| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
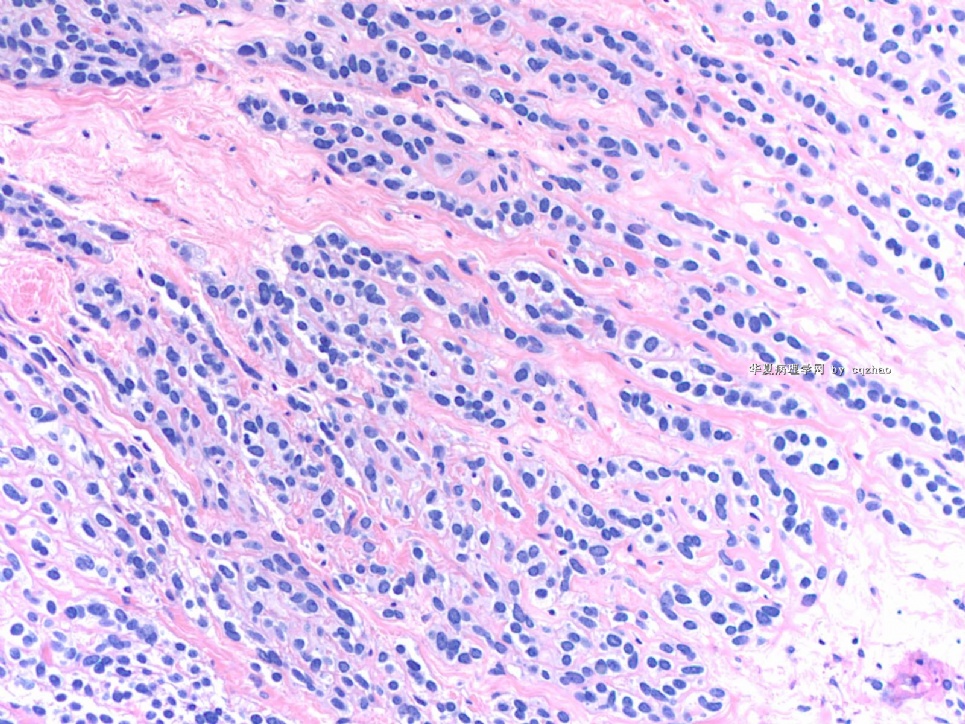
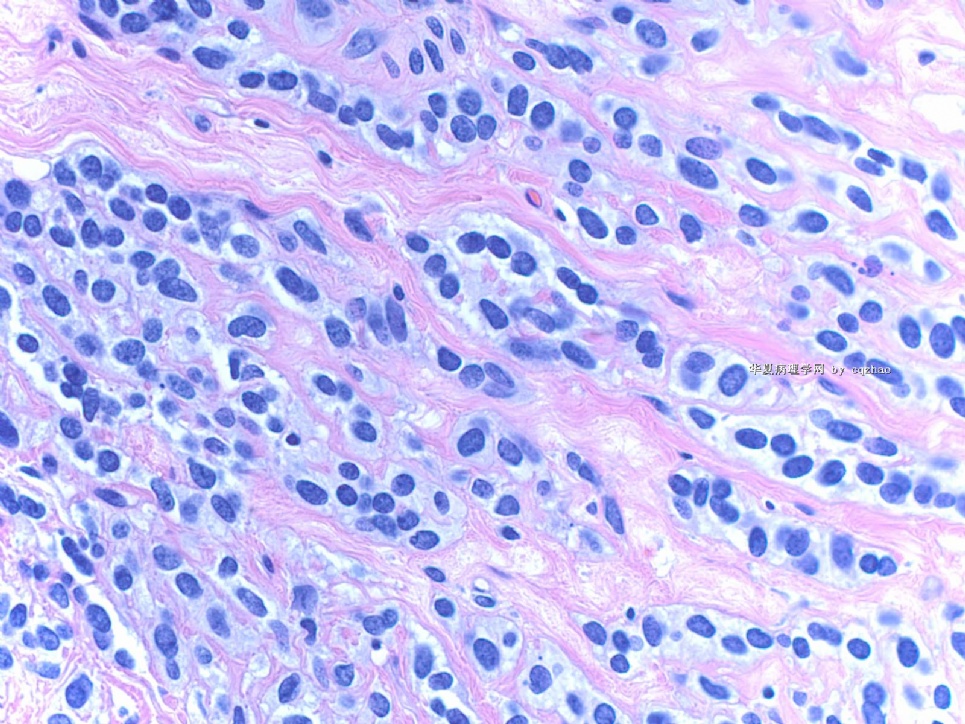
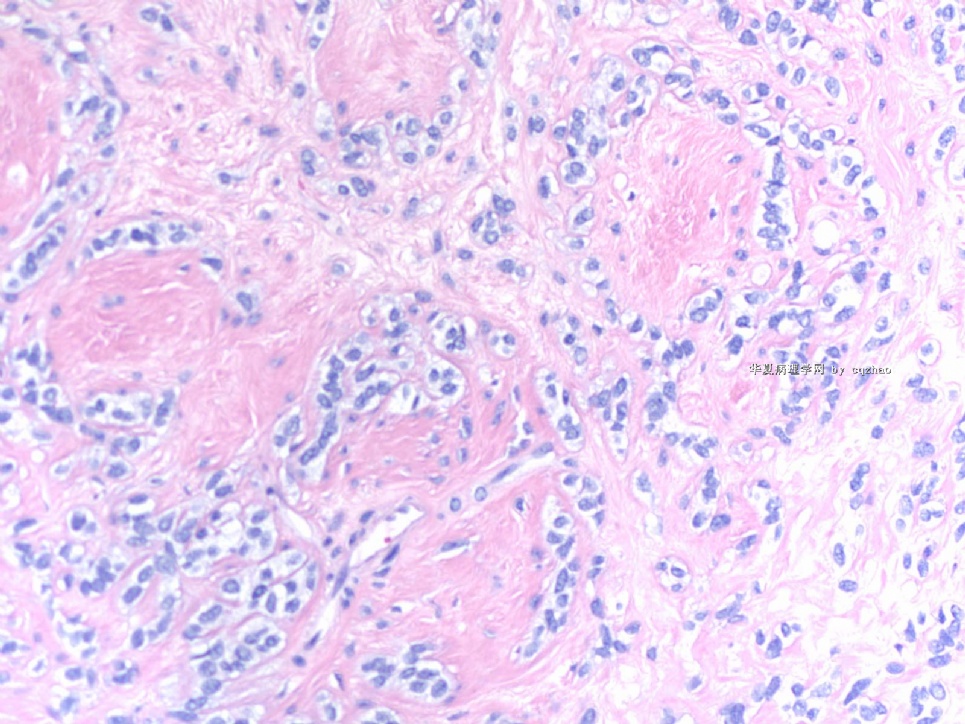
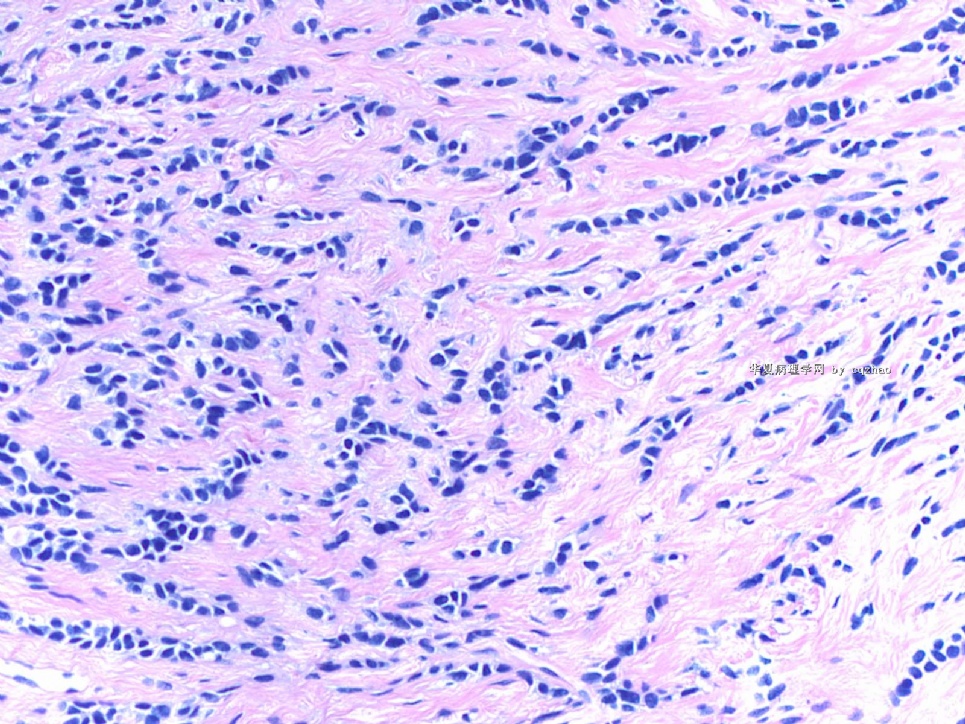
