| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
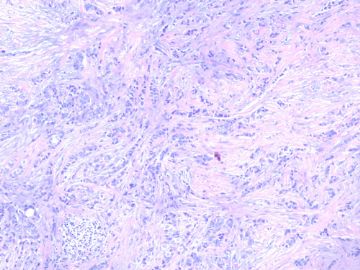
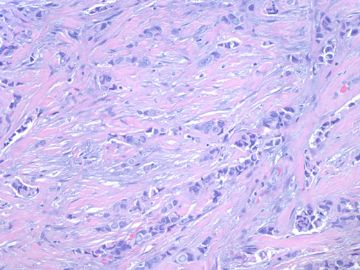
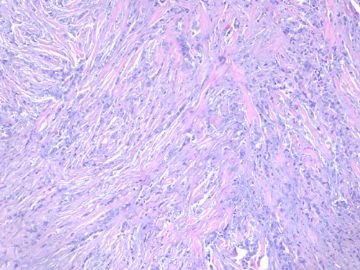
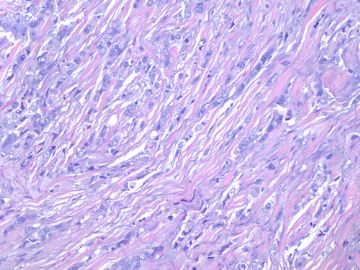
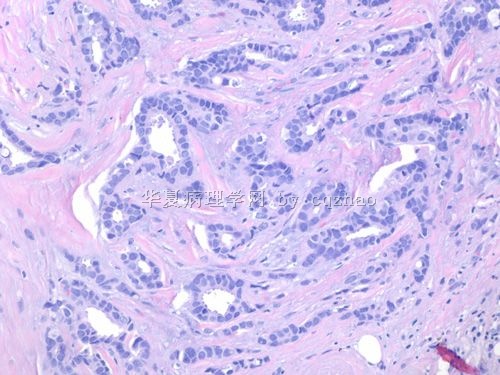
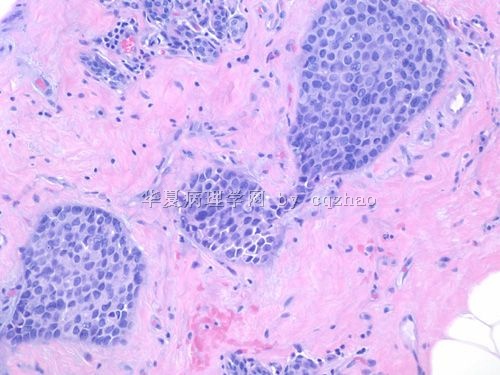
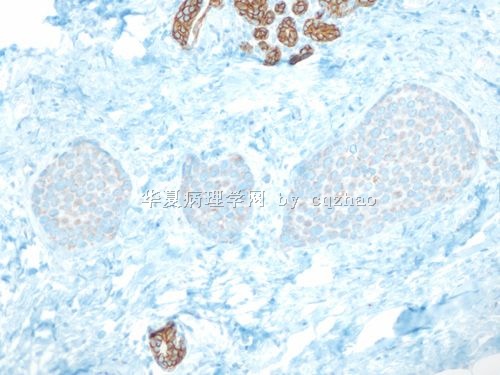
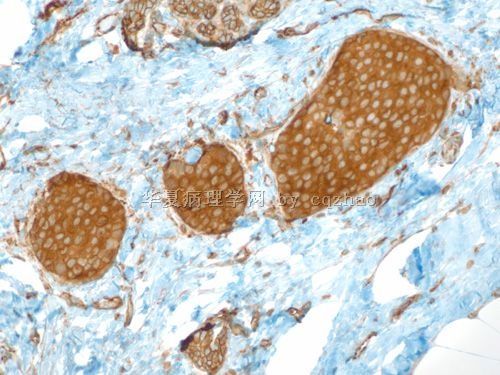
