| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
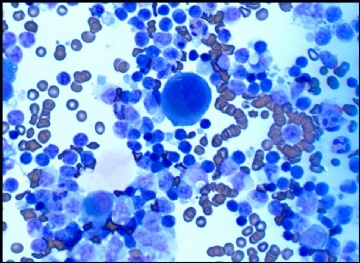
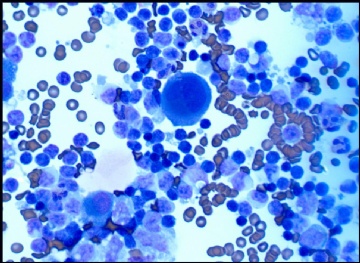
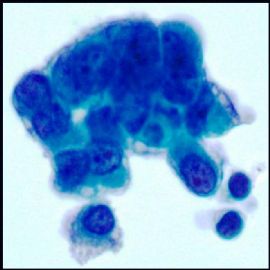
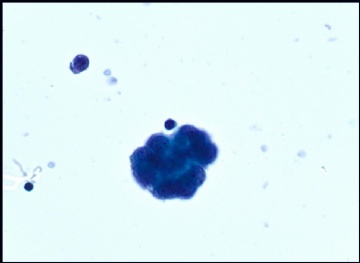
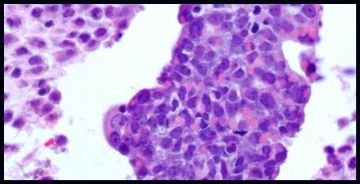
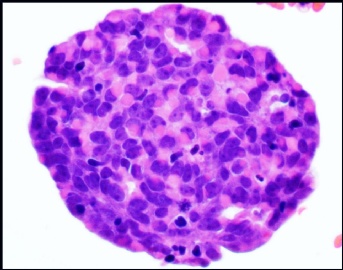
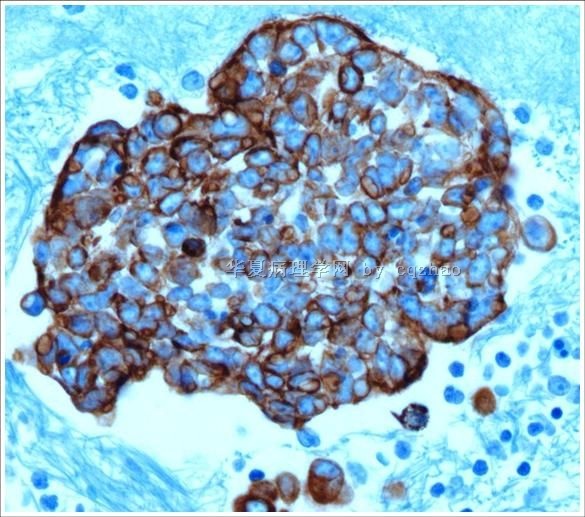
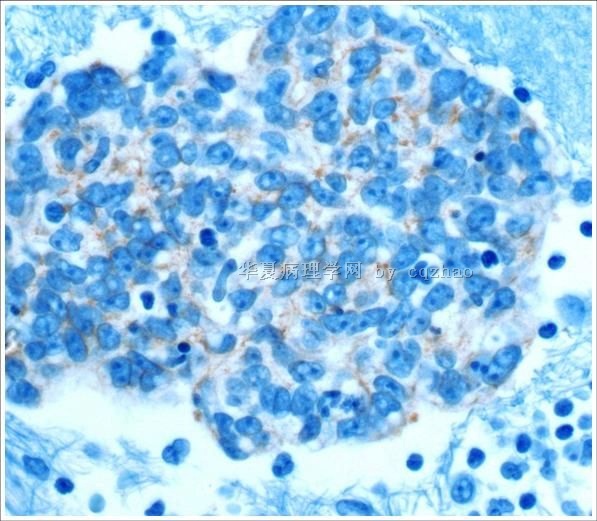
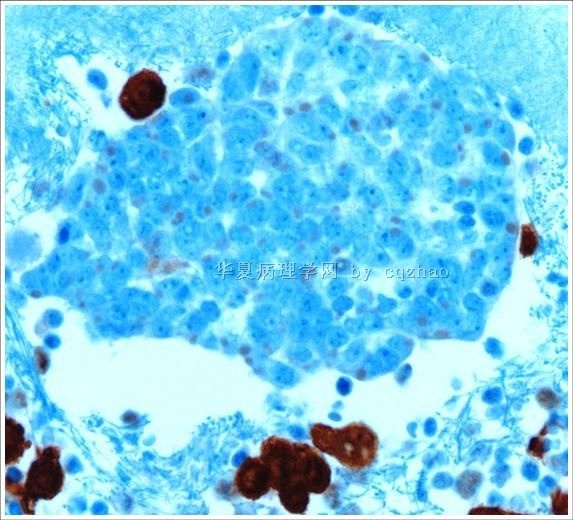
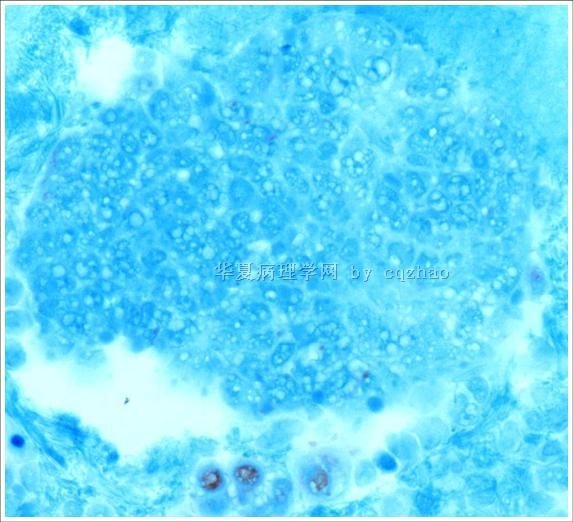
- 70 岁 妇女,胸水,metastatic adenoid cystic carcinoma from lung
-
蝴蝶兰dali2003 离线
- 帖子:11421
- 粉蓝豆:2441
- 经验:11985
- 注册时间:2009-09-06
- 加关注 | 发消息
-
本帖最后由 于 2009-09-10 06:58:00 编辑
Agree with above.
The work concept may be different in different work condition, sources. Currently in the USA, Pathologists (at least most) will try hard to identify the primary for body flood positive cases. For example patient has a lung mass with positive pleural flood, we will do ck7, ck20, TTF1 and try to