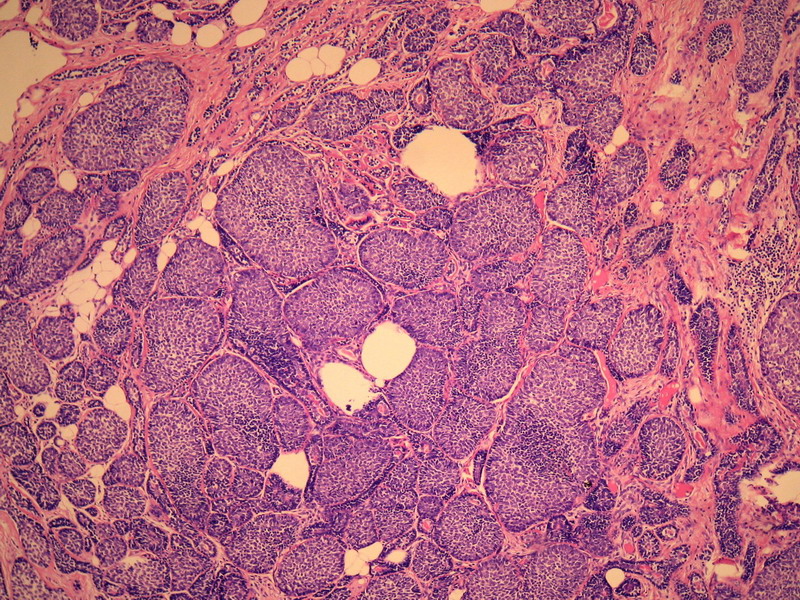
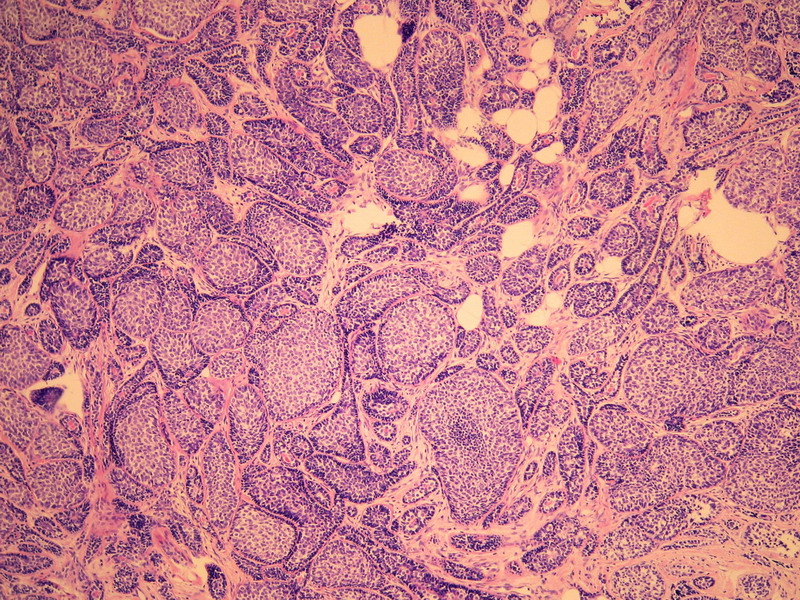
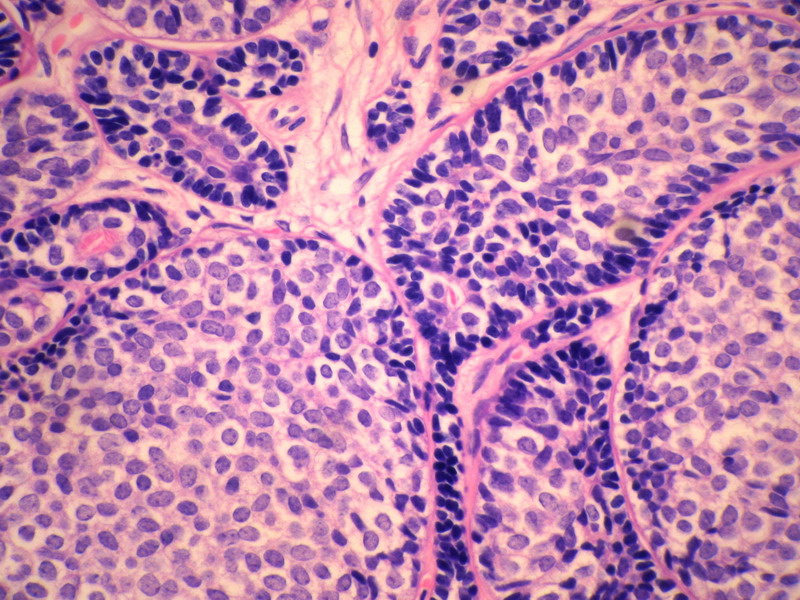
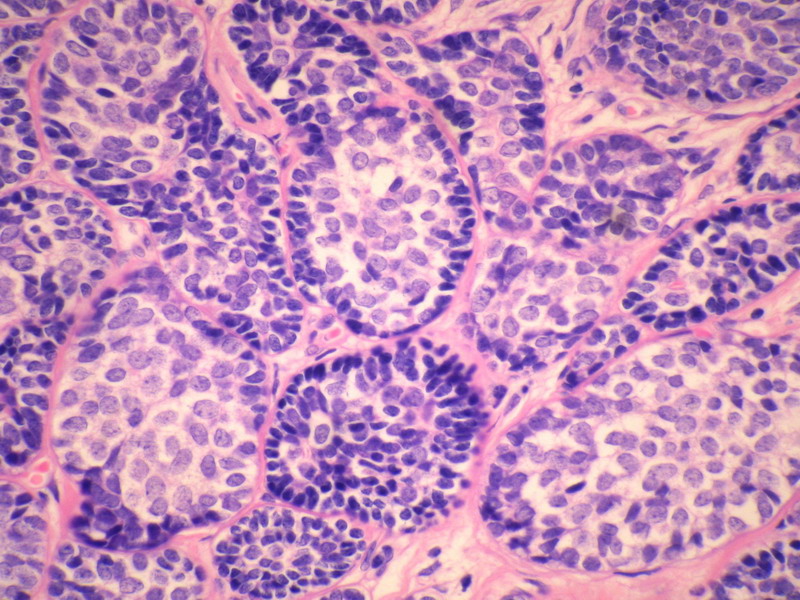
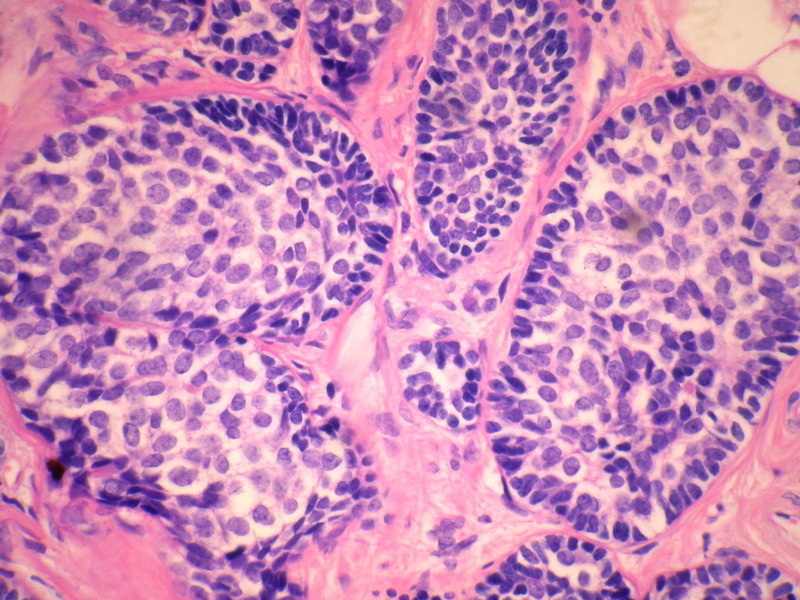
- B228652岁女性,乳腺癌,求类型。已发免疫组化。
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
名称:图1
描述:图1
名称:图2
描述:图2
名称:图3
描述:图3
名称:图4
描述:图4
名称:图5
描述:图5
名称:图6
描述:图6
名称:图7
描述:图7
名称:图8
描述:图8
名称:图9
描述:图9
名称:图10
描述:图10
名称:图11
描述:图11
名称:图12
描述:图12
名称:图13
描述:图13
名称:图14
描述:图14
-
本帖最后由 于 2010-09-09 16:26:00 编辑

- 病理,让疾病明明白白。
相关帖子
- • 边界清楚的乳腺包块