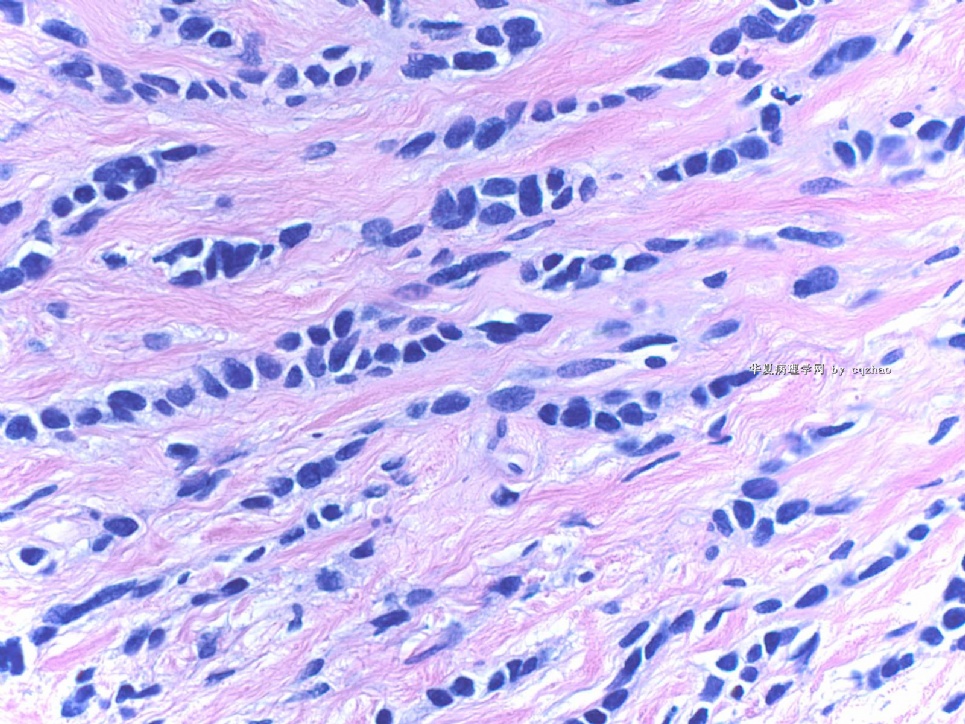
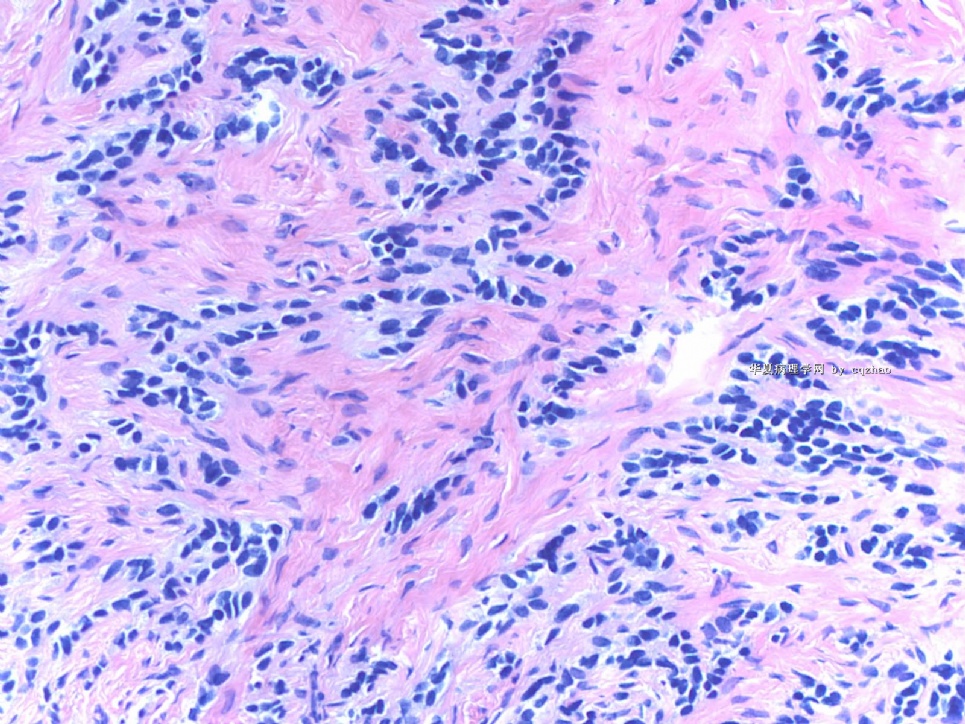
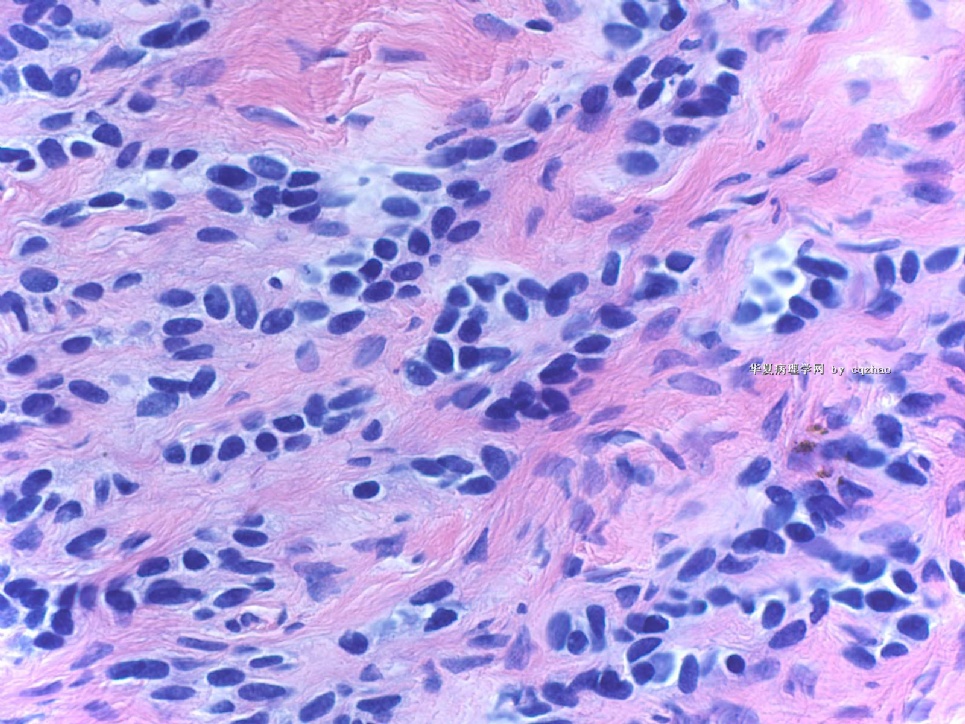
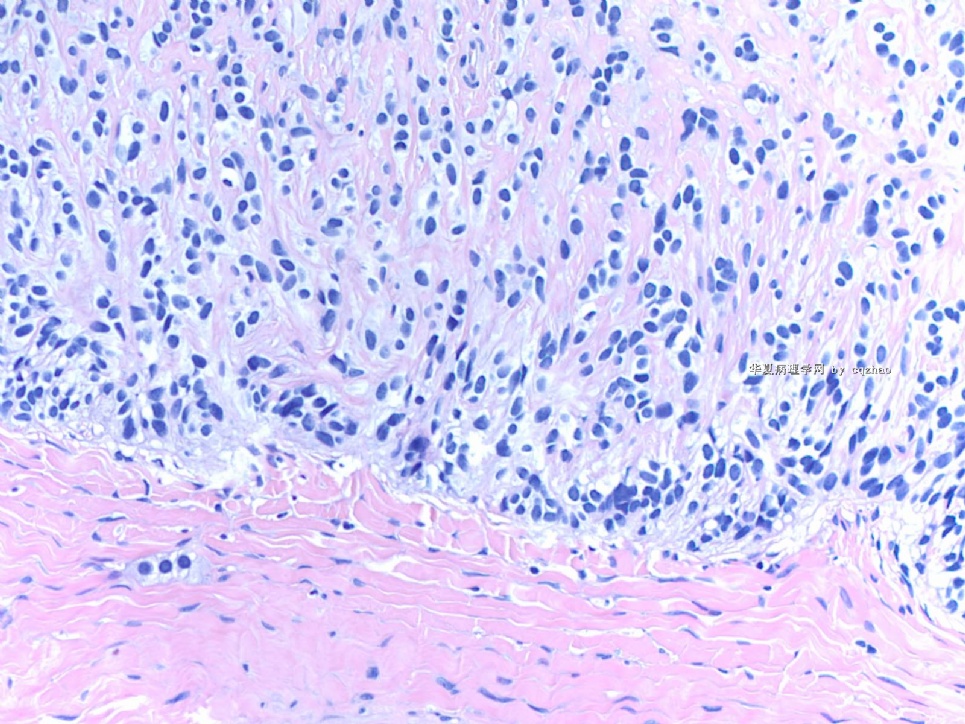
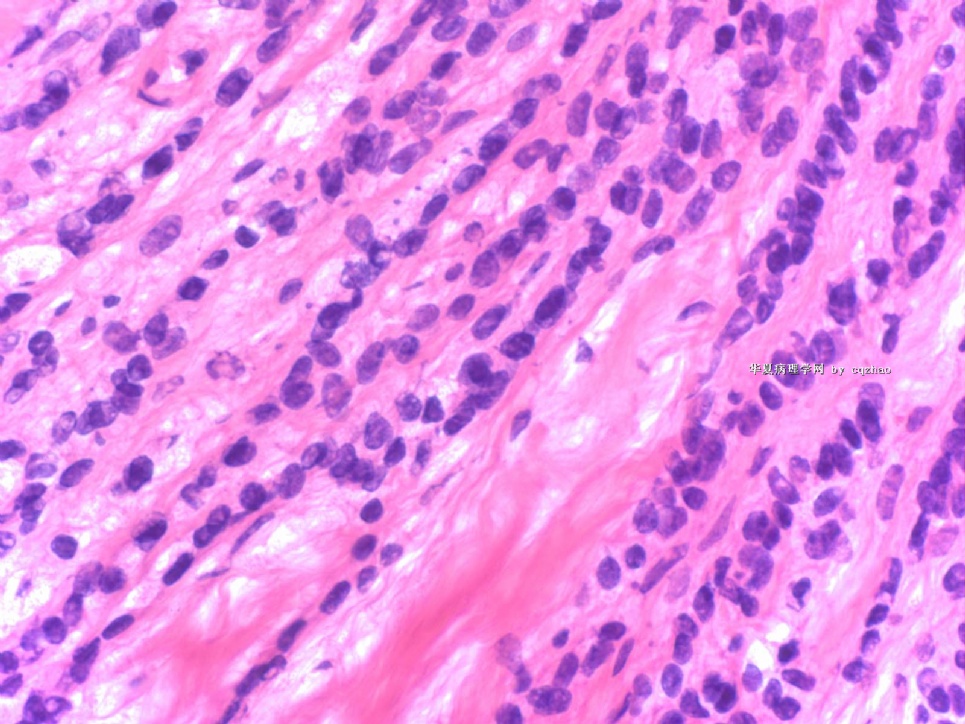
