| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B1778双侧乳腺血管肉瘤,有近期随访
| 姓 名: | ××× | 性别: | 女 | 年龄: | 28 |
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
-
本帖最后由 于 2010-01-29 19:27:00 编辑

- 嫁人就嫁灰太狼,学习要上华夏网。
相关帖子
- • 乳腺肿物一例,请会诊。
- • 乳腺肿块
- • 右乳包块(男)
-
huocheng_325 离线
- 帖子:152
- 粉蓝豆:6
- 经验:247
- 注册时间:2009-04-15
- 加关注 | 发消息
-
我从头到尾看了这一例的讨论,真的是很有意思。
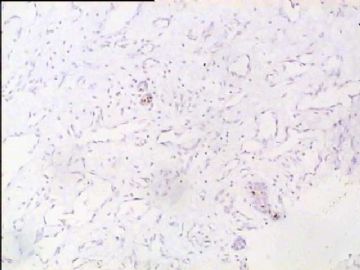
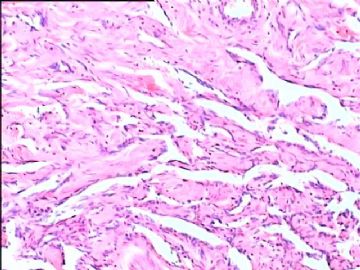
其实乳腺的这种高分化血管肉瘤在会诊和读片会中并不少见,北京市读片会、全国病理读片会多次有相同的病例,06年(也可能是05年?)IAP香港区病理年会时M.D Andson Cancer Center的教授展示过同样一例乳腺高分化血管肉瘤。
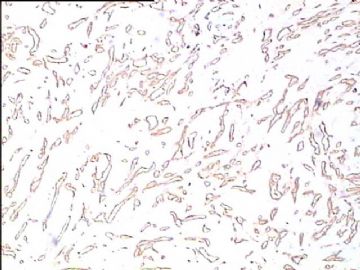
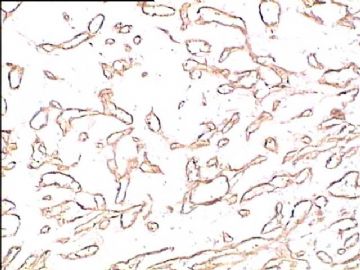
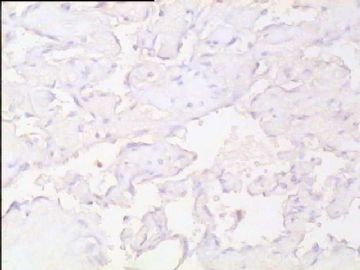
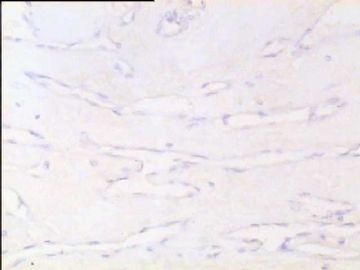
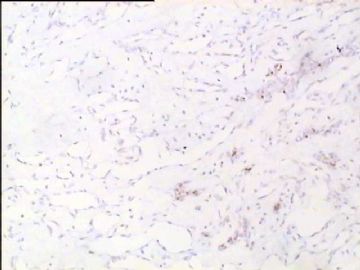
