| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
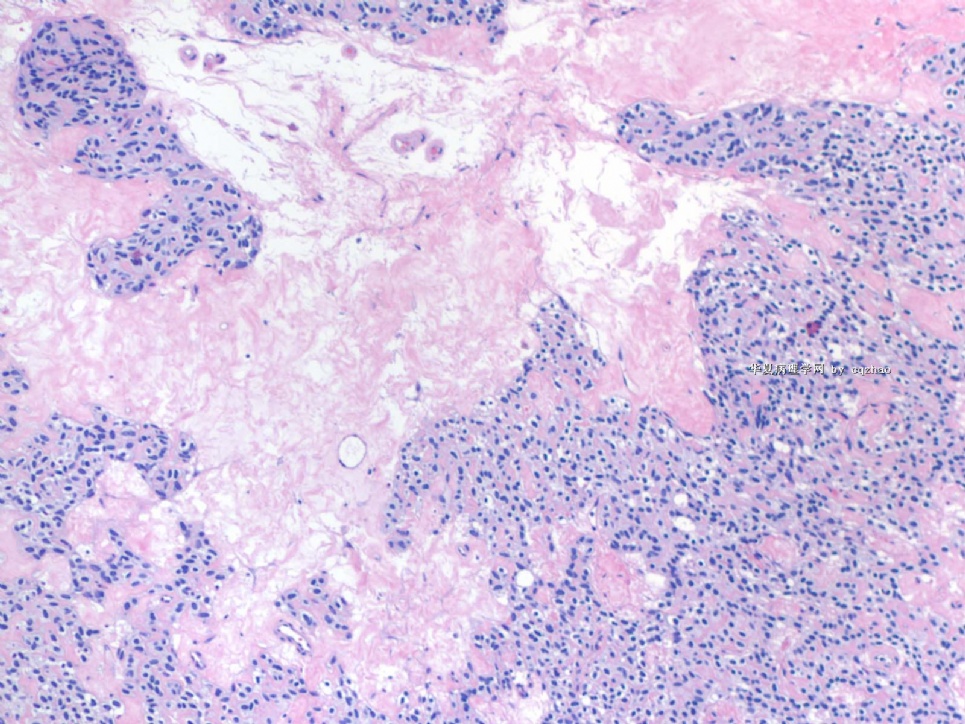
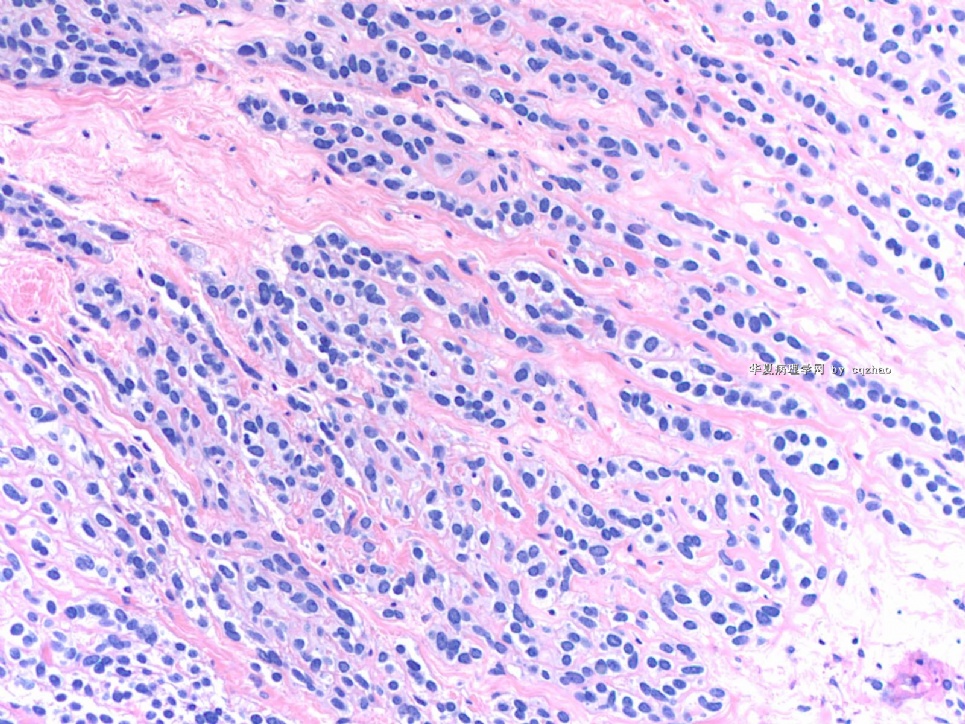
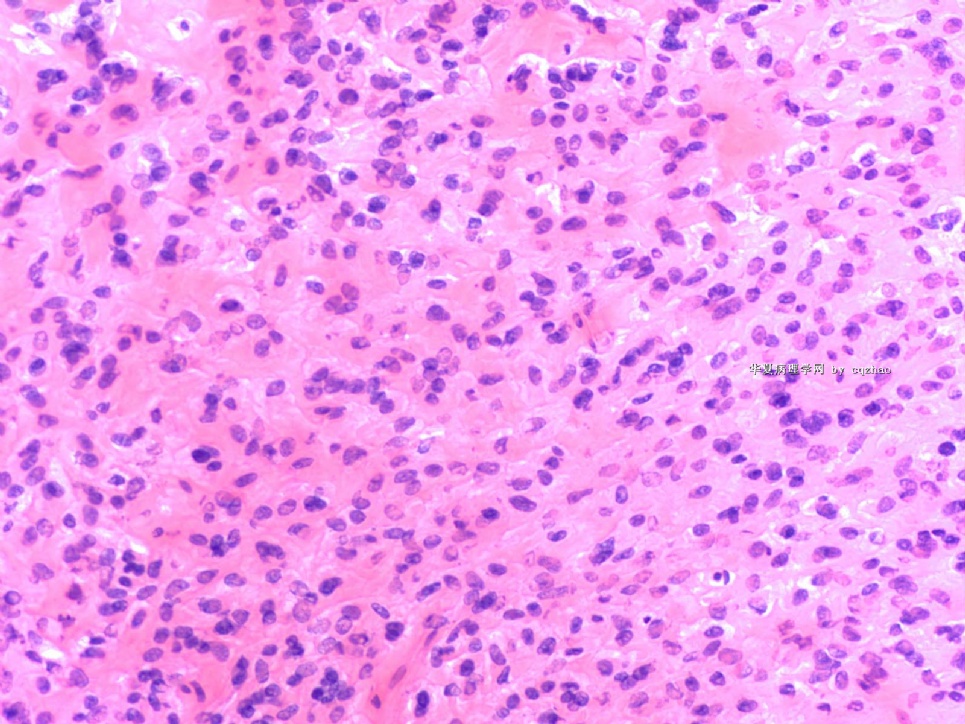
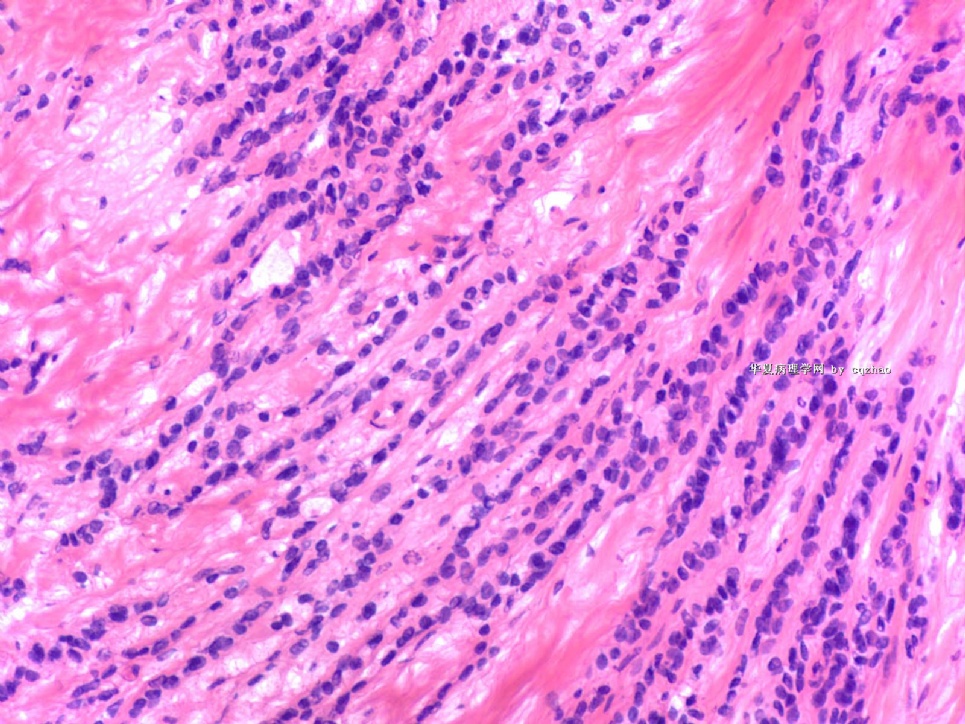
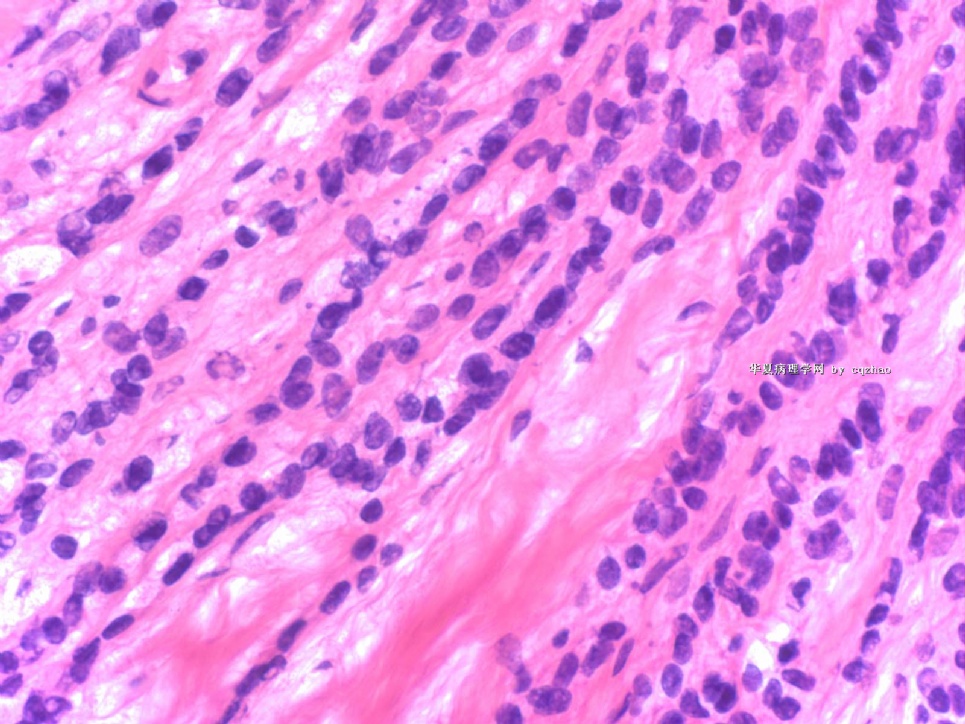
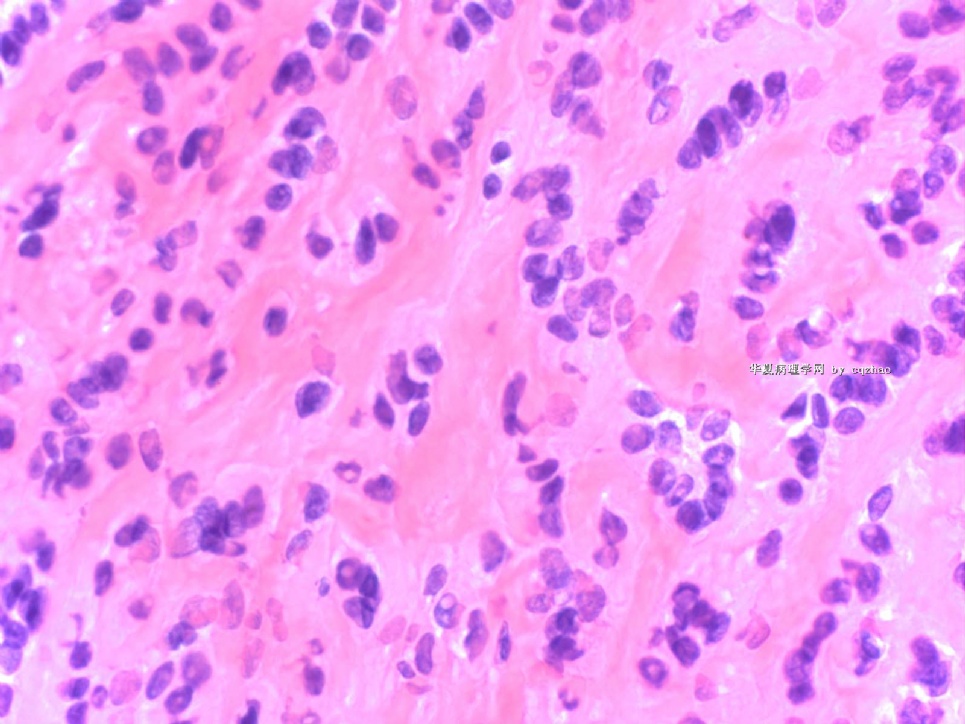
- B1590Interpretation: Ovarian stromal tumor with features of sclerosing stromal tumor and thecoma
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
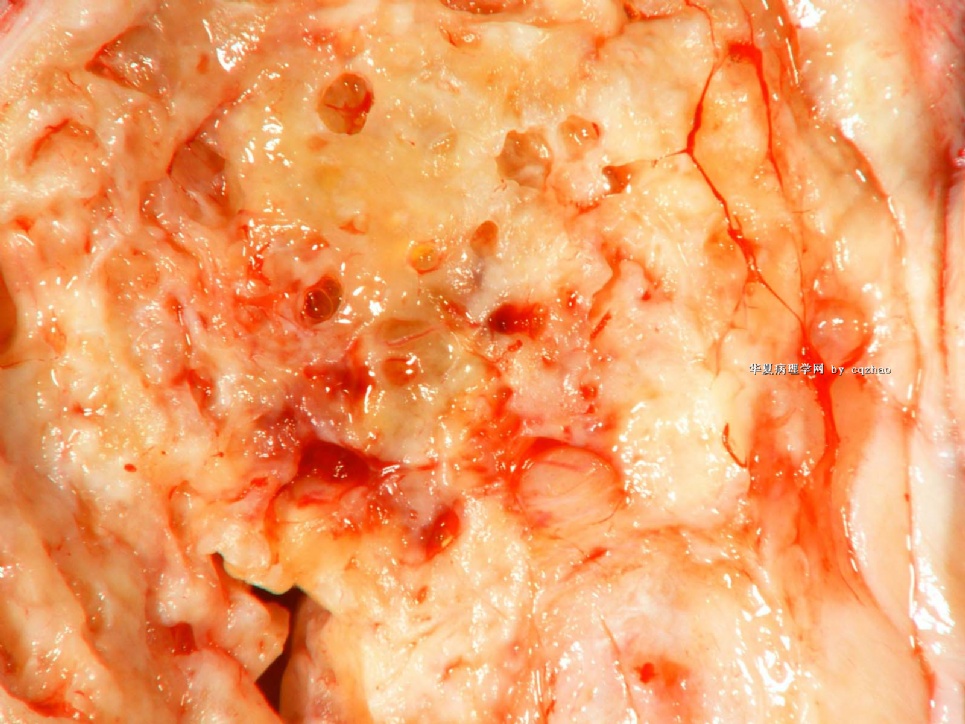
| 肉眼检查: | |||||