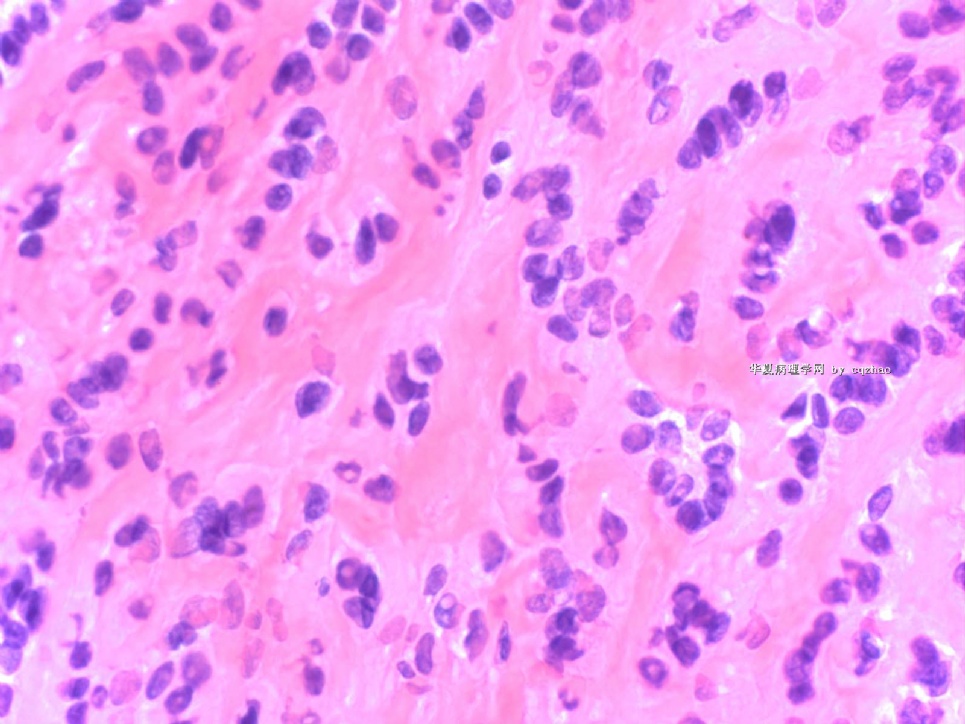
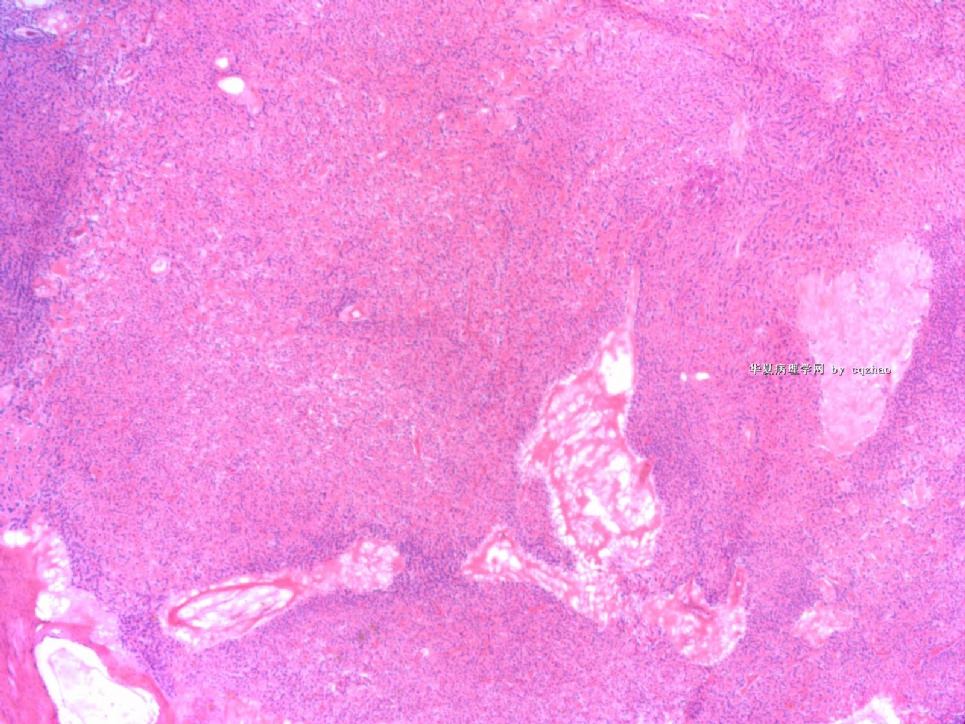
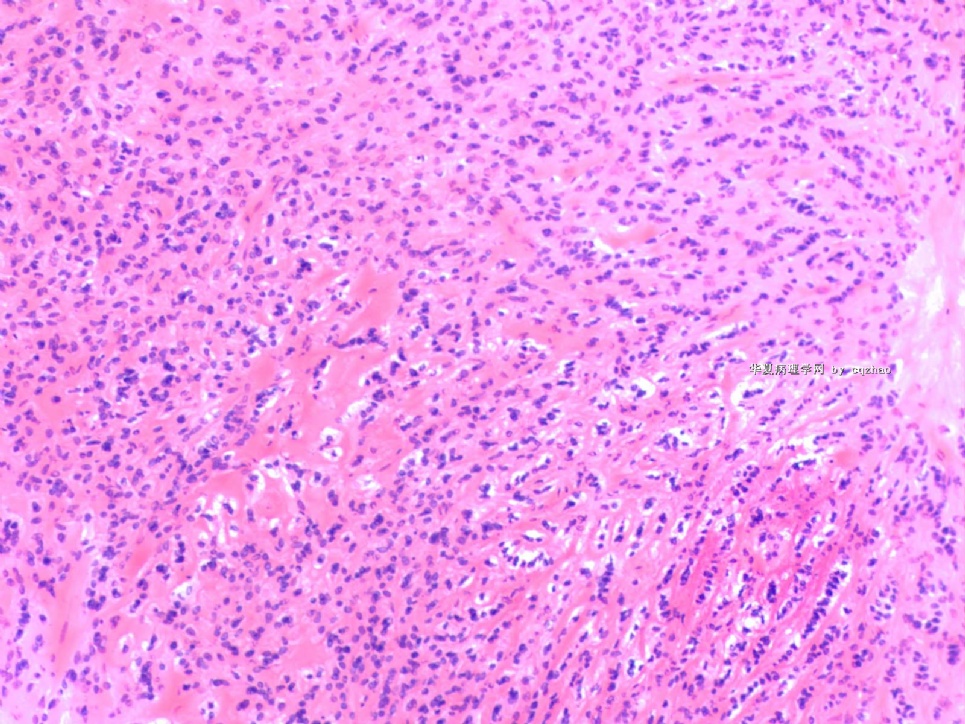
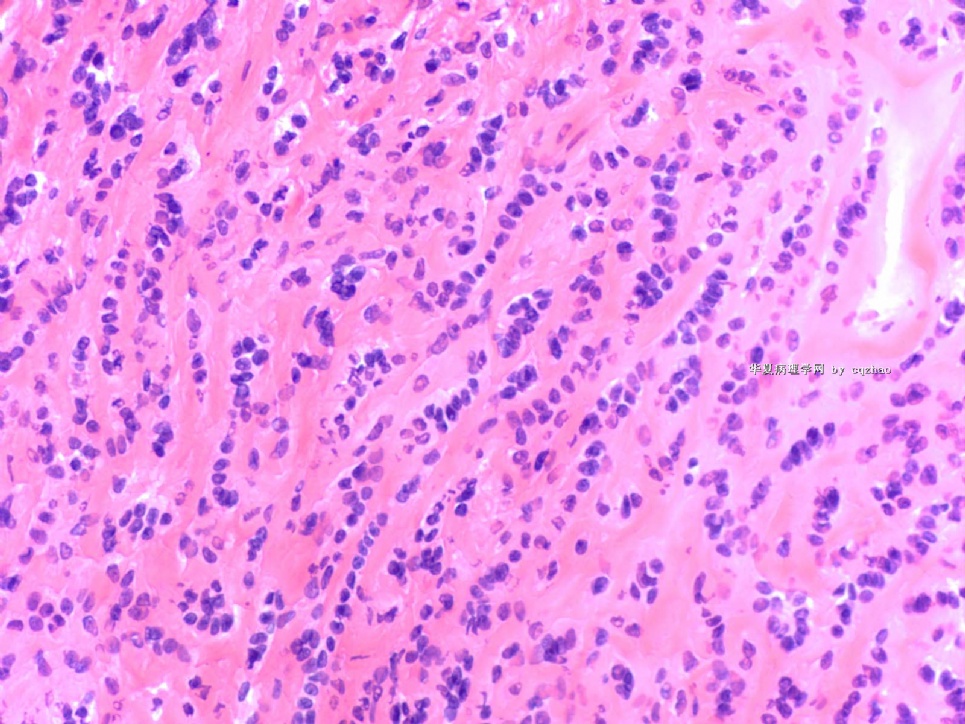
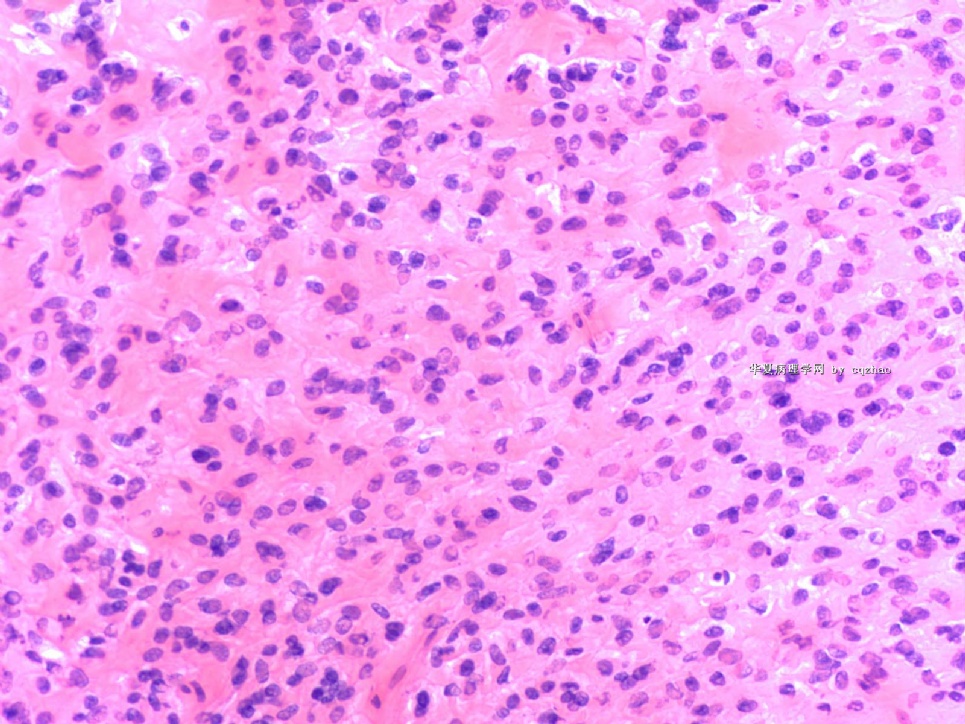
