| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
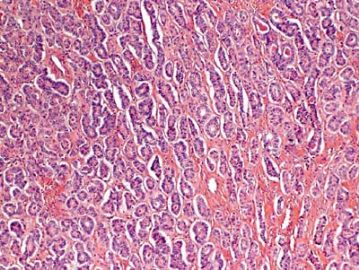
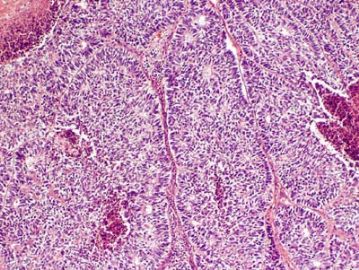
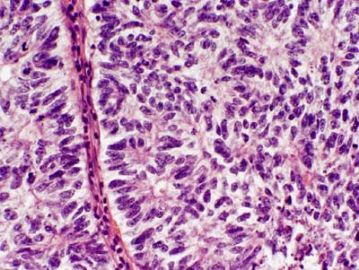
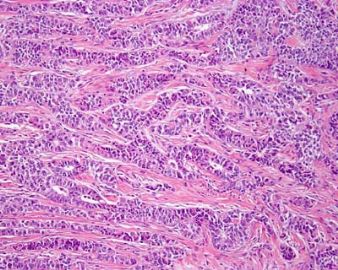
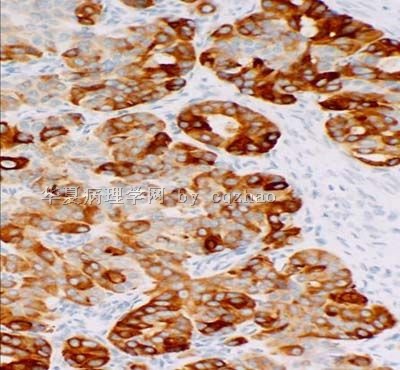
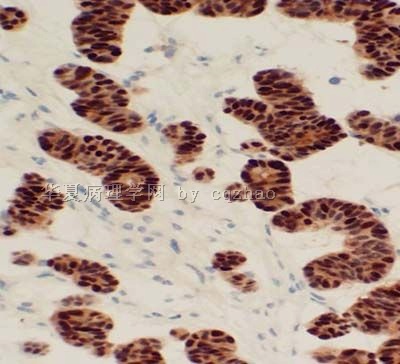
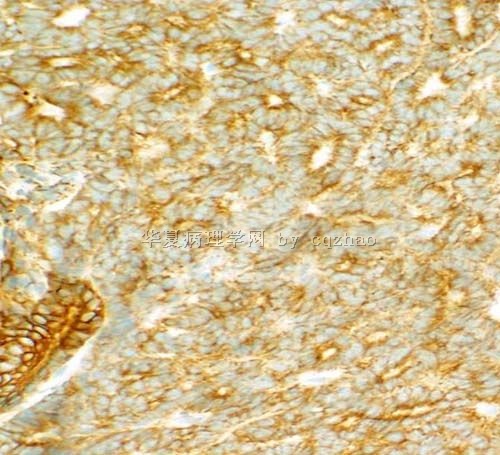
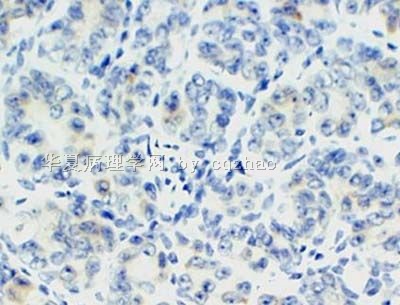
- 卵巢Sertoliform (or sex cord-like) variant of 子宫内膜样癌 (cqz-3)
-
Arch Pathol Lab Med. 2005 Oct;129(10):1288-94.
-
- Erratum in:
- Arch Pathol Lab Med. 2008 Aug;132(8):1222. Okamura, Mitsue [corrected to Muraoka, Mitsue].
Granulosa cell tumor-like variant of endometrioid carcinoma of the ovary exhibiting nuclear clearing with biotin activity: a subtype showing close macroscopic, cytologic, and histologic similarity to adult granulosa cell tumor.