40-45 y/f with hx of cervical ca with radiation, chemotherapy, ovarian mass 11 cm. I did frozen. Gynecologist came to frozen room to sit with me to read frozen slide.
What can you tell your surgen about the case if your were the pathologist?
What is your differential dx?
I ordered IHC in frozen block and will know basic result tomorrow.
abin译:
20分钟前的卵巢肿瘤冰冻切片。我们能告诉妇科医生什么?
40-45岁女性,有宫颈癌病史和化疗、放疗史。卵巢肿块11cm。我做冰冻切片,妇科医生跑到冰冻室,和我坐在一起看冰冻切片。本例,如果你是病理医生,你能告诉手术医生什么?
你的鉴别诊断是什么?
我用冰冻切片做了免疫组化,明天会知道基本结果。
-
本帖最后由 于 2009-07-24 08:08:00 编辑
相关帖子
-
本帖最后由 zhihualan 于 2012-06-20 23:52:24 编辑
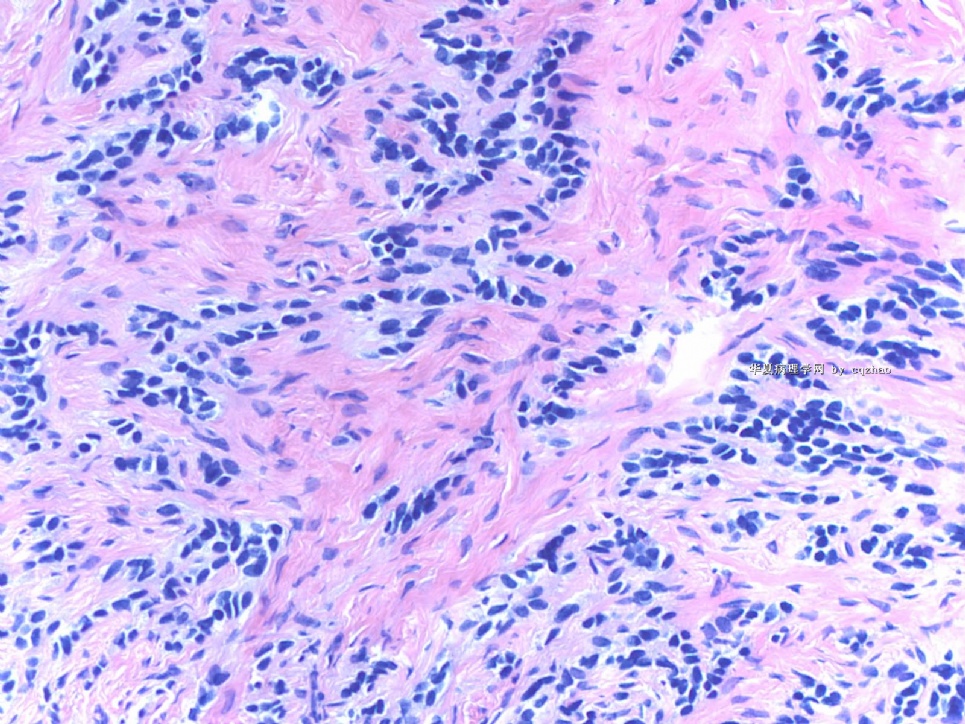
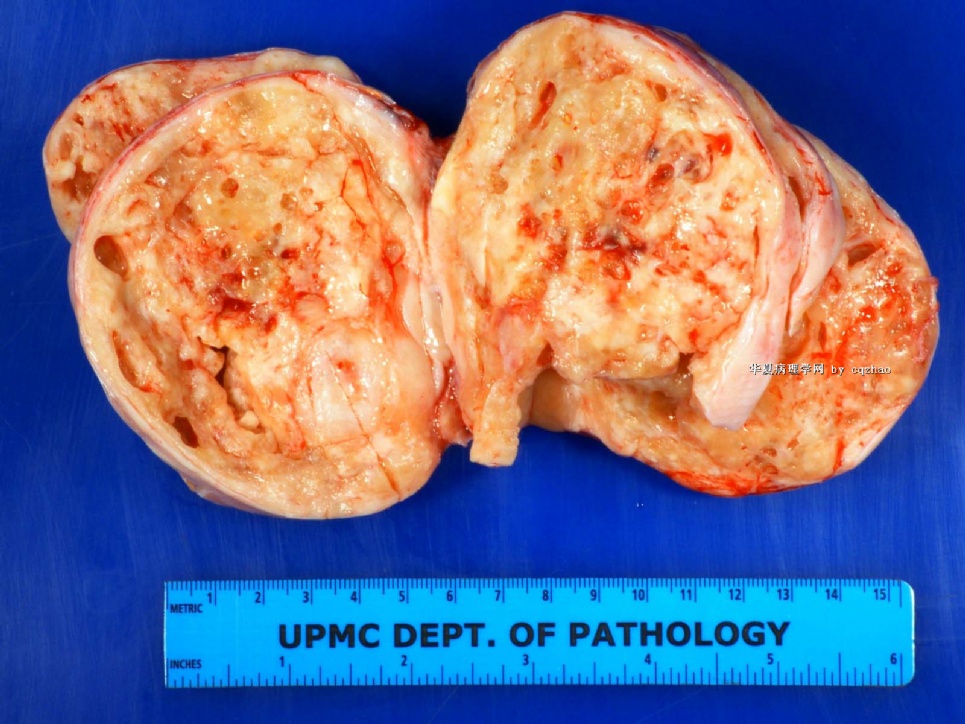
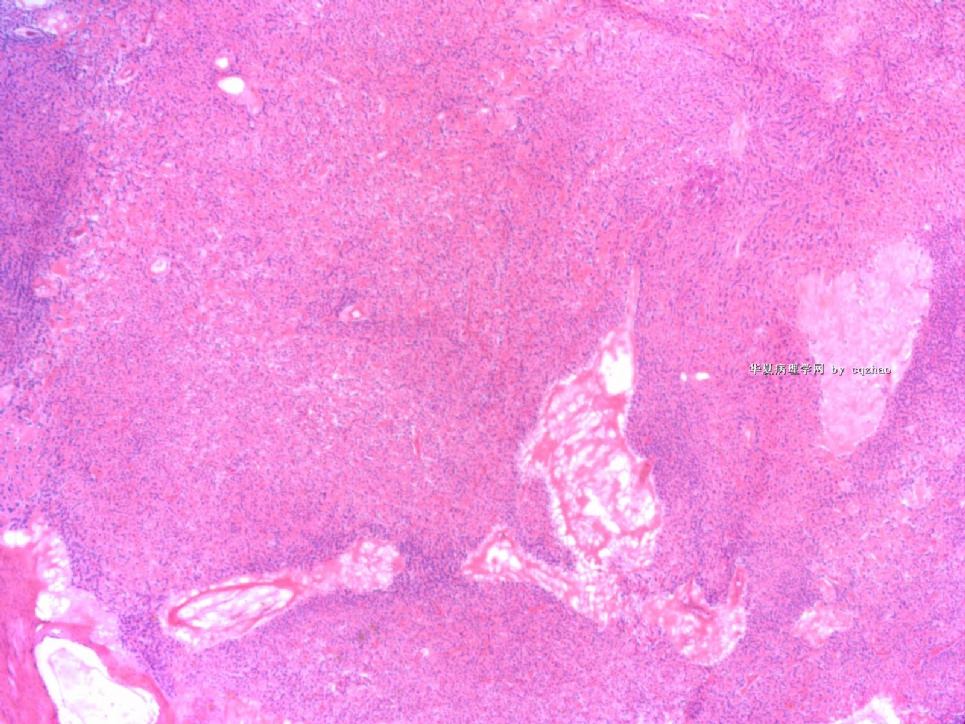
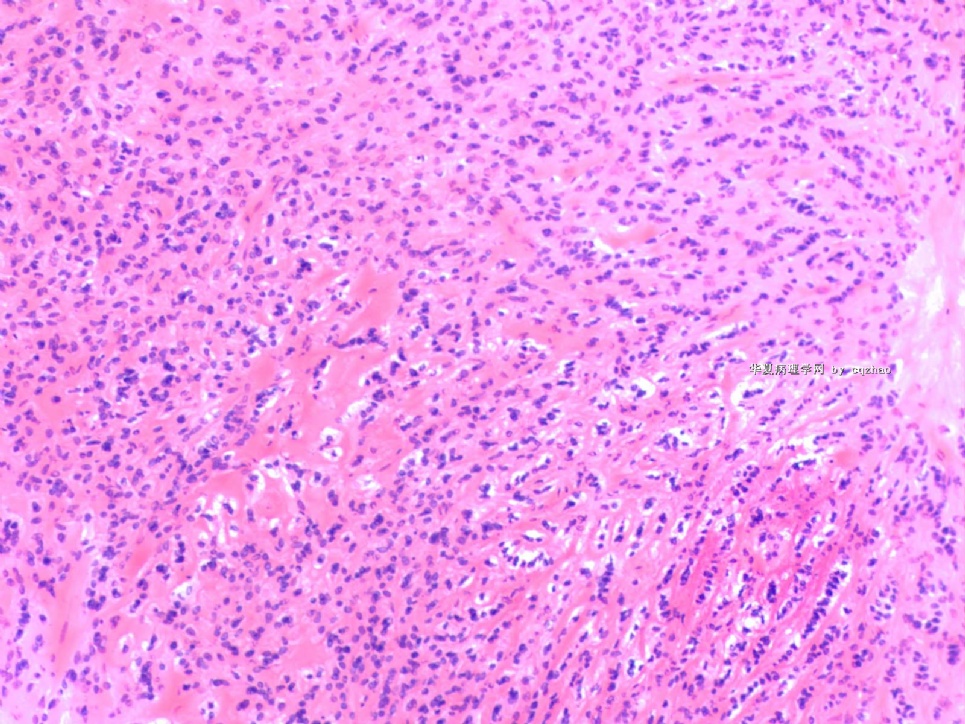
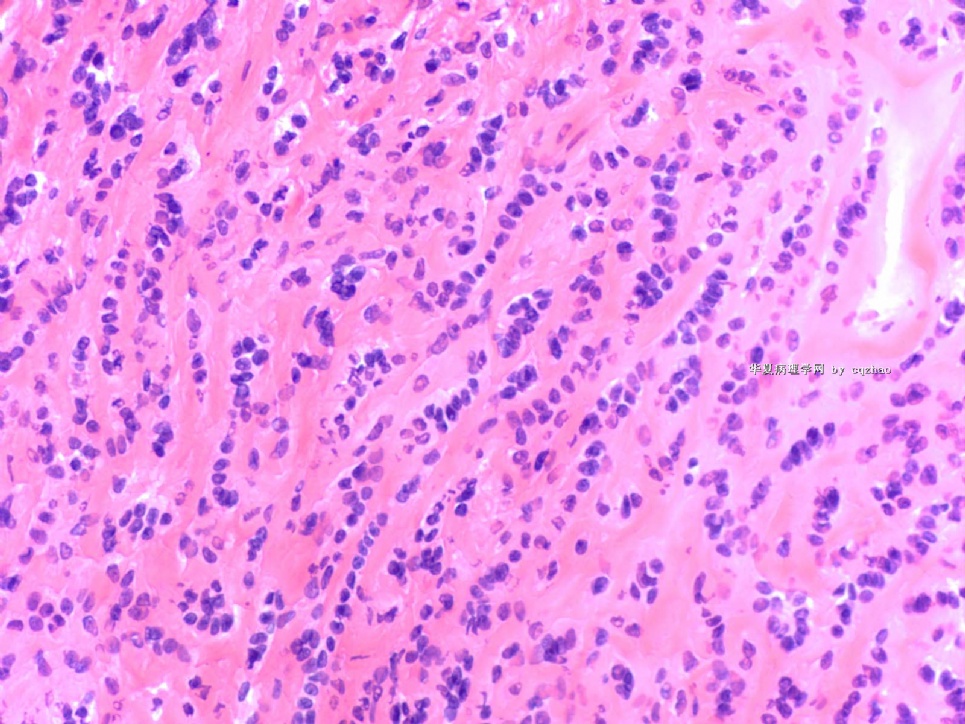
对于这一例,大体下有淡黄色的切面,这让我首先想到了性索-间质的肿瘤。镜下我看到的列兵样排列,我个人认为是性索样的分化的感觉,如果去掉广泛的纤维胶原区,那么性索样的分化更为明显,类似于颗粒细胞瘤的缎带,波纹型。颗粒细胞瘤是低度恶性的,即使是幼年型的颗粒细胞瘤也有10%是低度恶性的,当然这一例显然不是幼年型的颗粒细胞瘤,而硬化性间质瘤与卵泡膜瘤是良性的,所以如何发报告,对病理医生是一个较大的挑战。只能依赖于免疫组化,问题是性索间质之内的3个肿瘤可以靠免疫来区分吗?呵呵。对于术中快速,只能与临床有良好的沟通,以帮助临床做出手术选择,又不必给自己带来过大的压力。这些是个人的浅见,请各位老师批评指正。还是看不懂,呵呵

- 我思故我在
-