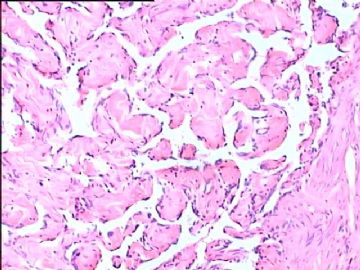
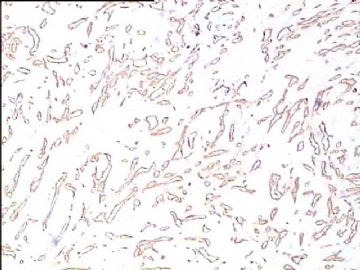
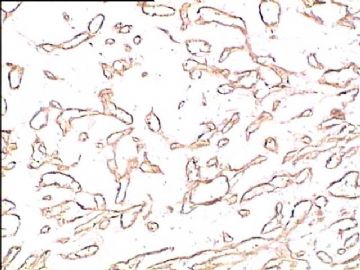
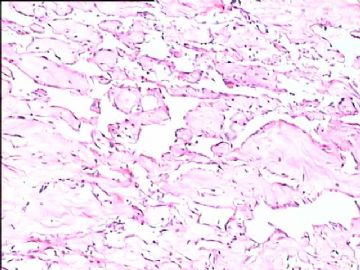
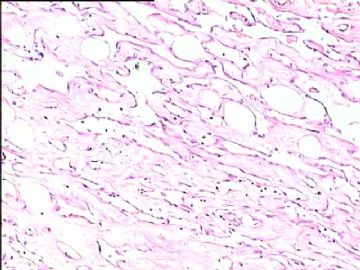
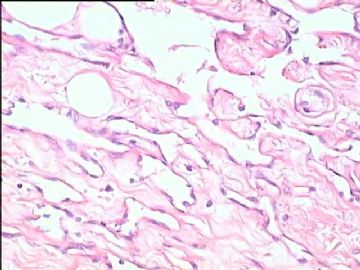
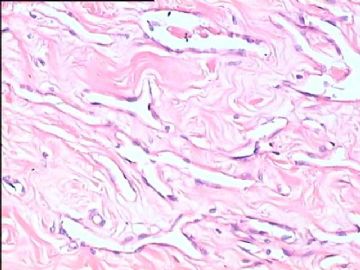
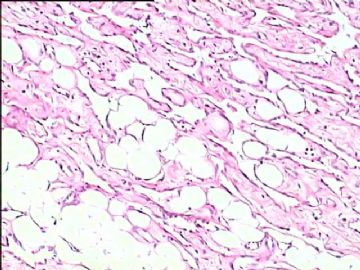
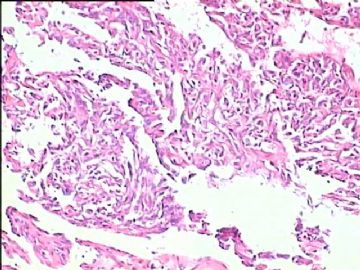
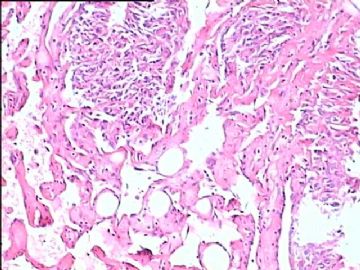
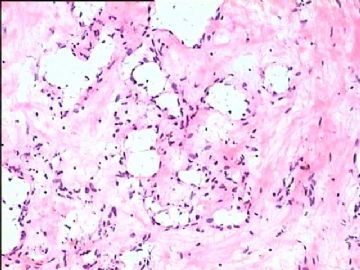
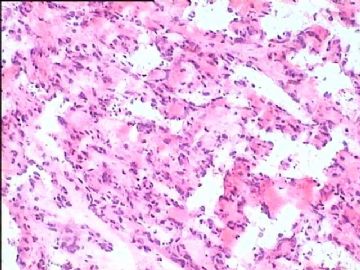
我们之所以不敢下决心诊断,原因是对这种病变的组织学了解不足,大家看一下这个图片,再对照一下软组织病理学(Soft Tissue Tumor,蓝皮的新版的又出来了),软组织中这种看似良性的相互沟通的鹿角状、迷路状相互沟通的血管腔隙,是诊断的特征性病变。以后看到得多了,胆子自然就大了。这种高分化血管肉瘤预后并不好,对治疗反应很差。
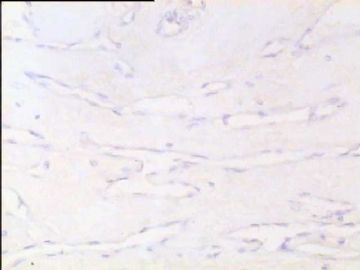
有一种情况下,也可出现与上述非常相似的病变,是在血栓机化时,这时决不能诊断为高分化血管肉瘤,一定要慎之再慎!