Department of Surgical Pathology, Tokyo Women's Medical University Medical Center East, Tokyo, Japan. fujibasp@dnh.twmu.ac.jp
CONTEXT: The sex cord-like variant of endometrioid carcinoma of the ovary shows many similarities to Sertoli-Leydig cell tumor and granulosa cell tumor. However, few cases of the granulosa cell tumor-like variant have been reported, suggesting this tumor might often be hidden under the diagnosis of granulosa cell tumor. OBJECTIVE: To investigate the similarities and differences between the granulosa cell tumor-like variant of endometrioid carcinoma and granulosa cell tumor of the ovary and to evaluate a newly observed feature, namely, nuclear clearing (or optically clear nuclei), in this variant tumor. DESIGN: A comparative macroscopic, cytologic, histopathologic, and immunohistochemical study in specimens obtained from the following patients: 1 patient with granulosa cell tumor-like variant of endometrioid carcinoma diagnosed by frozen section examination, 3 patients with granulosa cell tumor, and 6 patients with classic endometrioid carcinoma. RESULTS: The granulosa cell tumor-like variant showed close macroscopic, cytologic, and microscopic similarities to granulosa cell tumor. However, the 2 tumors could be differentiated immunohistochemically. The former also showed intense staining for progesterone receptors and contained nonmorular nests that exhibited the so-called nuclear clearing with biotin activity. CONCLUSION: Because the granulosa cell tumor-like variant is pathologically similar to granulosa cell tumor, showing only some dissimilarities to the latter, it can easily be misdiagnosed if the possibility of this variant is not kept in mind. Identification of the typical endometrioid histologic features or related lesions or immunohistochemistry may lead to a proper diagnosis. The observation of nuclear clearing with biotin activity in nonmorular nests suggests that this tumor has endometrioid epithelial characteristics.
-
Mod Pathol. 1999 Oct;12(10):933-40.
-
Sertoliform endometrioid carcinomas of the ovary: a clinicopathologic and immunohistochemical study of 13 cases.
Department of Pathology, Institud d'Investigacions Biomèdiques August Pi i Sunyer, Hospital Clinic, Facultat de Medicina, Universitat de Barcelona, Spain.
Ovarian endometrioid carcinomas with sertoliform features (SECs) are infrequent and often misinterpreted as sex cord-stromal tumors. The clinicopathologic features and immunohistochemical expression of keratin, epithelial membrane antigen (EMA), inhibin, and estrogen and progesterone receptors were evaluated in 13 cases of SEC. The women were 41 to 89 years of age (mean, 60 yr) with abdominal enlargement secondary to a unilateral ovarian mass as the most frequent clinical presentation. One patient displayed virilization. At presentation, 10 patients were Stage I, one was Stage II and two were Stage III. The tumors were composed of compact anastomosing cords and small tubules embedded within a fibrous stroma. Nuclear features were Grade 1 or 2 in all but one tumor. Areas of conventional endometrioid carcinoma were observed in 12 cases. An adenofibromatous component comprising 5 to 60% of the lesion was present in seven cases. All 12 cases examined immunohistochemically were positive for keratin and EMA and negative for inhibin with focal, luteinized stromal cells positive for inhibin in 10 cases. Estrogen and progesterone receptors were positive in 10 and 11 cases, respectively. Follow-up on 6 of 10 patients with Stage I and the one patient with Stage II disease displayed no evidence of disease 10 to 120 months (mean, 57 mo). Progressive disease and death occurred at 12 and 72 months only in the two women with Stage III disease, one of which had an associated serous carcinoma in the contralateral ovary. Adequate sampling, a careful search for areas of conventional endometrioid carcinoma, and immunohistochemical studies (including EMA, keratin, and inhibin) are helpful in the evaluation of ovarian tumors with sex cord-stromal features. SEC should be considered a well-differentiated endometrioid carcinoma despite the presence of a solid, sex cord-like proliferation, with a good prognosis when confined to the ovary.
-
Int J Gynecol Pathol. 1996 Apr;15(2):119-26.
-
Sertoliform endometrial adenocarcinoma: a study of four cases.
James Homer Wright Pathology Laboratories, Massachusetts General Hospital, Boston 02114, USA.