本帖最后由 于 2009-04-17 12:13:00 编辑
很羡慕Dr.zhao和临床医生之间融洽的合作关系。
大体和镜下图像都是恶性肿瘤,它的起源和组织学类型颇费思量。
1 转移性
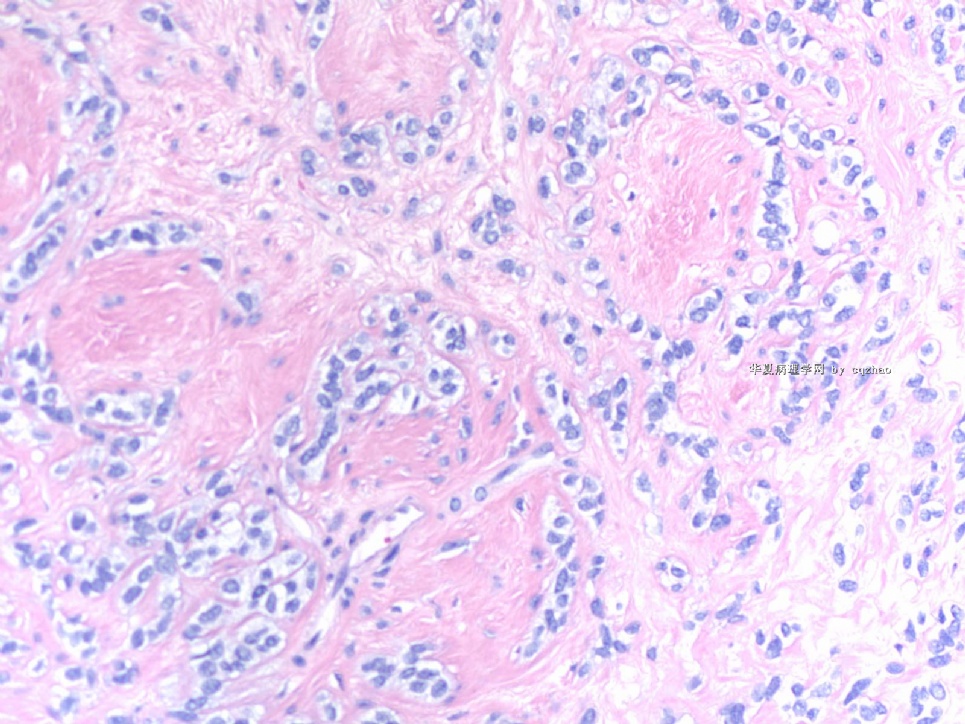
由于有宫颈癌病史,首先想到宫颈癌转移。卵巢肿瘤是否双侧性?宫颈癌的原诊断,是腺癌还是鳞癌?冰冻切片时间紧迫,几乎不可能调阅原切片,知道原诊断的组织学类型也有帮助。冰冻切片的图像少见,似癌但又不太像,是否因放化疗影响导致的形态学改变?
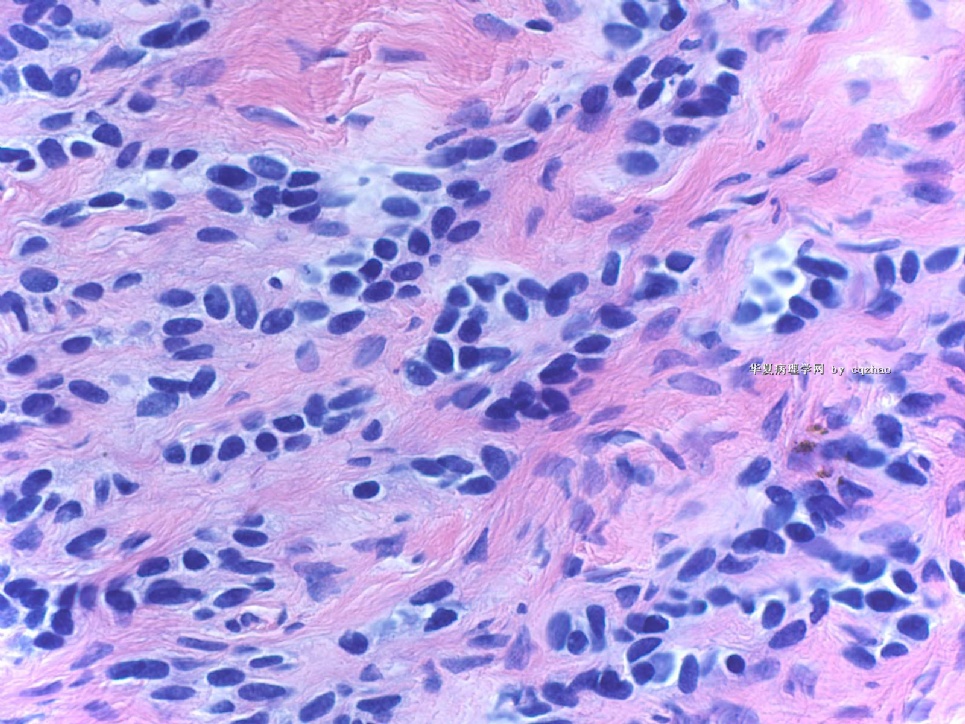
其它部位的转移性恶性肿瘤?单行排列和印戒细胞,怀疑转移性乳腺浸润性小叶癌。消化道也要探查。还有恶黑、子宫内膜间质肉瘤、促结缔组织增生性小圆细胞肿瘤、淋巴瘤和白血病也要考虑。
2 原发性
然后是卵巢原发的恶性肿瘤。小细胞恶性肿瘤,有透明胞浆和核内假包含体(也可能是冰冻假象),片状小巢状和条索状排列,有大片坏死和间质胶原化。鉴别诊断包括:低分化腺癌、小细胞癌(肺型和高血钙型)、PNET、性索间质肿瘤、。
如果是我,会告诉临床:是恶性肿瘤,但来源和组织学类型暂时无法确定,等常规切片和免疫组化。它可能是原发的也可能是转移的,需要探查多个部位。

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
-
stevenshen 离线
- 帖子:343
- 粉蓝豆:2
- 经验:343
- 注册时间:2008-06-03
- 加关注 | 发消息
- I agree with Abin's detailed and careful observation and consideration. I am impressed with the nested nature and intracytoplasmic mucin like material and signet ring cells. Although I would consider other possibilties, I would tell the surgeon: carcinoma with signet ring like cells, favor metastatic (breast, GI, consider cervix first if the primary cervial cancer is adenocarcinoma).