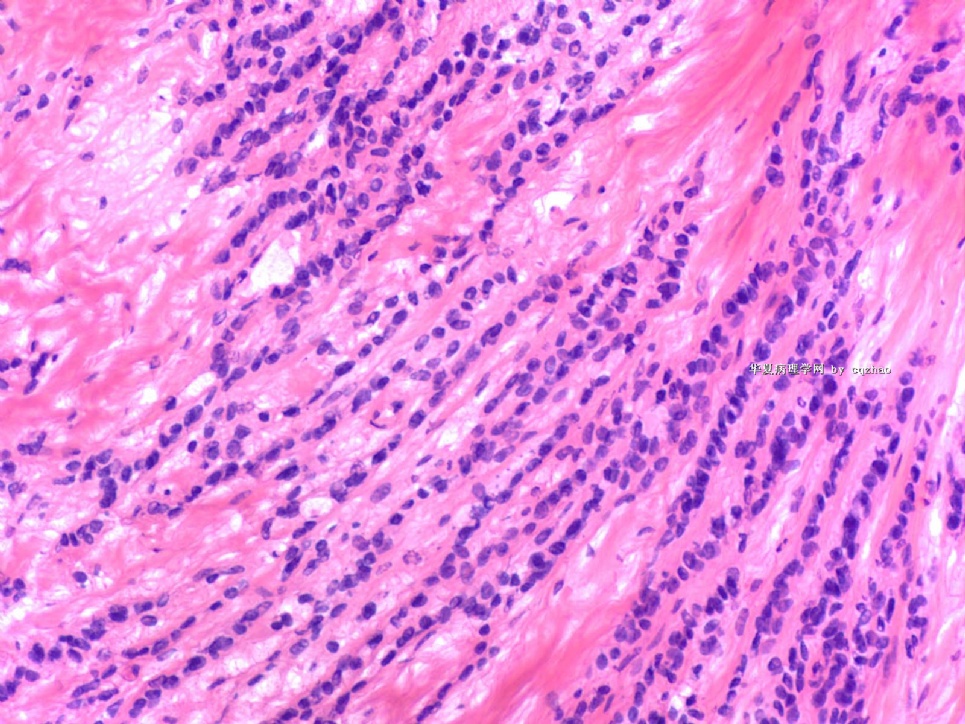
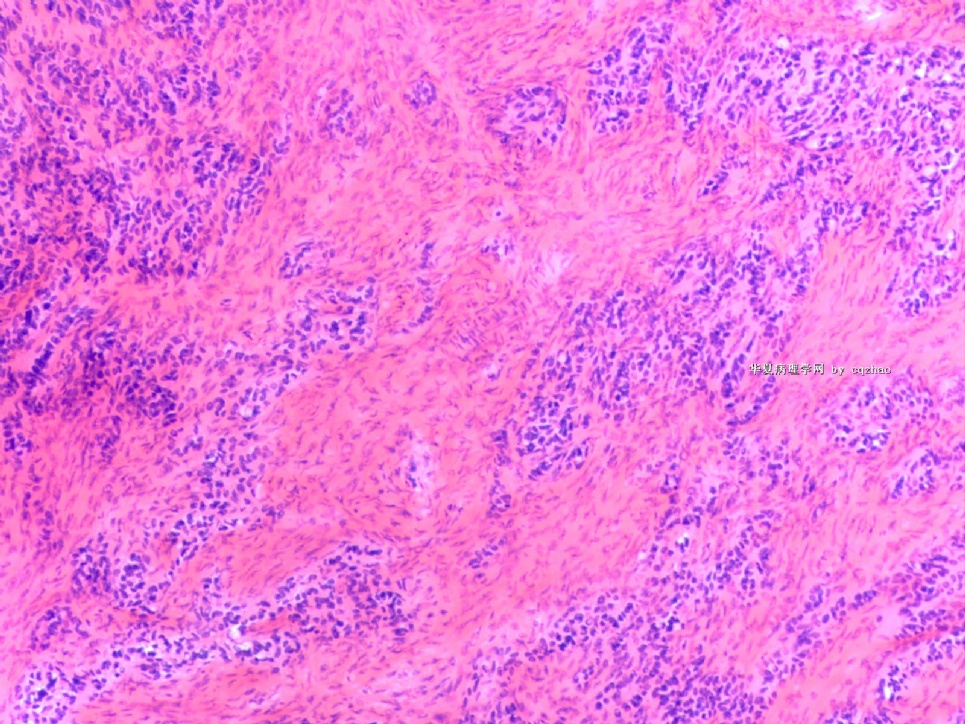
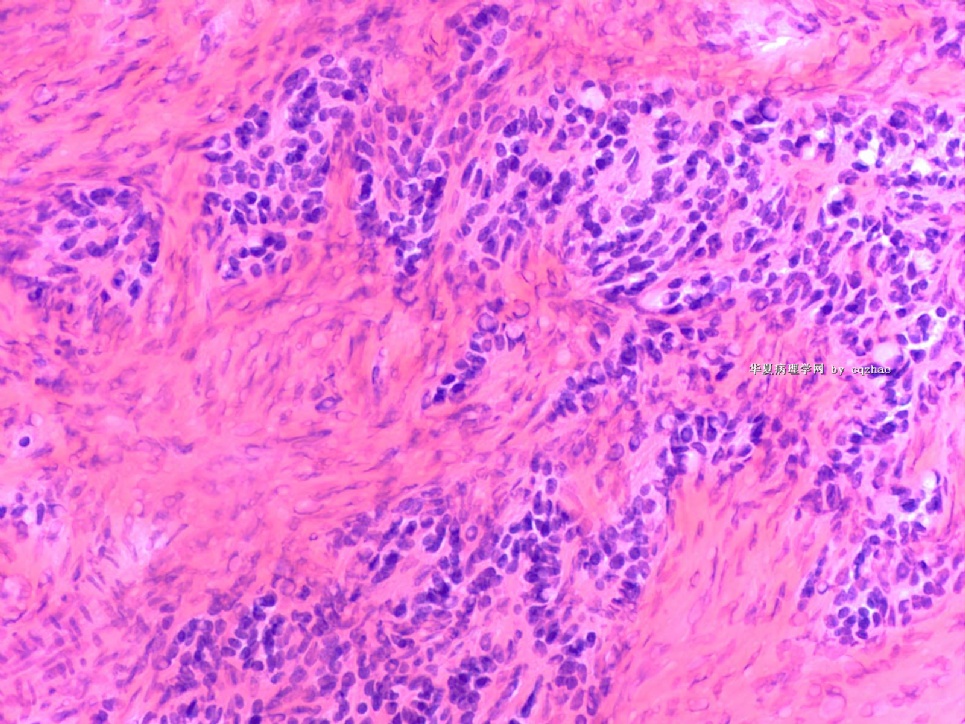
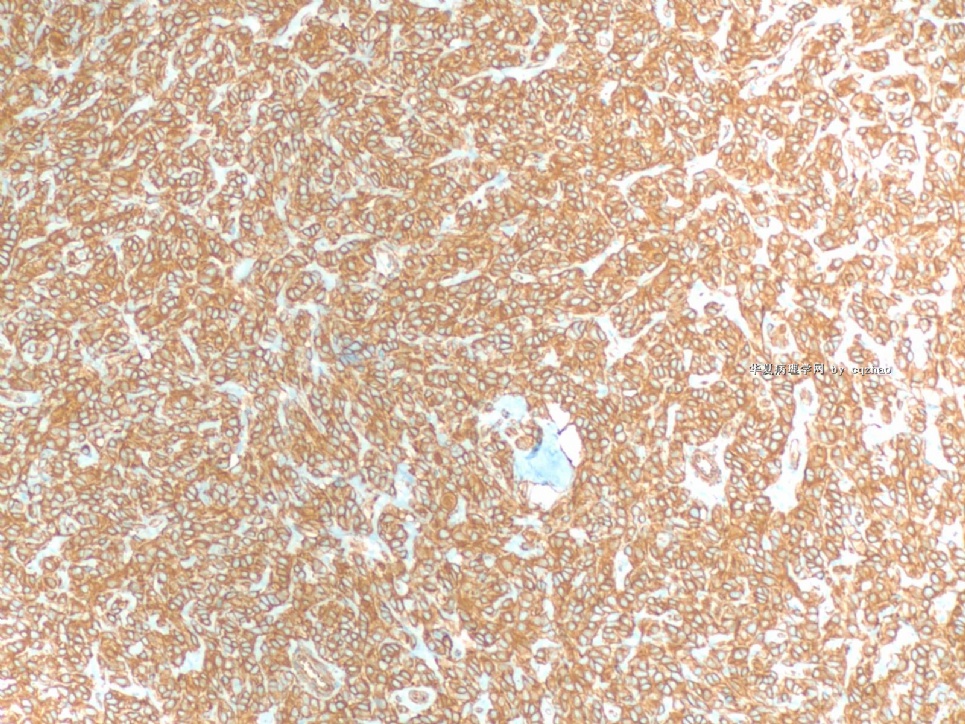
- B1590Interpretation: Ovarian stromal tumor with features of sclerosing stromal tumor and thecoma