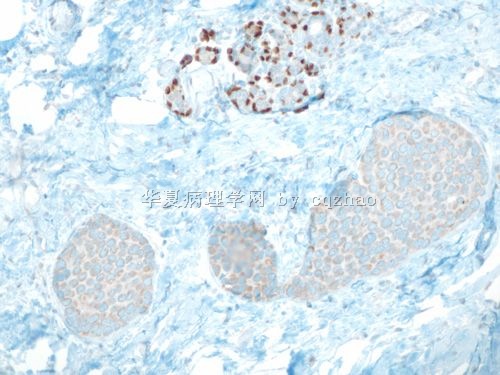
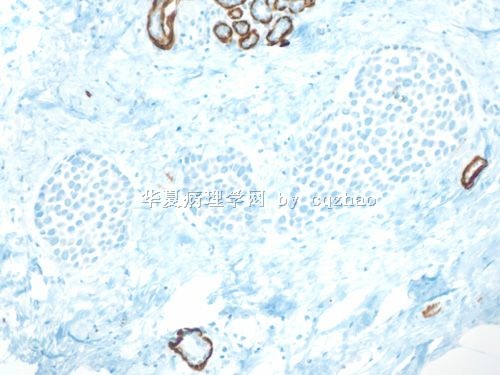
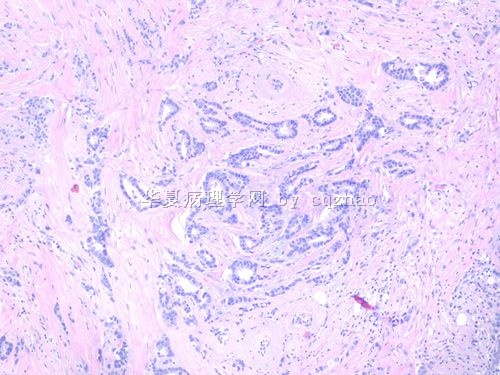
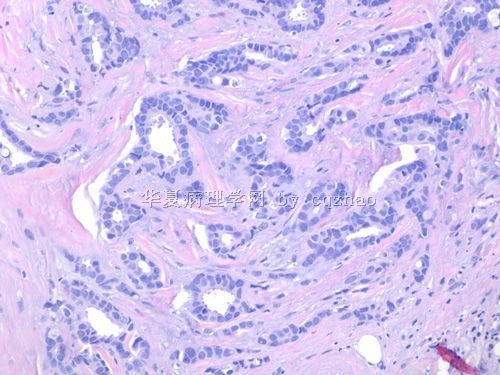
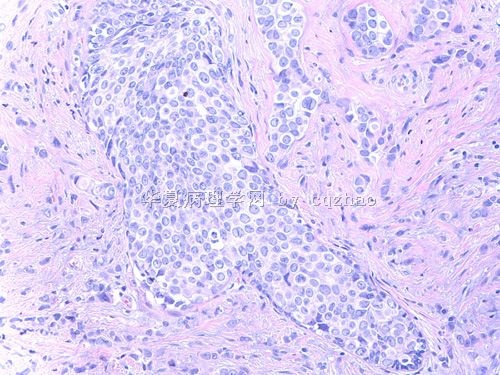
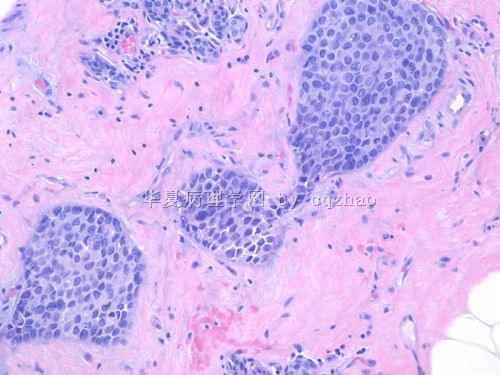
- B2280小叶癌with focal 小管structure(cqz-28)(11-6-09)
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
50 岁妇女乳腺肿瘤2.5cm
. Fig 1-4. most areas of the tumor.