- I am surprised that you will and can do the immunostain on frozen tissue.
- What I probably will do is to wait until we have a chance to review the morphology on permanent paraffin sections to see whether there is better differentiated areas.
- Would you consider move this case to Frozen Section...
Hi Dr. Zhao, it was great to see you at the USCAP meeting and I wish I could have more time to talk to you. I am sure that we will see each other many more times in the future. I would join in the discussion and look forward to hearin from you and others how to deal with this case. Thanks!
-
本帖最后由 于 2009-04-18 11:06:00 编辑
Dr. Shen, glad to meet you too in Boston. Thank your input for this case.
Agree with your and abin's interpretation. It is a tumor, mostly malignant, either primary or metastatic.
-Definetely it is not like classic ovarian epithelial carcinoma (serous, endometrioid, ccc, or mucinous).
-Other ovarian tumors include sex cord stroma tumor, neuroendocine tumor (carcinoid), or small blue cell tumors. If it is ovarian primary, I favor granulosa tumor.
-Metastatic tumors: morphology looks like breast lobular ca. Cytomorphologic features do not like colonic or upper GI tumors.
-Later I checked the history and noticed that pt had CIN3. So surgens' information are often not accurate.
-Thinking about the clinical pictures: mid age women had not carcinoma history, large ov mass 11 cm without normal ovarian tissue. I favor a ov primary tumor.
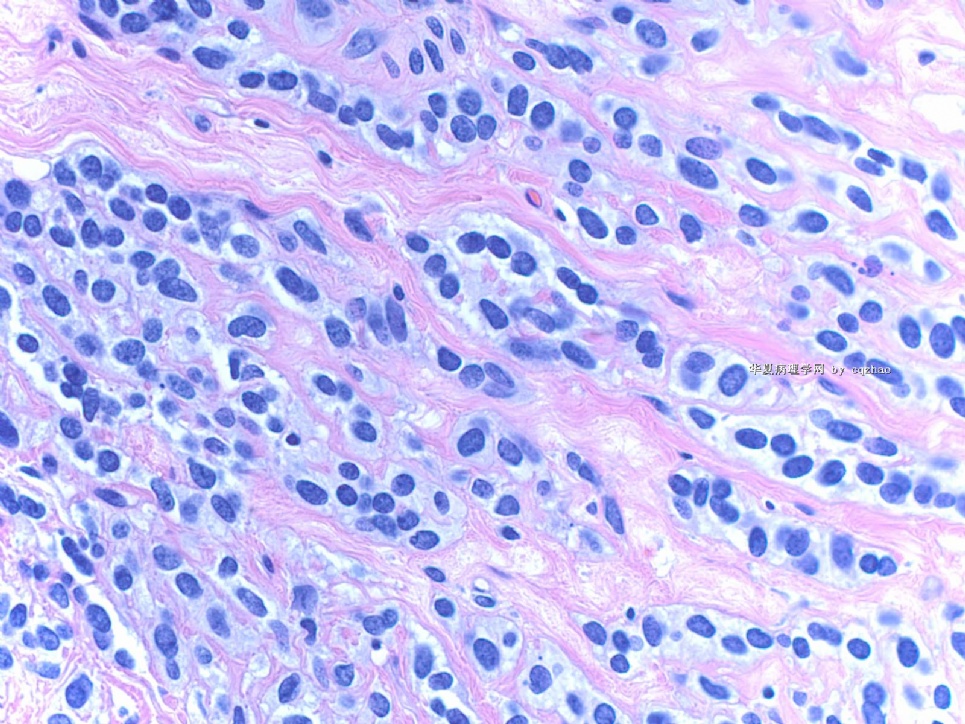
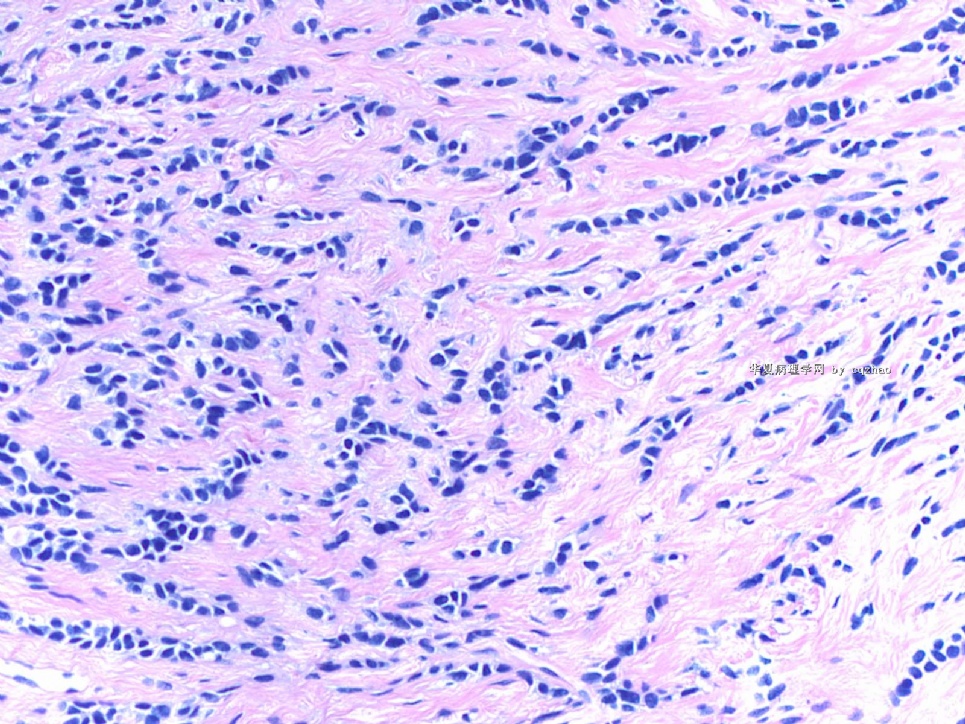
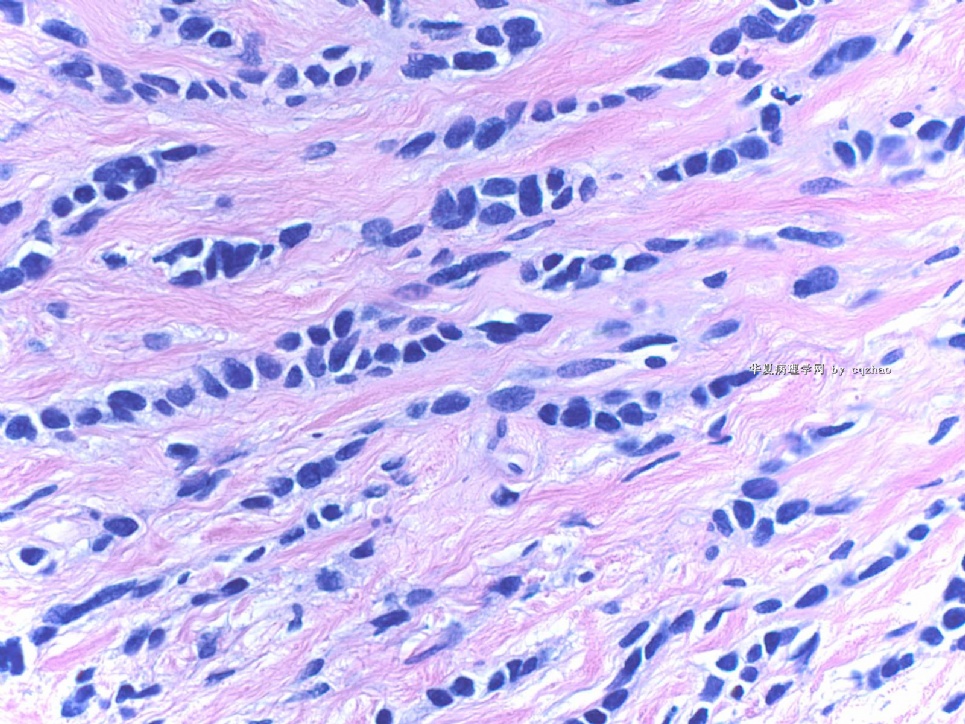
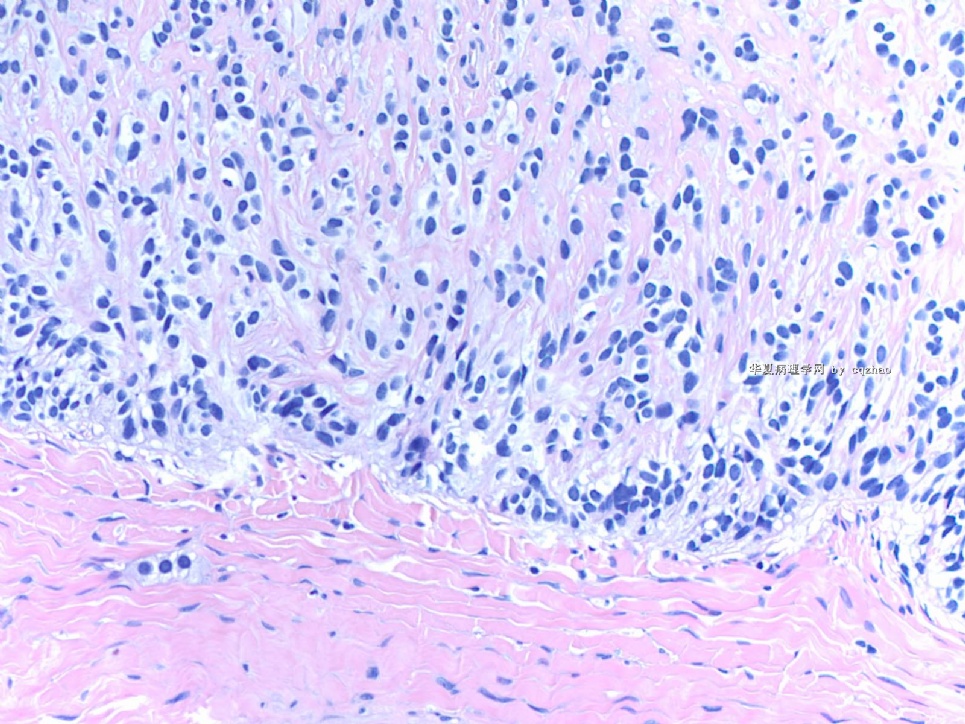
-Granulosa cell tumor (GCT) includes many growth patterns: microfollicular, macrofollicular, insular, diffuse, trabecular, watered-silk (moire-silk), gyriform, cystic, luteinized et al. This tumor shows uniform small round cells with diffuse, and single cell file growth patterns, really like breast lobular ca. However you see the first photos above, you can see tumor nests srrounding with dense stroma. About the focal signet ring cells, I favor frozen artifact. Also we can appreciate some microfollicular structures in the last photo.