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
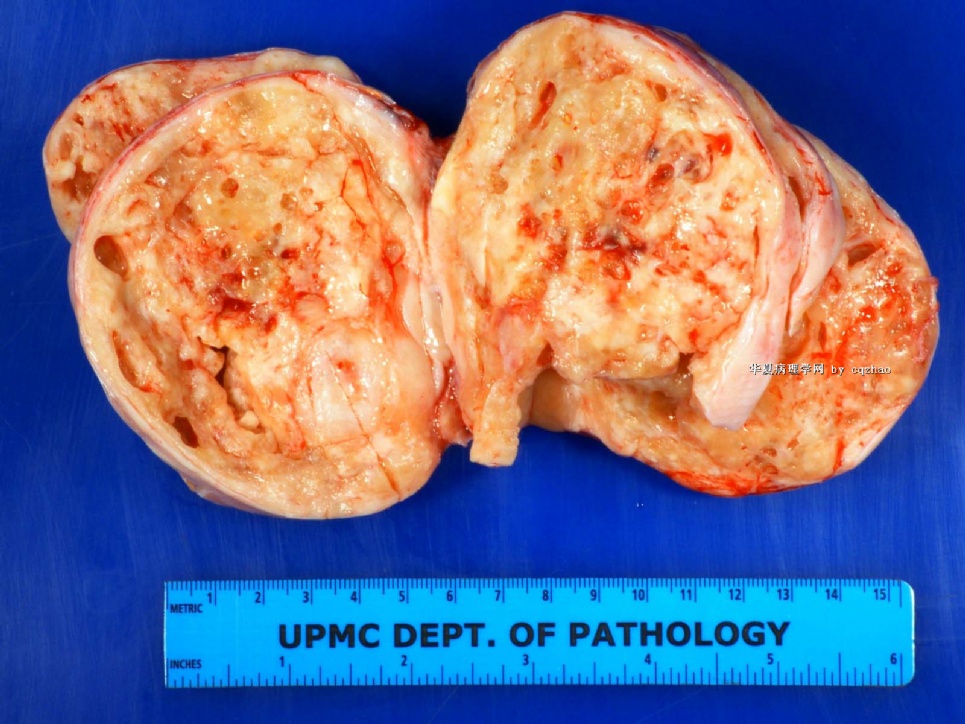
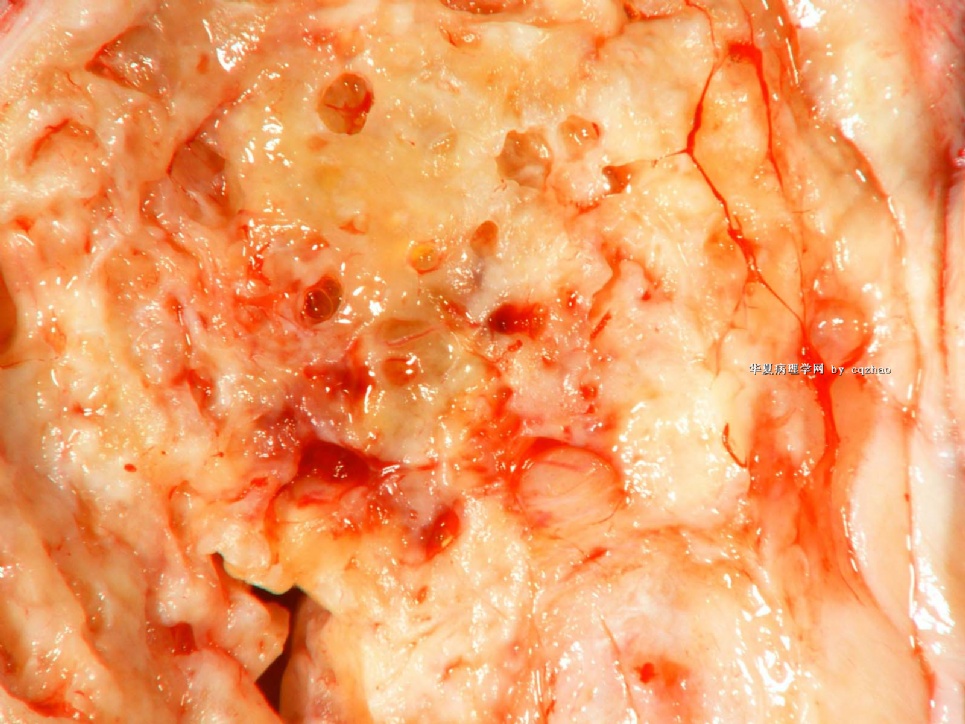
| 肉眼检查: | |||||
40-45 y/f with hx of cervical ca with radiation, chemotherapy, ovarian mass 11 cm. I did frozen. Gynecologist came to frozen room to sit with me to read frozen slide.
What can you tell your surgen about the case if your were the pathologist?
What is your differential dx?
I ordered IHC in frozen block and will know basic result tomorrow.
abin译:
20分钟前的卵巢肿瘤冰冻切片。我们能告诉妇科医生什么?
40-45岁女性,有宫颈癌病史和化疗、放疗史。卵巢肿块11cm。我做冰冻切片,妇科医生跑到冰冻室,和我坐在一起看冰冻切片。本例,如果你是病理医生,你能告诉手术医生什么?
你的鉴别诊断是什么?