We studied four endometrial carcinomas with a conspicuous component that resembled patterns in Sertoli cell tumors. The patients presented at age 44-83 years (mean 65 years), with abnormal or postmenopausal vaginal bleeding in three and abnormal cervical cytology in one. All were multiparous, moderately to markedly obese, and hypertensive, and three patients had non-insulin-dependent diabetes mellitus. One tumor was suspected to be an endometrial stromal sarcoma with sex-cord-like differentiation on biopsy. Gross examination of the hysterectomy and bilateral salpingo-oophorectomy specimens showed solid polypoid endometrial tumors in each case. Light microscopic examination showed three to be superficially invasive of the myometrium and one to be confined to the endometrium; none of the tumors showed the tongue-like pattern of myoinvasion or the angiolymphatic invasion characteristic of low-grade endometrial stromal sarcomas. The sertoliform component, which predominated in one case and was only focal in the three others, was composed of uniform small hollow tubules lined by columnar cells with apical cytoplasm and of compact slender cords. The tubules and cords were often present between benign-appearing or carcinomatous glands. In the case with predominate sertoliform areas, the lesional cells had clear cytoplasm suggesting a lipid-rich variant; special stains of this case demonstrated cytoplasmic glycogen but no fat. In none of the cases was cytoplasmic mucin, argyrophil granules, or argentaffinity demonstrated. The nonsertoliform areas of the tumors consisted of typical endometrioid adenocarcinoma; concurrent endometrial hyperplasia was also present in each case. Squamous differentiation and minor foci of anaplastic carcinoma with bizarre tumor giant cells were present in three tumors. Immunoperoxidase stains showed staining for two or more markers of epithelial or glandular differentiation in the sertoliform areas in all cases (keratin, epithelial membrane antigen, carcinoembryonic antigen, CA125, Tag72), with focal expression of vimentin in all cases. In none of the cases was desmin or actin staining observed. The evidence indicates that tumors in this series are variants of endometrioid adenocarcinoma and are distinct from uterine tumors resembling ovarian sex-cord tumors and stromal sarcomas with sex-cord-like differentiation.
| 以下是引用wfbjwt在2009-8-31 12:41:00的发言: 抑制素、NSE、EMA。 |
Almost right.
抑制素 is the best marker for sex cord tumor, negative for epithelial tumors
EMA is 100% positive for epithelial tumors and always negative for sex cord tumor
Chromgranin is the best marker carcinoid in term of sensitivity and specificity.
Let's nerrow down the ddx:
1. sex cord tumor (granulosa cell tumor/sertoli cell tumor)
2. carcinoid tumor
3. Endometrioid carcinoma.
If you can only order three immunostains, which three stains will you ordered in order to separate these three categories of tumor?
-
southsheep 离线
- 帖子:15
- 粉蓝豆:1
- 经验:15
- 注册时间:2009-08-14
- 加关注 | 发消息
| 以下是引用3673566在2009-8-28 20:37:00的发言:
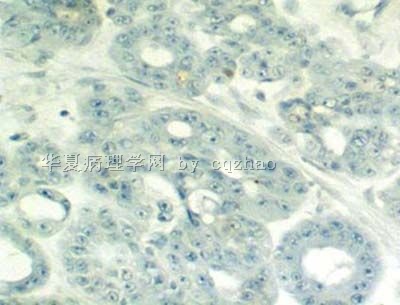
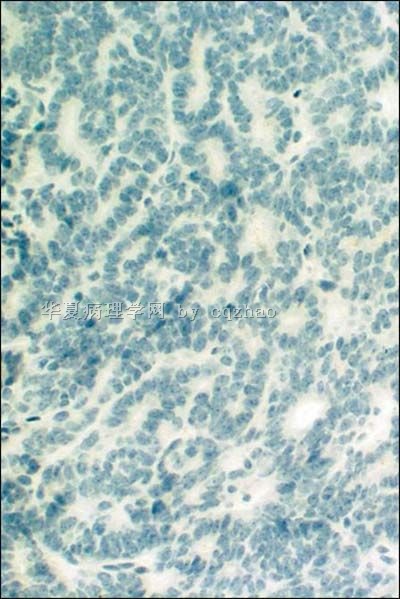
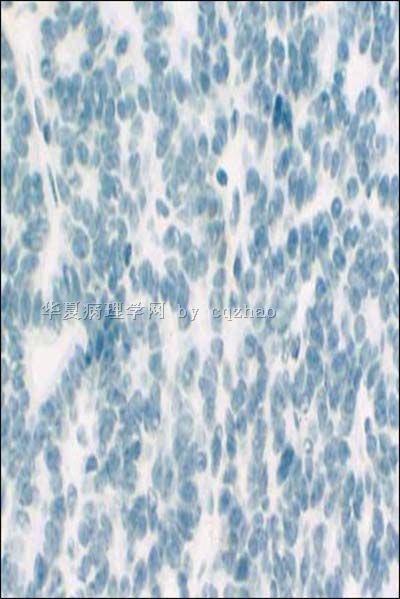
学习了各位前辈的精彩分析,获益匪浅! 除了前辈提到的诊断外,我再提一个:卵巢子宫内膜样腺癌Sertoli样变型(或称为类似性索-间质肿瘤的子宫内膜样腺癌)。依据:1)患者60岁,年龄较大;2)图1显示明确的腺管样结构,大小不等,部分有相互融合;3)图2-图4显示实性片巢状、梁索状结构,但未见明确的Call-Exner小体及咖啡豆或石榴籽样细胞;4)需鉴别类癌、性索间质肿瘤。除仔细寻找子宫内膜样腺癌的其他特征(如有无鳞化)外,需做免疫组化PCK、CK7、EMA、Inhibin、CgA、syn等鉴别。 |
-
Sertoli cell tumors of the ovary: a clinicopathologic and immunohistochemical study of 54 cases.