confirm the lung primary. The pathologic diagnosis should include malignant or benign, also the possible origins. Even for the lung mass FNA, we also do some basic immuno panel to confirm the primay and types (squamou carcinoma, adenocarcinoma, small cell carcinoma).
-
本帖最后由 于 2009-08-07 11:55:00 编辑
cqzhao老师回复
看到大家发了好多体液细胞学的讨论病例,从中可以看出有些朋友对体液细胞学的诊断原则还不太清楚。
1.临床最常见的体液为胸膜腔积液和腹水。间皮细胞为单层扁平上皮。但是在很多反应性状态下,导致间皮细
胞增生,因此导致可见双核或多核、核分裂增加、核增大、核浆比增大、染色质增粗、核仁可见,甚至显著的
细胞非典型性。以上这些特征都类似肿瘤,可能误判为恶性,尤其是腺癌。
2.当看到不典型的腺样细胞时,必须注意排除这些细胞是不是反应性间皮细胞。这一点很重要。如果是间皮细
胞,那么就是良性的反应性的(当然少见的间皮瘤也是可能的)。如果是上皮细胞,那么可能是转移性癌细胞
(腹腔冲洗液时候要注意排除异位的子宫内膜)。
3.记住:有时候反应性间皮细胞可以看上去非常奇形怪状,有时候腺癌细胞又可能看上去像良性。
4.虽然细胞学形态、组织学检查、临床表现等非常有价值,但是在许多病例,免疫组化还是很重要的,尤其是
没有病史的病例。如果仅仅是靠镜下细胞型态学表现来做诊断,如果你是一个很厉害的细胞学诊断家的话,那么大部分 时候你会做的很好,但是在你的病理生涯中,出错将是难免的。
5.大部分时候,在体液细胞学中作出恶性诊断常可能是首次诊断。因此作为细胞病理
学家我们作出诊断的时候必须十分慎重。
6. 鉴别间皮细胞和上皮细胞又许多标记。
上皮细胞: BerEp4, MOC 31, B72.3, CEA et al
间皮细胞 (不管是反应性还是恶性): Calretinin, ck5/6, WT1 et al.