- • 右乳肿块,新加免疫组化结果
- • 乳癌类型?
- • 乳腺肿块,请会诊
- • 左侧乳腺外上象限肿物,髓样癌?
- • 乳腺肿块
- • 女,29岁,发现右乳肿块,停止哺乳后手术切除肿块
- • 请求老师会诊,34岁女,乳腺肿物。
- • 乳腺癌类型?
- • 乳腺微创手术活检,诊断?
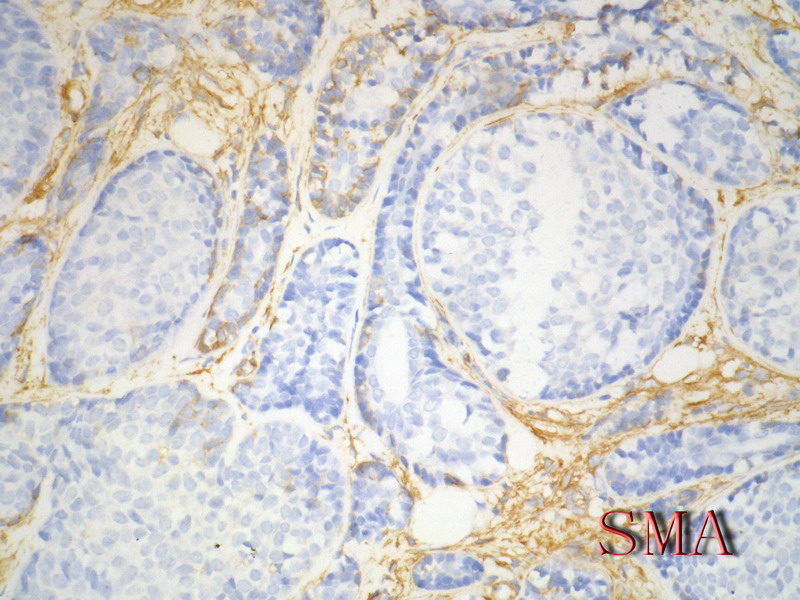
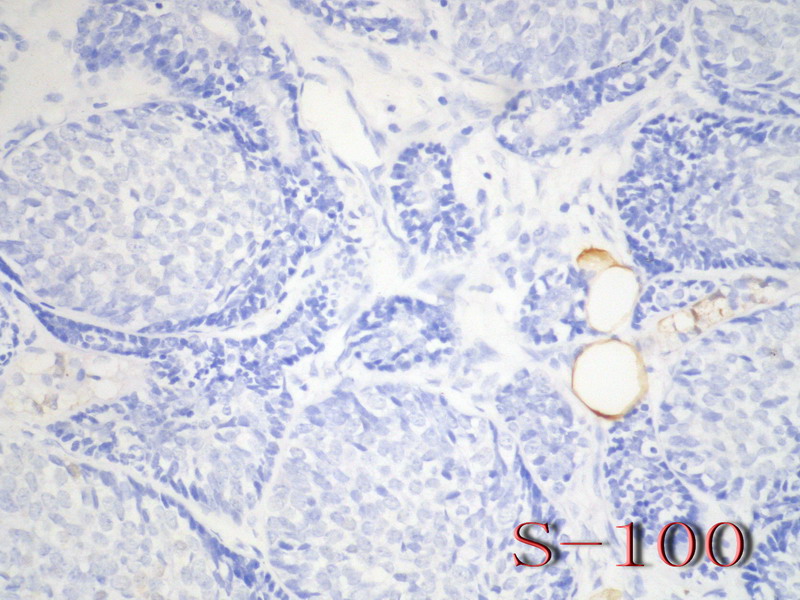
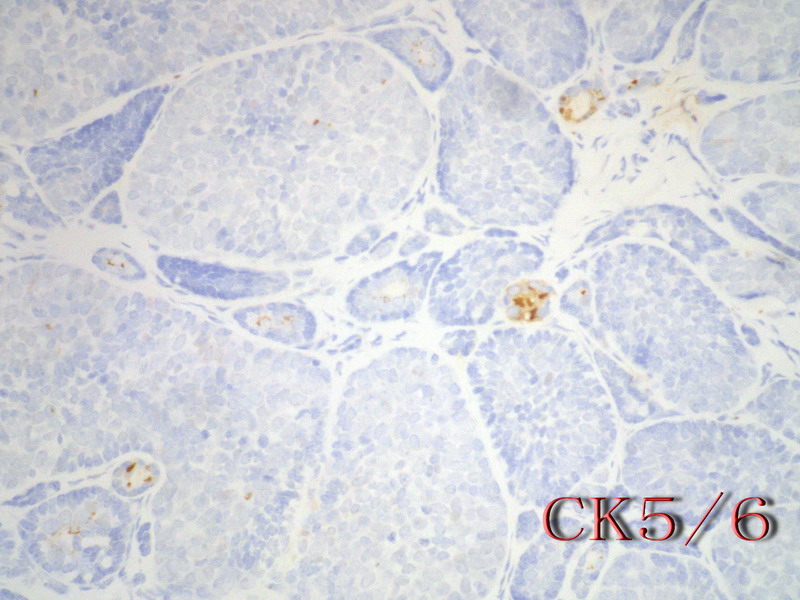
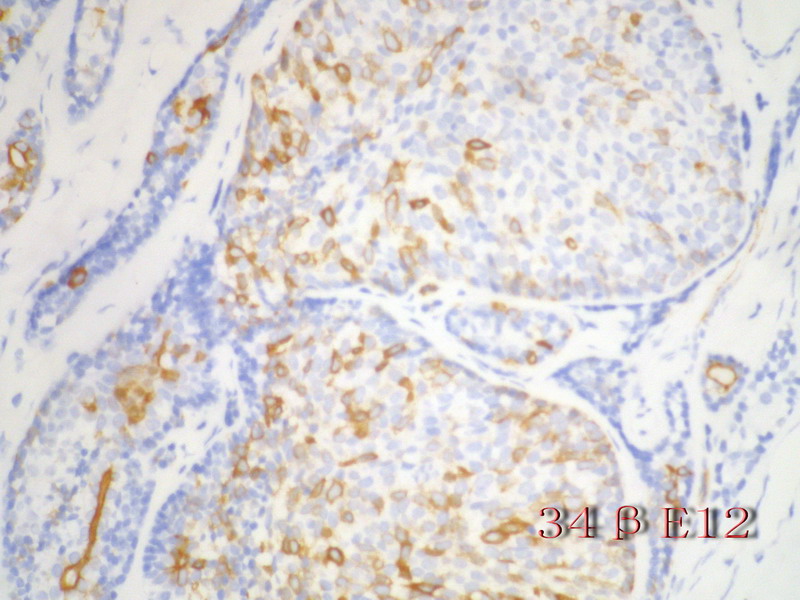
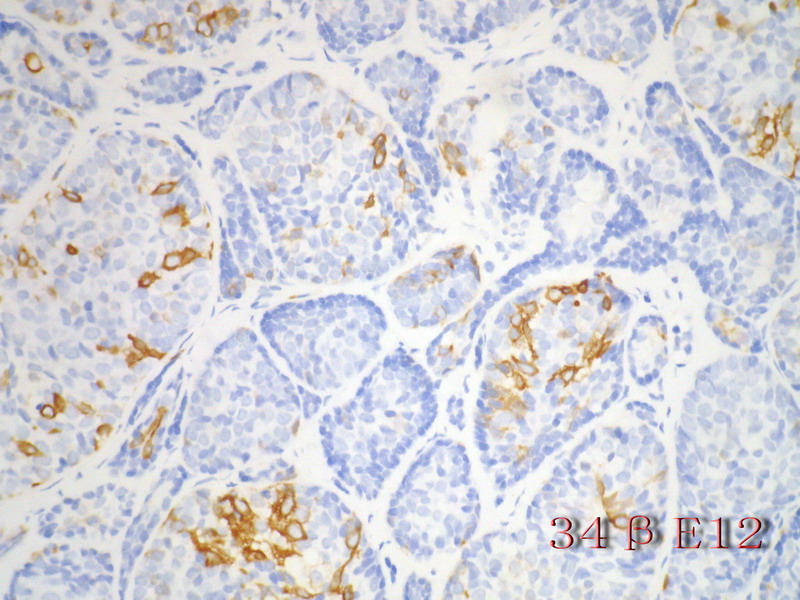
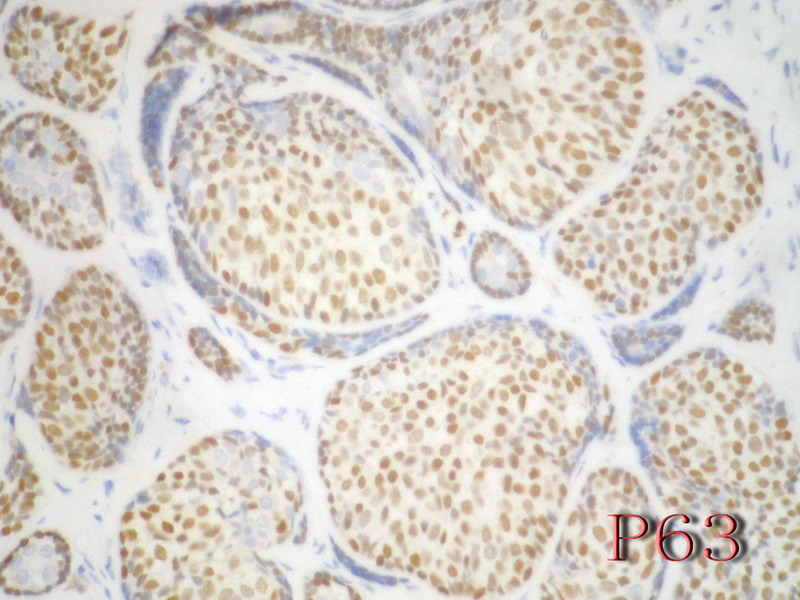
乳腺腺样囊性(ACC)的形态与唾液腺ACC的形态是相似的。唾腺ACC组织学类型:小管型,筛孔型,实体性,混合型。IHC标记:一般标记CK7+ CK14+ CK17+ CK19+; S-100+ MUC1+ RB+ CD117+:
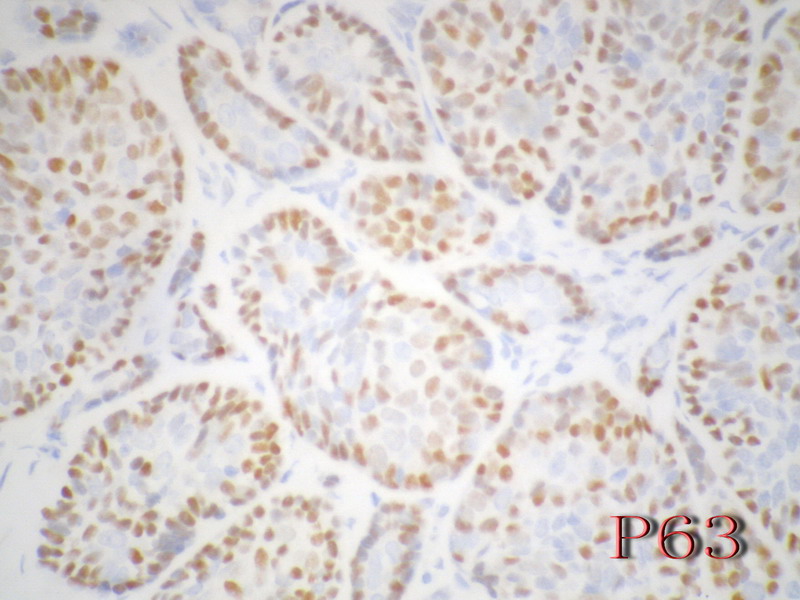
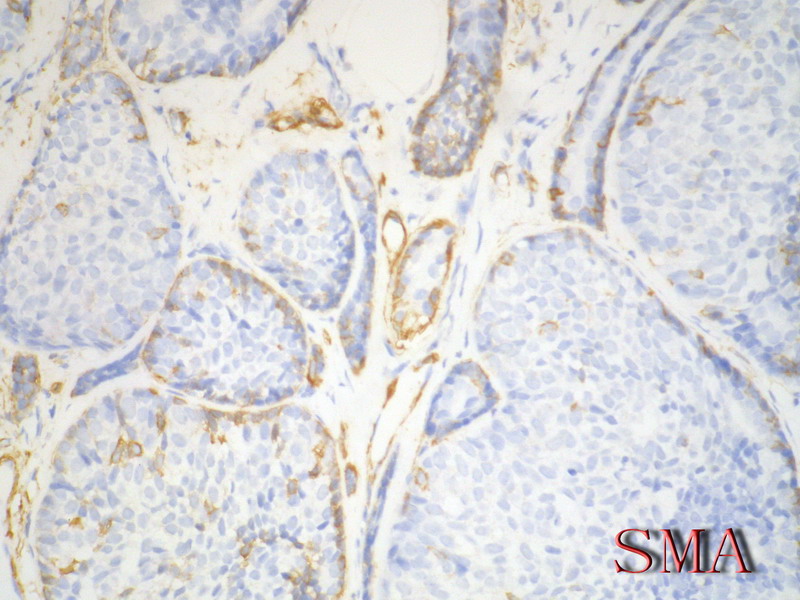
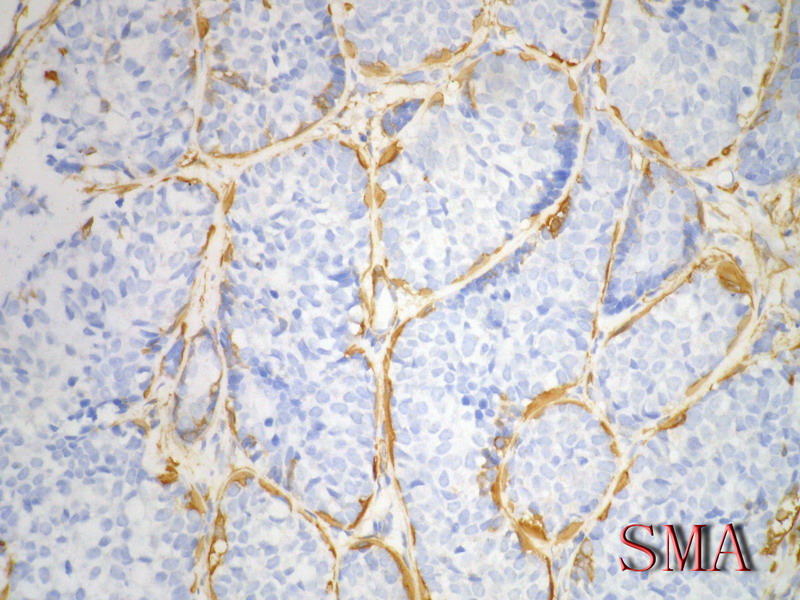
导管上皮细胞:CEA+EMA+;肌上皮分化细胞:CK+ Vimentin+ MSA+ p63+, SMA+ SMMHC+ Calponin+ GFAP 局限+,等。 ER/PR一般为阴性。
注意:乳腺ACC的形态变异比唾腺ACC更多,而且基底细胞样表型时p63-34BE12+。Ro 等提出乳腺ACC可根据肿瘤内实体成分的百分比分为3级:1级 无实体性成分;2级实体性成分小于30%; 3级实体成分大30%。
本例诊断依据:肿瘤浸润性生长,浸润脂肪组织。主要结构为实体细胞团,但可见小管样结构。实体巢周边细胞栅栏样排列,似汗腺圆柱瘤;二种细胞构成(导管上皮和肌上皮),细胞小,比较均一,无核分裂象,无坏死。鉴别1)浸润性小叶癌无二种类型的细胞,肌上皮应该消失,浸润时呈靶形结构和单行排列。2)浸润性导管癌累及小叶时(小叶癌化)肿瘤细胞异型性大,且应有导管癌成分。
以上个人观点仅供参考。

- xljin8
-
本帖最后由 于 2009-11-13 20:42:00 编辑
This is an very interesting case. Thank Dr. XLJin8 's excellent analysis.
My differential dx for this case.
1. lobular lesion, chance is low
2. ACC
3. basoloid carcinoma of breast (BCB)
4. IDC with basal-like phenotype.
Differential dx shoud include all possibilities. Then we will rule out or rule in one by one.
In fact most ACC and BCB are in the category of basal-like carcinoma.
Stains
E-cad
ER, PR, Her2: Most lobular lesions ER/PR+
ACC and BCB: triple negative in most cases
Ckit, P63, SMA positive in ACC, but negative in BCB, high molecular weight CK should be pos in both (see the following abstract, I am not sure).
some basal-like markers ck14, ck5/5, ck17 or EGFR can be positive in both ACC and BCB.
-
本帖最后由 于 2010-09-09 19:00:00 编辑
Ann Diagn Pathol. 2008 Feb;12(1):4-11. Epub 2007 Oct 3.
Basaloid carcinoma of the breast: a review of 9 cases, with delineation of a possible clinicopathologic entity.
Lamovec J, Falconieri G, Salviato T, Pizzolitto S.
Department of Pathology, Institute of Oncology, SI-1000 Ljubljana, Slovenia.