-
本帖最后由 于 2009-12-16 11:07:00 编辑
相关帖子
- • 女性/45岁 右侧乳腺肿块 诊断?
- • 左乳肿块,新加免疫组化
- • 乳癌?求助
- • 乳腺肿瘤
- • 够小叶癌吗?
- • 女 48岁 左侧乳腺肿块10余天
- • 女性 60岁乳腺肿块 乳腺癌分型
- • 乳腺穿刺
- • 右乳肿块
- • 右乳腺肿块穿刺活检,新加手术后图片
There are two ways to determine the nature of the tumors, ductal vs lobular in some cases. Some people think they should be decided based on the cytomorphology and others think they should be decided based on E-cadhere stains. This is why some people including Dr. Schnit though some lobular ca can be E-Cadherin positive.
I favor they should be dicided by IHC. IHC is more objective than morphology only.
For my case I just call invasive lobular ca and I did not mention the focal 伴随小管癌样结构. Clinically it is no difference. I do not want to make the clinicians confused. Many invasive ductal ca with lobular growth pattern. We just call them as invasive ductal ca and never mention them with invasive ductal ca with lobular growth pattern.
The term of tubulolobular carcinoma is not widely accepted. If we read the original relatied papers carefully we will notice that all cases of tubulobular ca are E-Cadherin positive. So I think tubulolobular ca is just a varaint of ductal ca and no relation to lobular ca.
Now what is your diagnosis for the main tumor?
1. Tubulobular ca ?
2. Mixted lobular and tubular ca?
3. Lobular ca?
4. Is E-cadherin positive or negative in tubulobular ca (people called)?
5. Is tubulobular ca in the WHO calssification of breast ca?
6. How many cases of tubulobular ca did you see in your clinical practice?
| 以下是引用xljin8在2009-11-18 6:27:00的发言: 2008-04-23 abin医师对浸润性小叶癌做了非常详尽的组织学和细胞学总结, 使我受益非浅。我把它储存在收藏夹量,以便温故知新。 更是敬佩Dr. Chao 乳腺病理诊断的丰富经验和非常感激对国内病理医师的仔细讲解和示教。 |
| 以下是引用xljin8在2009-11-14 13:17:00的发言:
非常感兴趣的病例,但是我有些疑问: 1)文献中有tubulolobular carcinoma 的名称,应该如何理解? 2)能否提供小管癌区域的免疫组化标记片? 3)诊断时是否因为浸润性小叶癌的恶性程度高而可忽略其他成分? |
Thank for your attention.
1) + 2): will show the IHC results of other areas and have some discussion one by one.
3)诊断时是否因为浸润性小叶癌的恶性程度高而可忽略其他成分?
No. We report all abnormal lesions in the reports in our hospital.
For example:
Invasive ductal or lobular ca
in site ca (DCIS or LCIS)
Atypical lesions: ADH, ALH, atypical papilloma, FEA
Will have one dx line to include all non-neoplastic breast lesions such as FCC, sclerosing adenosis, introductal papilloma, UDH, radial scar, CCC, calcification....
-
本帖最后由 于 2009-11-14 01:00:00 编辑
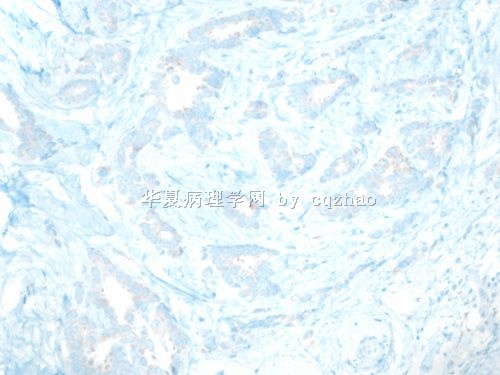
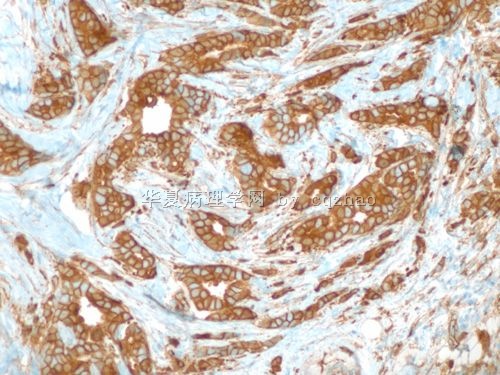
All of you are right about the tumor.