-Anyway based on the clinical, gross, and microscopic features, I will choose granular cell tumor if I must pick one answer in a test.
-I told gyncologist what I mentioned above. The only issue is that the patient might not need to stage if I am sure it is a metastatic tumor. I am not sure of that. Gynecologist agree and understood. He did lymph node stage for this patient.
-In our frozen interpretation, we must write one diagnosis from three choices: malignant, benign, defer. Then we can write more detailed interpretation.
So my frozen report for this case: A) Malignant B) primary ov tumors favor granulosa tumor; metastatic tumors, breast et al. All the frozen report will be checked and compared with perminant diagnosis, as quality control. QA only cares first line dx, maligant, benign, defer. You cannot have too many defer reports.
Dr. Shen is right that we should wait for the perminant H@E slides and then choose a good block and make decision to do IHC. For this case I am very curious to know what it is. This is why I ordered the IHC yesterday and I can have the result today. Our large slides will be out 10-12 o'clock. I order IHC today I will not know the resut until Monday. IHC can be done in frozen block. In fact I asked the PA to choose another section for IHC. All mass is tumor for this case. Even though I do not see the H@E. It should be good enough for IHC.
I have not my H@E slides of today's cases yet. So I have time to read more for the reference of our chinses young pathologists. I should have IHC result today at four o'clock and will paste the result next week. Of cause all my analyses can be totally wrong.
cz
-
本帖最后由 于 2009-04-19 18:36:00 编辑
- I agree with Abin's detailed and careful observation and consideration. I am impressed with the nested nature and intracytoplasmic mucin like material and signet ring cells. Although I would consider other possibilties, I would tell the surgeon: carcinoma with signet ring like cells, favor metastatic (breast, GI, consider cervix first if the primary cervial cancer is adenocarcinoma).
- I am surprised that you will and can do the immunostain on frozen tissue.