Basaloid carcinoma of the breast (BCB) is an unusual neoplasm composed of basal-type neoplastic cells similar to those found in adenoid cystic carcinoma (ACC), although lacking distinctive features such as a cribriform pattern, a dual neoplastic population (epithelial-myoepithelial/basaloid), and stromal deposits of basement membrane-like material. In this article, we present 9 cases of breast cancer showing overall/predominant basaloid morphology. Patients' ages ranged from 47 to 75 years (mean, 61.4 years). Surgical treatment included mastectomy or quadrant excision with or without axillary dissection. Most tumors had a circumscribed outline and ranged in size from 1.3 to 5.5 cm (mean, 2.5 cm). Microscopically, they featured sheets, nests, and cords of proliferating basaloid tumor cells with ovoid, hyperchromatic nuclei with inconspicuous nucleoli and scant cytoplasm. No foci with characteristics of ACC were found in any of the tumors. Transition into pleomorphic basaloid carcinoma with foci of high-grade ductal carcinoma in situ plus infiltrating ductal carcinoma (IDC) and admixture with grade 3 ductal and sarcomatoid carcinoma was seen in 2 cases. Tumor cells were positive for wide-spectrum keratins and epithelial membrane antigen (9/9) and high-molecular-weight keratins (7/9). They were negative for smooth muscle actin, p63, calponin, and CD10 in all tested cases. Estrogen receptor, progesterone receptor, and HER-2 were negative. Axillary lymph node metastases were seen in 3 cases. At follow-up (range, 10-169 months), 5 patients were alive, 1 with evidence of contralateral breast cancer. Three patients died: one of disseminated BCB metastases, another of liver cirrhosis, and one of disseminated estrogen receptor/progesterone receptor-positive contralateral IDC. One patient was lost to follow-up. We concluded that BCB has some phenotypic and immunohistochemical features enabling its distinction from ACC or IDC. It appears to be a morphological and possibly a clinical entity. Compared with ACC, BCB appears to be more aggressive and may entail a more guarded prognosis.
-
本帖最后由 于 2010-09-09 19:01:00 编辑
Mod Pathol. 2005 Oct;18(10):1277-82.
Immunoreactivity for c-kit and p63 as an adjunct in the diagnosis of adenoid cystic carcinoma of the breast.
Mastropasqua MG, Maiorano E, Pruneri G, Orvieto E, Mazzarol G, Vento AR, Viale G.
Division of Pathology and Laboratory Medicine, European Institute of Oncology and University of Milan, School of Medicine, Milan, Italy.
Adenoid cystic carcinoma of the breast represents a unique clinicopathologic entity with a variable histological appearance and a relatively indolent clinical course in most of the cases. Adenoid cystic carcinoma may be difficult to differentiate from infiltrating duct carcinomas, and in particular from tubular and cribriform carcinomas, especially in core or vacuum-assisted biopsies. We evaluated the prevalence of c-kit, p63, and e-cadherin immunoreactivity in a series of 20 adenoid cystic carcinomas, comparing the results with those obtained in a series of infiltrating tubular carcinomas and infiltrating cribriform carcinomas. The hormone receptor status, proliferation labeling index, and HER/2 immunoreactivity had been previously investigated in all the cases. Three (15%) adenoid cystic carcinomas and all infiltrating tubular and cribriform carcinomas showed estrogen receptor and/or progesterone receptor immunoreactivity (P < 0.00001 for estrogen and P = 0.00002 for progesterone receptors). Adenoid cystic carcinomas consistently lacked any immunoreactivity for HER/2, whereas three (15%) infiltrating and cribriform carcinomas showed weak and incomplete membrane staining (P = 0.23077). Membranous immunoreactivity for c-kit was found in all except one (predominantly basaloid) adenoid cystic carcinomas (95%), and in none of the infiltrating tubular and cribriform carcinomas (P < 0.00001). Nuclear immunoreactivity for p63 was found in all except three (predominantly basaloid) adenoid cystic carcinomas (85%) and in none of the infiltrating tubular and cribriform carcinomas (P < 0.00001). All infiltrating tubular and cribriform carcinomas and 18/20 (90%) adenoid cystic carcinomas showed immunoreactivity for e-cadherin (P = 0.48718). In summary, adenoid cystic carcinomas showed the following phenotype: estrogen receptor-/progesterone receptor-/c-kit+/p63+ (13 cases, 65%), estrogen receptor-/progesterone receptor/c-kit+/p63- (three cases, 15%), estrogen receptor-/progesterone receptor-/c-kit-/p63+ (one case, 5%), estrogen receptor+/progesterone receptor+/c-kit+/p63+ (two cases, 10%), and estrogen receptor+/progesterone receptor-/c-kit+/p63+ (one case). By contrast, all the infiltrating tubular and cribriform carcinomas showed the estrogen receptor+/progesterone receptor+/c-kit-/p63- phenotype. Our data provide evidence that immunoreactivity for c-kit and/or p63 may be useful in differentiating adenoid cystic carcinomas from other types of breast cancer.
-
本帖最后由 于 2010-09-09 19:02:00 编辑
Radiologia. 2006 Jul-Aug;48(4):235-40.
[Adenoid cystic carcinoma of the breast]
[Article in Spanish]
de Luis E, Apesteguía L, Noguera JJ, Pina L, Martínez-Regueira F, Miguel C, Sáenz J.
Servicio de Radiología, Clínica Universitaria de Navarra, Pamplona, España. edeluis@unav.es
OBJECTIVE: To review the clinical presentation and imaging findings of adenoid cystic carcinoma (ACC). MATERIAL AND METHODS: We performed a retrospective study of the period between January 1990 and July 2004, comprising five cases of ACC of the breast, all in women, among 4,036 malignant lesions diagnosed (0.12%). We reviewed the available imaging studies (mammography in all five cases, ultrasound in four, and magnetic resonance in one). We also reviewed the clinical presentation and evolution in all patients. RESULTS: Three patients presented with palpable lesions. Mammographic findings consisted of irregular, ill-defined nodules in three cases, a well-defined rounded nodule in one, and an asymmetrical density in the other. No microcalcifications were observed in any case. Ultrasound examination showed ill-defined polylobulated nodules in three cases and a well-defined, rounded nodule with small cysts inside in the remaining case that showed intense vascularization in the Doppler study. The only case studied by magnetic resonance was seen as a rounded nodule that showed heterogeneous contrast uptake, well-defined margins, and an enhancement curve considered highly suspicious for malignancy. Treatment was tumorectomy together with radiotherapy in all cases. Four patients remain asymptomatic at present (mean follow-up = 64 months) and one presented lung and liver metastes twelve years after the diagnosis of ACC. CONCLUSION: ACC is an uncommon breast tumor with varied radiologic appearance, although moderately or highly suspicious lesions predominate. We consider the absence of microcalcifications in these tumors to be noteworthy. The prognosis is generally good, although the possibility of remote metastasis exists.