类似的情况下冰冻直接诊断,风险还是比较大的。如果遇到这种情况,建议跟外科大夫沟通,告诉他们我大概有9成左右的把握,还有一些类似的病变需要鉴别。请他们与病人家属商量,以决定手术是否继续进行。在事先沟通的情况下,一般不会发生后续的医疗纠纷。
总之,冰冻有风险,大家(病理大夫、外科大夫、病人家属)共承担,病理大夫不要逞强,独自承担风险。

- 我的微博:眼镜加显微镜 访问地址:http://weibo.com/pathology
-
Am J Surg Pathol. 2008 Jun;32(6):943-50.
-
Atypical vascular lesions after surgery and radiation of the breast: a clinicopathologic study of 32 cases analyzing histologic heterogeneity and association with angiosarcoma.
Department of Pathology and Laboratory Medicine, Emory University School of Medicine, Atlanta, GA 30322, USA.
We report the clinicopathologic study of 32 cases of atypical vascular lesions (AVLs) after surgery and radiation of the breast, which were referred to us in consultation over a 17-year period. The patients, all women, ranged in age from 41 to 95 years (mean 61 y). The lesions developed within the radiation field from 1 to 12 years (median 6.0 y) after therapy. They occurred as one (n=18) or more (n=10) flesh-colored papules or erythematous patches/plaques ranging in size from 1 to 60 mm (mean 8.0 mm, median 4.0 mm). Tumors could be divided into 2 histologic types: a lymphatic type (LT) (n=22) and a vascular type (VT) (n=10). LT AVLs consisted predominantly of thin-walled, variably anastomosing lymphatic vessels that were usually confined to the superficial dermis but occasionally extended into the deep dermis and even subcutis. The VT (n=10) typically consisted of small, irregularly dispersed, often blood-filled, pericyte-invested, capillary-sized vessels involving the superficial or deep dermis. VTs were often associated with extravasated erythrocytes, hemosiderin, and a surrounding minor LT component. In 4 cases, endothelial atypia, consisting of nuclear and nucleolar enlargement, was noted. Follow-up of 21 patients with LT AVLs (1 to 106 mo; mean 47 mo) disclosed recurrence/additional lesions in 6, all of whom had additional surgery. Of the 21 patients, 17 are alive without disease, 1 is alive with disease, 1 died of breast carcinoma, 1 died of unknown causes, and 1 showed progressive histologic changes in the AVLs over a period of 5 years resulting in a well-differentiated angiosarcoma. Follow-up in 8 patients with VT AVL (2 to 181 mo; mean 40 mo) disclosed that 6 were alive and well, but 2 of the 4 patients whose lesions displayed endothelial atypia had additional complications. One patient underwent a mastectomy that revealed extensive residual AVL and the second developed a high-grade angiosarcoma after 14 months. We conclude that AVLs encompass a wider spectrum of changes than previously appreciated, ranging from superficial lymphatic proliferations to more complex lymphatic and capillary vascular lesions. There seems to be an association of AVL with angiosarcoma that differs depending on the histologic features, with the VT AVLs having the higher risk. In the 2 patients who developed angiosarcoma, morphologic evidence suggested AVLs to be a precursor rather than simply a risk factor. Future outcome and management studies should take into account these differences.

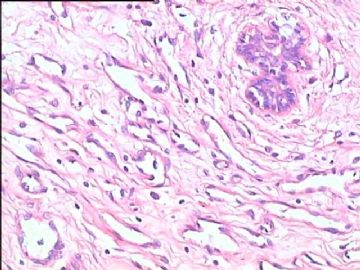
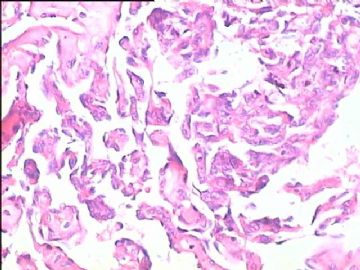
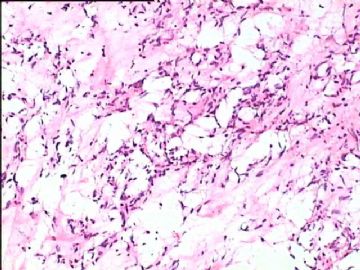



 脉管肿瘤,冰冻不能轻易下血管肉瘤,等石蜡。
脉管肿瘤,冰冻不能轻易下血管肉瘤,等石蜡。