- What I probably will do is to wait until we have a chance to review the morphology on permanent paraffin sections to see whether there is better differentiated areas.
- Would you consider move this case to Frozen Section...
| 以下是引用stevenshen在2009-4-17 7:01:00的发言:
Hi Dr. Zhao, it was great to see you at the USCAP meeting and I wish I could have more time to talk to you. I am sure that we will see each other many more times in the future. I would join in the discussion and look forward to hearin from you and others how to deal with this case. Thanks!
|
译文:赵博士,很高兴在USCAP年会上见到你,很想有更多的时间和你交流。我相信将来这种机会会越来越多。我加入这个讨论,期望听听你和其他人的意见以及对这个病例的处理。谢谢。
我同意abin详细和认真的观察和分析,镜下肿瘤细胞排列成巢状,胞质内有粘液样空泡,像印戒细胞。尽管我也考虑到其他疾病的可能,但我会告诉手术医生,肿瘤是伴有印戒样细胞特征的癌,支持转移性的(乳腺、胃肠道,如果宫颈原发癌是腺癌,首先考虑为宫颈转移)。
我对你们能在冰冻切片中做免疫标记感到好奇
我可能要做的是等到石蜡切片出来看是否有分化较好的区域。
你是否愿意将这一病例移到“冰冻切片”专栏?
-
本帖最后由 于 2009-04-30 19:44:00 编辑
| 以下是引用cqzhao在2009-4-17 21:38:00的发言:
Dr. Shen, glad to meet you too in Boston. Thank your input for this case. Agree with your and abin's interpretation. It is a tumor, mostly malignant, either primary or metastatic. -Definetely it is not like classic ovarian epithelial carcinoma (serous, endometrioid, ccc, or mucinous). -Other ovarian tumors include sex cord stroma tumor, neuroendocine tumor (carcinoid), or small blue cell tumors. If it is ovarian primary, I favor granulosa tumor. -Metastatic tumors: morphology looks like breast lobular ca. Cytomorphologic features do not like colonic or upper GI tumors. -Later I checked the history and noticed that pt had CIN3. So surgens' information are often not accurate. -Thinking about the clinical pictures: mid age women had not carcinoma history, large ov mass 11 cm without normal ovarian tissue. I favor a ov primary tumor. -Granulosa cell tumor (GCT) includes many growth patterns: microfollicular, macrofollicular, insular, diffuse, trabecular, watered-silk (moire-silk), gyriform, cystic, luteinized et al. This tumor shows uniform small round cells with diffuse, and single cell file growth patterns, really like breast lobular ca. However you see the first photos above, you can see tumor nests srrounding with dense stroma. About the focal signet ring cells, I favor frozen artifact. Also we can appreciate some microfollicular structures in the last photo. -Anyway based on the clinical, gross, and microscopic features, I will choose granular cell tumor if I must pick one answer in a test. -I told gyncologist what I mentioned above. The only issue is that the patient might not need to stage if I am sure it is a metastatic tumor. I am not sure of that. Gynecologist agree and understood. He did lymph node stage for this patient. -In our frozen interpretation, we must write one diagnosis from three choices: malignant, benign, defer. Then we can write more detailed interpretation. So my frozen report for this case: A) Malignant B) primary ov tumors favor granulosa tumor; metastatic tumors, breast et al. All the frozen report will be checked and compared with perminant diagnosis, as quality control. QA only cares first line dx, maligant, benign, defer. You cannot have too many defer reports. Dr. Shen is right that we should wait for the perminant H@E slides and then choose a good block and make decision to do IHC. For this case I am very curious to know what it is. This is why I ordered the IHC yesterday and I can have the result today. Our large slides will be out 10-12 o'clock. I order IHC today I will not know the resut until Monday. IHC can be done in frozen block. In fact I asked the PA to choose another section for IHC. All mass is tumor for this case. Even though I do not see the H@E. It should be good enough for IHC. I have not my H@E slides of today's cases yet. So I have time to read more for the reference of our chinses young pathologists. I should have IHC result today at four o'clock and will paste the result next week. Of cause all my analyses can be totally wrong. cz |
Dr. Shen,非常高兴在波士顿见到你,谢谢你参与这个病例的讨论。
同意你和abin的分析。该例是一个肿瘤,基本是恶性的,原发或转移。
明确一些它不像经典的卵巢上皮性癌(浆液性、子宫内膜样、透明细胞癌或黏液性癌)
其他的卵巢肿瘤包括性索间质肿瘤、神经内分泌肿瘤(类癌)或小蓝细胞肿瘤。如果是原发的,我认为是粒层细胞瘤。
转移性肿瘤:形态学像乳腺小叶癌,细胞形态学特征不像结肠或上消化道肿瘤。
后来我看了病人的病史,发现病人有CIN3而不是癌,所以有时候医生的信息也不是准确的。
结合临床情况:中年女性,没有癌的病史,肿块大有11cm,未见正常卵巢组织,我认为是卵巢原发的。
粒层细胞肿瘤(GCT)有多种生长构型:微滤泡型、巨滤泡型、岛状、弥漫型、梁状型、波纹型、gyriform、囊性和黄素化等。本例肿瘤细胞小而圆,大小一致,弥漫和单个细胞排列,非常像乳腺小叶癌。然而,你看第一张图片,发现肿瘤呈巢状分布于致密的间质中。至于局灶性印戒细胞,我认为是冰冻假象。另外有一些微滤泡样结构在最后一图片。
无论如何,如果要在考试中必须选择一个答案的话,我会根据临床、大体和镜下形态选择粒层细胞肿瘤的诊断。
我告诉妇科医生我上面提到的情况。唯一的问题是如果我确信是一个转移性肿瘤,那么病人就不需要进一步staging处理。我无法确信是一个转移性肿瘤,妇科医生同意,也表示理解。他为这个病人进行了淋巴结切除。
在我们的冰冻切片诊断中,我们必须在恶性、良性和待常规等3种诊断中选择一种。然后我们才能详细说明。
这例我的冰冻报告是:A)恶性B)如为原发卵巢肿瘤考虑为粒层细胞肿瘤;若为转移性肿瘤则乳腺等。作为质量控制,所有冰冻报告都将与常规诊断比较。首先应保证一线诊断:恶性、良性和等待常规。你不能够有太多的延迟报告。
孙博士说的正确,我们应该等常规HE切片,然后选择好的蜡块做免疫标记。对于这例我非常好奇它是什么,这就是我为什么昨天就做了免疫标记,今天能知道结果。我们大切片在10-12点出来,今天做标记要到下周一才能知道结果。可以在冰冻组织中做免疫组化。实际上我要求住院医师选择另一个切片做。这个病例所有肿块都是肿瘤,不看切片,这组织快也应可以用于做免疫标记。
我还没有收到今天的病理HE切片,所以我有更多时间与中国的年轻病理医生进行交流。今天下午4点钟免疫组化结果应该出来,下周我将IHC结果贴上来。当然我的所有分析可能都是错误的。