James Wright Pathology Laboratories, Massachusetts General Hospital, Harvard Medical School, Boston, MA 02114, USA. eoliva@partners.org
Ovarian Sertoli cell tumors are rare, and their morphologic spectrum, behavior, and factors influencing the latter are not clearly established. They may be mimicked by many different tumors, some of them more frequent than Sertoli cell tumors; immunohistochemistry may aid in this differential, but its role has not been analyzed in a large series. We studied the clinicopathologic features of 54 Sertoli cell tumors, including the immunohistochemical profile of 23 of them. The patients, 6 of whom had Peutz-Jeghers syndrome, ranged from 2 to 76 years of age (mean, 30 years). Eleven patients had estrogenic and 4 had androgenic manifestations. The tumors ranged from 0.8 to 30 cm, with the majority being in the range of 4 to 12 cm. They were all unilateral, usually solid, and often yellow. The predominant microscopic pattern was tubular, seen, albeit often only focally, in all tumors; other patterns were cords or trabeculae (28), diffuse (21), pseudopapillary (4), retiform (3), islands or alveolar arrangements (3), and spindled (3). The tubules were solid or hollow with the former being somewhat more common. Delicate septa were occasionally seen and were conspicuous in areas of one tumor. The stroma was abundant in 15 tumors with marked sclerosis in 4. The cells usually had pale to occasionally densely eosinophilic cytoplasm, but 6 tumors were composed of cells with prominent foamy cytoplasm, falling in the category of "lipid-rich" Sertoli cell tumor, and one had cells with clear non-foamy cytoplasm. Forty-four tumors were stage I (42 of them were stage Ia and 2 were stage Ic), 1 was stage II, 3 were stage III, and 6 were not adequately staged. Follow-up was available for 27 patients with stage I tumors, and all were alive and well at last follow-up except for 2 patients with stage Ia and 1 with stage Ic disease. Those 3 patients had pelvic-abdominal recurrences 18, 36, and 9 months, respectively, after the initial diagnosis. Two of the three clinically malignant stage I tumors had moderate to severe cytologic atypia and brisk mitotic activity (>5 or more mitoses/10 high power fields [HPFs]), and one of these had tumor cell necrosis. Among the 10 clinically benign stage I tumors with more than 5 years of follow-up, only 3 had >5 mitoses/10 HPFs, but none had more than mild cytologic atypia and none had tumor cell necrosis. Two of the three patients with stage III disease had follow-up information and one was alive at 16 months and the second developed splenic metastases 2 years after the initial diagnosis. Two of the three stage III tumors had at least moderate cytologic atypia and brisk mitotic activity. Immunohistochemical stains showed positivity for AE1/3-Cam5.2 in 15 of 23 tumors; Epithelial membrane antigen (EMA) was negative in all the tumors. Inhibin was positive in 18 of 22 tumors, calretinin in 10 of 20, CD99 in 19 of 22, vimentin in 17 of 18, smooth muscle actin in 4 of 18, neuron specific enolase in 8 of 16, S-100 in 2 of 20, and chromogranin was negative in all 21 cases studied. Although Sertoli cell tumors usually have a distinctive tubular pattern that facilitates the diagnosis, other patterns may occasionally predominate, causing confusion with various other primary and metastatic ovarian tumors. EMA, inhibin, and chromogranin represent the most helpful triad of immunomarkers serving to exclude two common mimics of Sertoli cell tumors (endometrioid carcinoma [inhibin-; EMA+; chromogranin-] and carcinoid tumor [inhibin-; EMA+; chromogranin+]). Although CD99 and calretinin are often expressed in these tumors, they are much less specific and not as helpful in the differential diagnosis. Most Sertoli cell tumors are stage I, unilateral, cytologically bland, and clinically benign, but occasional examples are high stage, and about 11% of stage I tumors have worrisome histologic features that may portend an adverse outcome. The tumors typically occur in young females, sometimes children who typically present with sexual precocity, and occasional patients have Peutz-Jeghers syndrome.
In term of morphologic study, this is the best and largest paper to describe ov sertoli cell tumor. If you want to know the morphologic features well, please read the original paper. I remeber that I once pasted this abstract some where in the web.
Am J Surg Pathol. 2005 Feb;29(2):143-56.
| 以下是引用wfbjwt在2009-8-28 19:15:00的发言:
|



 男性索(sertoli)+女性索(粒层)=两性母
男性索(sertoli)+女性索(粒层)=两性母