我用冰冻切片做了免疫组化,明天会知道基本结果。
-
本帖最后由 于 2009-07-24 08:08:00 编辑
相关帖子
-
本帖最后由 于 2009-04-25 19:02:00 编辑
IHC results:
Epithelial markers are negative: AE1/AE3/Ck7/ck20/Cam5.2
Other negative markers:
S100, HMB45
Mamaglobin
Inhibin, CD99
SMA, Caldesmon
Synaptophysin, chromogranin
ER, PR
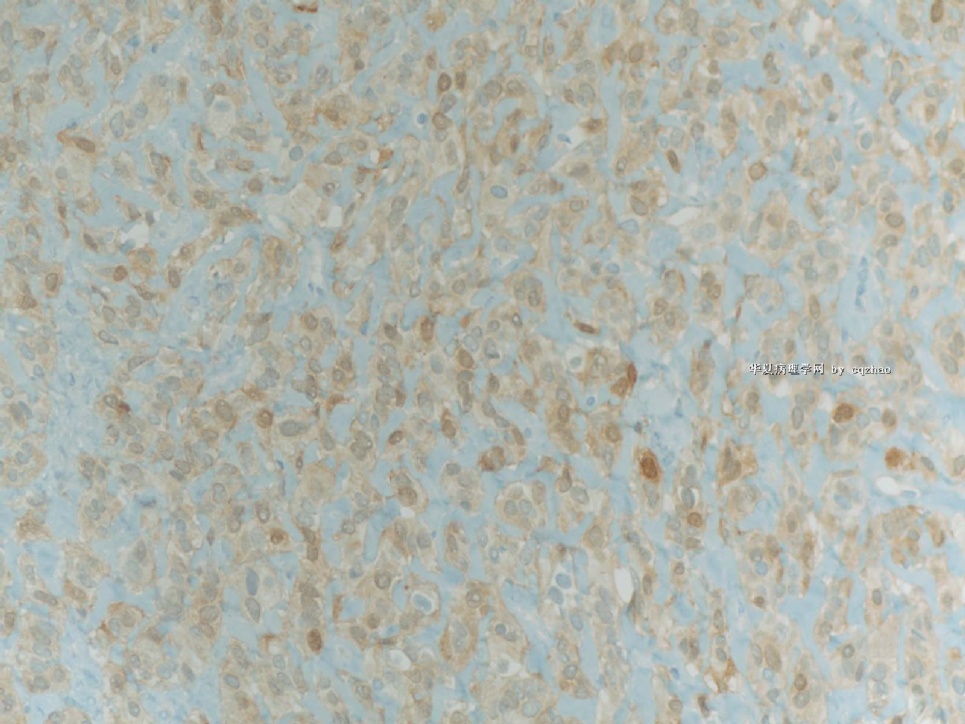
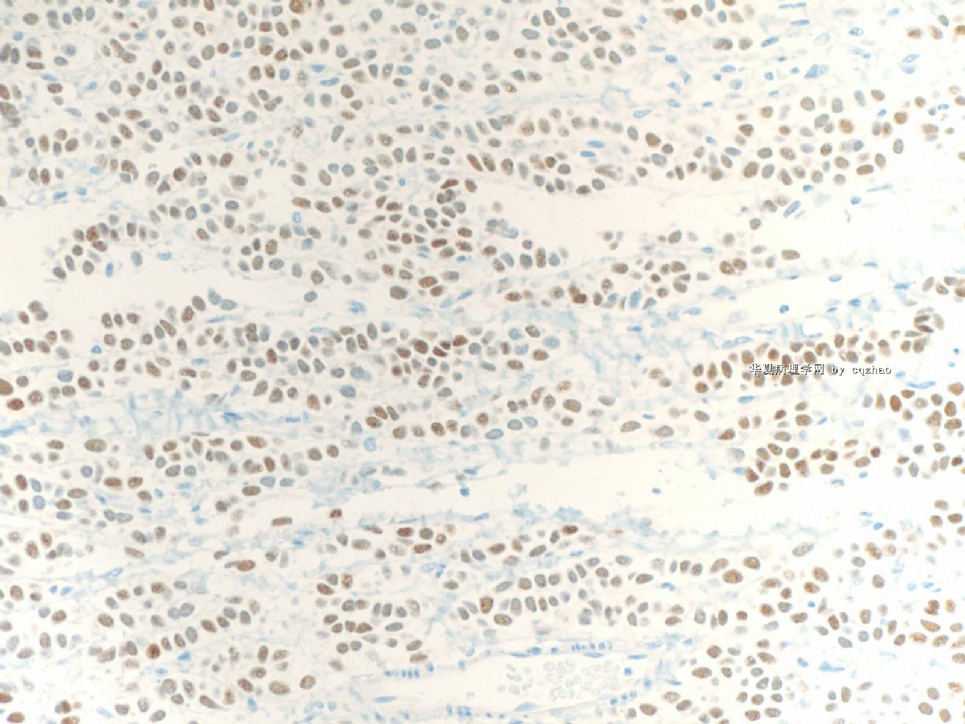
positive markers
F1 vimentin
F2 calretinin
F3 WT1
名称:图1
描述:图1
名称:图2
描述:图2
名称:图3
描述:图3
-
本帖最后由 于 2009-04-18 11:06:00 编辑
Dr. Shen, glad to meet you too in Boston. Thank your input for this case.
Agree with your and abin's interpretation. It is a tumor, mostly malignant, either primary or metastatic.
-Definetely it is not like classic ovarian epithelial carcinoma (serous, endometrioid, ccc, or mucinous).
-Other ovarian tumors include sex cord stroma tumor, neuroendocine tumor (carcinoid), or small blue cell tumors. If it is ovarian primary, I favor granulosa tumor.
-Metastatic tumors: morphology looks like breast lobular ca. Cytomorphologic features do not like colonic or upper GI tumors.
-Later I checked the history and noticed that pt had CIN3. So surgens' information are often not accurate.
-Thinking about the clinical pictures: mid age women had not carcinoma history, large ov mass 11 cm without normal ovarian tissue. I favor a ov primary tumor.
-Granulosa cell tumor (GCT) includes many growth patterns: microfollicular, macrofollicular, insular, diffuse, trabecular, watered-silk (moire-silk), gyriform, cystic, luteinized et al. This tumor shows uniform small round cells with diffuse, and single cell file growth patterns, really like breast lobular ca. However you see the first photos above, you can see tumor nests srrounding with dense stroma. About the focal signet ring cells, I favor frozen artifact. Also we can appreciate some microfollicular structures in the last photo.
-Anyway based on the clinical, gross, and microscopic features, I will choose granular cell tumor if I must pick one answer in a test.
-I told gyncologist what I mentioned above. The only issue is that the patient might not need to stage if I am sure it is a metastatic tumor. I am not sure of that. Gynecologist agree and understood. He did lymph node stage for this patient.
-In our frozen interpretation, we must write one diagnosis from three choices: malignant, benign, defer. Then we can write more detailed interpretation.
So my frozen report for this case: A) Malignant B) primary ov tumors favor granulosa tumor; metastatic tumors, breast et al. All the frozen report will be checked and compared with perminant diagnosis, as quality control. QA only cares first line dx, maligant, benign, defer. You cannot have too many defer reports.
Dr. Shen is right that we should wait for the perminant H@E slides and then choose a good block and make decision to do IHC. For this case I am very curious to know what it is. This is why I ordered the IHC yesterday and I can have the result today. Our large slides will be out 10-12 o'clock. I order IHC today I will not know the resut until Monday. IHC can be done in frozen block. In fact I asked the PA to choose another section for IHC. All mass is tumor for this case. Even though I do not see the H@E. It should be good enough for IHC.
I have not my H@E slides of today's cases yet. So I have time to read more for the reference of our chinses young pathologists. I should have IHC result today at four o'clock and will paste the result next week. Of cause all my analyses can be totally wrong.
cz