-
本帖最后由 于 2010-09-09 19:02:00 编辑
Mod Pathol. 2006 Oct;19(10):1351-7. Epub 2006 Jun 30.
Immunophenotypic overlap between adenoid cystic carcinoma and collagenous spherulosis of the breast: potential diagnostic pitfalls using myoepithelial markers.
Rabban JT, Swain RS, Zaloudek CJ, Chase DR, Chen YY.
Department of Pathology, University of California, San Francisco, CA 94143, USA. joseph.rabban@ucsf.edu
Adenoid cystic carcinoma of the breast is a rare neoplasm whose cribriform architecture may mimic invasive cribriform carcinoma, cribriform ductal carcinoma in situ, and collagenous spherulosis. The diagnosis may be even more challenging in needle core biopsies. Immunohistochemical expression of p63 and c-kit distinguishes adenoid cystic carcinoma from invasive cribriform carcinoma and ductal carcinoma in situ. A formal comparison of the immunophenotype of adenoid cystic carcinoma to collagenous spherulosis has not been reported. Of concern is the overlap in myoepithelial markers between these two entities. Both may express S100, smooth muscle actin, and p63. This overlap may cause diagnostic confusion yet is under-emphasized in the literature. The expression profile of newer myoepithelial markers has not been studied in this setting. We evaluated smooth muscle actin, p63, calponin, smooth muscle myosin heavy chain, as well as c-kit, in nine cases of cribriform pattern adenoid cystic carcinoma of the breast in comparison to 12 cases of collagenous spherulosis. Both entities strongly expressed p63 and smooth muscle actin; in adenoid cystic carcinoma, the basaloid myoepithelial-like tumor cells expressed these markers, but the ductular epithelial cells did not. Neither calponin nor smooth muscle myosin heavy chain was expressed in adenoid cystic carcinoma but both were strongly expressed in collagenous spherulosis. Whereas the ductular epithelial cells of adenoid cystic carcinoma were positive for c-kit in all cases, collagenous spherulosis was negative for c-kit. Positive p63 expression by a cribriform breast lesion is not sufficiently specific to confirm a diagnosis of adenoid cystic carcinoma. A broader panel that includes calponin or smooth muscle myosin heavy chain and c-kit is required to exclude collagenous spherulosis in settings in which the distinctive morphologic features that separate these entities are not conspicuously present. Reliance on p63 or smooth muscle actin alone poses a potential diagnostic pitfall in evaluating cribriform breast lesions.
-
本帖最后由 于 2010-09-09 19:02:00 编辑
Pathol Res Pract. 2005;201(10):705-11. Epub 2005 Sep 28.
Solid variant of mammary "adenoid cystic carcinoma with basaloid features" merging with "small cell carcinoma".
Cabibi D, Cipolla C, Maria Florena A, Fricano S, Barresi E, Vieni S, Rodolico V, Napoli L.
Institute of Pathology, A.O.U. Policlinico Paolo Giaccone, Via del Vespro 129, 90127 Palermo, Italy. cabibidaniela@virgilio.it
We describe a rare case of a solid variant of a mammary adenoid cystic carcinoma with basaloid features (sbACC) and its coexistence with a "small cell" carcinoma (SCC), identified and confirmed by histological and immunohistochemical observations: the absence of glandular structures and PAS-positive globules, positivity for neuroendocrine markers (NSE, synaptophysin and chromogranin), and negativity for 34betaE12 and SMA actin were the aspects suggesting the presence of SCC. Furthermore, positivity for CD10 was found both in sbACC and in SCC, supporting the hypothesis that the two components share the same histogenetic myoepithelial origin and represent an example of dedifferentiation along neuroendocrine phenotype lines occurring in a multipotential neoplastic stem line, already committed towards a myoepithelial phenotype. To our knowledge, this is the first reported case of a solid basaloid adenoid cystic carcinoma merging with an SCC carcinoma. Furthermore, it is the first study in which CD10 was used to investigate the histogenesis of the two neoplastic components.
-
本帖最后由 于 2010-09-09 19:02:00 编辑
Mod Pathol. 2005 Dec;18(12):1623-31.
KIT is highly expressed in adenoid cystic carcinoma of the breast, a basal-like carcinoma associated with a favorable outcome.
Azoulay S, Laé M, Fréneaux P, Merle S, Al Ghuzlan A, Chnecker C, Rosty C, Klijanienko J, Sigal-Zafrani B, Salmon R, Fourquet A, Sastre-Garau X, Vincent-Salomon A.
Department of Pathology, Institut Curie, Paris Cedex, France.