Stains for the main tumor or fig1 (question 1)
E-cad and P120
interpretaion of P120: lobular lesion-cytoplasmic stain; ductal lesion-membrane stain.
We will have the answers for others one by one soon.
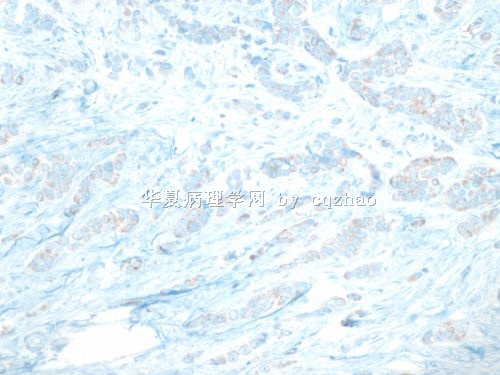
名称:图1
描述:图1
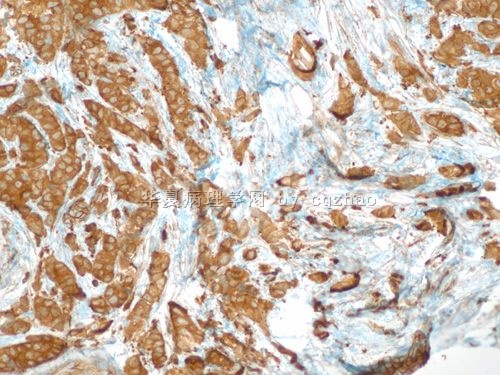
名称:图2
描述:图2
| 以下是引用SOS991229在2009-11-11 23:26:00的发言:
我们在平常工作中也会出现这种情况,我们就冠个总名:浸润性癌,部分区域为浸润性小叶癌,部分区域为浸润性导管癌。不知道赵老师那边是怎样规范的报告?还有是否国外在报告ER,PR时要报%吗?就像ki-67那样+>30%之类的吗?谢谢您! |
We do er/pr/her2/ki67 for all cases of invasive breast ca
I mentioned Her2 report before. I think the Her2 reort is similar among most hospitals in China and the US.
Currently we report ER/PR and ki67 as following.
ER/PR: H score:
example:
ER positive, H score 240 (0 10%; 1+10%; 2+10%; 3+70%)
H score count: (3x70=210)+(2x10=20)+(1x10=10)+(0x10=0) =240
Tumor cell proliferation index (Ki67):
Result 40%,
Index high (low: to 10%; moderate:11-25%; high:26-50%; very high:>50%)
Magee is a breast and gynecologic center. Our reports are very detailed. The report systems can be very variable in different hospitals.
Just for your reference
-
本帖最后由 于 2009-11-09 19:33:00 编辑
This is one of my cases of today. Take some photos to share with you if you are interested.
The photos 1-4 represent the 2.5 cm tumor. There are several focal lesions admixed with the tumor.
Question:
1. what is the dx of tumor (fig 1-4)?
2. what is dx of tumor nests in the area 2?
3. What is dx of tumor nests in the area 3?
4. What are the focal tubular structures in the area 4?
Good weekend for every one. cz
abin译:这是我今天的一个病例。上传一些照片分享,如果你有兴趣。
图片1-4代表2.5cm肿瘤。有数个病灶与肿瘤混杂。
问题:
1、肿瘤诊断什么?(图1-4)
2、第2个区域的肿瘤巢诊断什么?
3、第3个区域的肿瘤巢诊断什么?
4、第4个区域的局灶管状结构是什么?
祝大家周末快乐!cz