AE1/AE3, CK7, and EMA 在间皮细胞是阳性的. 因此它们对于鉴别是无帮助的。有些细胞病理学家对于一些疑
难病例喜欢选用两种上皮标记加两种间皮标记,因为有时候一些标记物的表达出现不同。比如有些病例中间皮
细胞MOC31是阳性的,而一些上皮细胞则berEp4或B72.4阴性。因此在作出诊断时候一定要结合实际病例。
7.如果排除了间皮来源,那么就要结合HE所见、临床以及影像学,甚至加做免疫组化来寻找恶性的原发灶。
8.恶性肿瘤性胸腔积液在男性最多见于肺癌,在女性最多见于乳腺癌。恶性腹水在男性则最多见于胃肠道来源
肿瘤,在女性则最多见于卵巢癌。
给sos老师的回复:
似我以前的发言,如果仅依据型态特点你可以大部分时间是正确的诊断,但是有时候也出错。对于体液细胞,我们的细胞技术员离心样本后做成直接涂片,液基单层,离心式液基,做细胞块 for all samples。我不知道具体怎么处理的。但是他们用的是常规的方法。 这些技术指导类的东西可以在实验指导类书或网上找到。
如果确定是癌(当然,最好是经过免疫组化确定的),那么可以根据细胞学特征、临床信息等做出诊断或者要求做某些免疫组化指标以排除或者确定诊断。

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
-
本帖最后由 于 2009-08-06 04:04:00 编辑
| 以下是引用sos991229在2009-8-6 1:45:00的发言: 我们现在做CK7,CK20.Villin。就可以找到大致的来源。不防试试。赵老师,我觉得是癌,首选乳腺或者肺部。 |
Good consideration. Thanks.
If you are sure it is carcinoma (it is better with IHC confirmation) you need to have your ddx based on the cytomorphologic features, clinical informtion and decide what IHC stains you will use to rule in or rule out the dx.
-
本帖最后由 于 2009-08-06 10:39:00 编辑
| 以下是引用xiangyao在2009-8-6 0:59:00的发言: 请教赵老师,这个病例如果不做免疫组化标记,真的不敢定是恶性的吗?间皮细胞增生到这种程度也恐怕是瘤性的了!还有您们的细胞蜡块做的很好啊,不知道是用什么方法做的?希望能得到您的指导! |
As I mentioned before most of the time you may be right, but you will be wrong some times.
For body cavity fluid cytotech will centrifuge the fluid and make the direct smears, ThinPrep slide, cytospin slide, and cell block always. I do not know exactly how they make in the lab.However they just use the routine or usual methods. You should easily find these methods in some lab tech books or internet
-
本帖最后由 于 2009-08-07 11:58:00 编辑
Occasionally saw many body fluid cases with discussion here. I think some people may be nor aware of the principle for dx of body fluid.
1.Most common body cavity fluid in clinic includes pleural effusion and ascites (peritoneal fluid). The mesaothelium is a single layer of flat cells. However, Many reactive conditions can lead to mesothelial cell proliferation, thus binuleaton and multinucleation, increased mitotic figures, nuclear enlargement, increased N/C ratio, coarse chromatin, prominant nucleoli, markedcytological atypia. All these features can mimic neoplastic conditions, and may be misinterpreted as malignancy, especially, adenocarcinoma.
2. When we see a case with atypical glandular-like cells we must rule out if these cells are reactive mesothelial cells. This is very important. If they are mesothelial cells, they are benign reactive cells (of cause rare mesothelioma can be present. If they are epithelial cells they may be metastatic carcinoma cells (except endosalpingiosis in pelvic wash).
3. Remember that some reactive mesothelial cells can look very ugly and some adenocarcinoma cells can look benign.
4. Even though cytomorphology, history, clinical presentation are very important, the IHC stains are very important for some cases, especially for the cases without history. If you make dx only based on cytomorphologic features, you can be right (if you are a good cytopathologist) in most of times. However you will be wrong some times during your pathologist career.
5. Often it is a primary malignant dx in body fluid cytolgy. So we as pathologists have to be very cautious about our dx.
6. There are many markers to distinguish mesothelial cells from epithelial cells.
Epithelial cells: BerEp4, MOC 31, B72.3, CEA et al
Mesothelial cells (reactive or malignant): Calretinin, ck5/6, WT1 et al.
AE1/AE3, CK7, and EMA are postive in mesothelial cells. They are useless for this differentiation.
Many cytopathologists like to use two epithelial markers and two mesothelial markers for the difficult cases because occasionally some markers can have different expression. Some cases of mesothelial cells may ne positive for MOC31, some epithelial cells may be negative for berEp4 or B72.4. Of cause you always make your judgment based on the individual case.
7. If we rule out the mestothelial origin we can consider the possible primary of the malignancy based on cytology, clinical and imaging information, and more IHC stains.
8. The most common cause of a malignant pleural effusion in men is lung carcinoma, and in women it is breast ca. A malignant peritoneal effusion is most commonly caused by a gastrointestinal malignancy in men and by ovrian carcinoma in women.