Recent biological studies have classified breast carcinomas into HER2-overexpressing, estrogen receptor-positive/luminal, basal- and normal-like groups. According to this new biological classification, the objectives of our study were to assess the clinical, morphologic and immunophenotypic characteristics of adenoid cystic carcinoma of the breast in order to classify this subtype of breast carcinoma. A total of 18 cases of adenoid cystic carcinoma were identified from the Institut Curie files. Clinical information was available for 16 patients with a median follow-up of 6.5 years. Morphologically, all tumors were graded according to the system defined by Kleer and Oberman (histologic and nuclear grade). Immunophenotype was assessed with anti-ER, PR, HER-2, KIT, basal (CK5/6) and luminal cytokeratins (CK8/18) and p63 antibodies. One out of 18 tumors was nuclear grade 1 (16%), nine were nuclear grade 2 (50%) and eight were nuclear grade 3 (44%). All cases were estrogen receptor, progesterone receptor and HER-2 negative. Epithelial cells were strongly positive around glandular lumina with one or both cytokeratins, identifying the coexistence of CK5/6+ cells, CK5/6 and CK8/18+ cells, CK8/18+ cells and p63+ cells. All cases (100%) were also KIT positive. In all, 15 patients were treated by surgery. Nine of them received adjuvant radiotherapy. Follow-up was available for 16 patients. In all, 14 patients were alive. Two of them, initially treated by surgery only, presented a local recurrence. Two patients died (one of them treated by radiation therapy only died from her disease). Our study shows that adenoid cystic carcinoma of the breast is a special, estrogen receptor, progesterone receptor, HER-2 negative and highly KIT-positive, basal-like breast carcinoma, associated with an excellent prognosis. This highly specific immunophenotype could be useful to differentiate adenoid cystic carcinoma of the breast from other subtypes of breast carcinoma such as cribriform carcinoma.
-
本帖最后由 于 2010-09-09 19:03:00 编辑
Am J Clin Pathol. 2005 Nov;124(5):733-9.
Expression of c-kit in adenoid cystic carcinoma of the breast.
Crisi GM, Marconi SA, Makari-Judson G, Goulart RA.
Department of Pathology, Baystate Medical Center/Tufts University School of Medicine, Springfield, MA 01199, USA.
Breast adenoid cystic carcinoma (BACC) is a biologically distinct tumor with morphologic mimickers, which might make accurate classification problematic. Because c-kit expression has been reported in adenoid cystic carcinoma of various anatomic sites, we evaluated BACC for c-kit by immunohistochemical analysis, comparing the findings to similarly stained mimickers. Tested cases included 6 BACCs, 15 low-grade infiltrating ductal carcinomas (LGIDCs) chosen as potential mimickers, and 15 head-neck adenoid cystic carcinomas (HNACCs). All BACCs showed plasma membranous and cytoplasmic staining equal to or greater than that of adjacent benign epithelium. Five BACCs (83%) expressed c-kit in more than 50% of tumor cells. Only 2 of 15 LGIDCs expressed low-intensity, focal c-kit staining. Of the 15 HNACCs, 10 (67%) expressed c-kit. Hormone receptors were consistently negative in BACCs. All BACCs expressed c-kit, whereas LGIDCs infrequently expressed low-intensity c-kit. Immunohistochemical evaluation for c-kit might aid in accurately classifying carcinomas with histologic features overlapping adenoid cystic carcinoma and LGIDC.
Above abstracts are for some ones who are interested to breast ACC related lesions.
For this case:
It is not like classic ACC. It can be ACC solid type with basaloid features, or BCB.
This kinds of lesions are rare. I just read less than 10 cases of ACC and one or two BCB. I do not have much experience about them. Wish more people share your oppinion.
Also hope 楼主let us know your IHC and interpretation. Thanks, cz
-
本帖最后由 于 2010-01-01 08:59:00 编辑
非常感谢Zhao医师的评论和有关乳腺基底样细胞癌的文献. 我把 "Basaloid carcinoma of breast" 翻译成"乳腺基底细胞样癌" 是为了避免读者将"Basal-like" 与 "Basaloid"混淆., 因为二者有着本质的区别. "Basal-like" 是指免疫表型( CK5/6+和/或CK14+)和基因表达谱与乳腺基底细胞相似, 形态学表现为高级别浸润性导管癌,IHC标记ER-PR-HER2-,临床预后差. 阅读上述文献摘要(未看全文及图片是草率的),作者提出"乳腺基底细胞样癌"是认为乳腺BCB与ACC在形态(无典型ACC)和免疫表型(非肌上皮 SMA-p63-calponin-CD10-)不同,预后比ACC差(3例死于肿瘤,一例带瘤生存).并注意到9例BCB中一例与导管原位癌有过渡;2例伴有3级浸润性导管癌.此外"三阴(triple negative)"的术语应严格用于高级别浸润性乳腺癌免疫表型ER-PR-Her2-的病例,提示预后比"非三阴癌"差. 就此例耒讲:鉴别诊断的焦点主要为:乳腺ACC-实体性, 乳腺BCB,和乳腺恶性圆柱瘤.尚不明确的是Rosen 乳腺病理学第3版第600页Fig 25.21图示中的A-C(Adenpoid cystic carcinoma, high grade: cylindromatous nodules are present in this basoloid tumor) 与 上述文献上"Basoloid carcinoma of breast" 在形态上是否是一回事? 鉴别无疑可用IHC标记,但是对这些少见肿瘤的研究仅是"初级阶段"

- xljin8
















