| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B1778双侧乳腺血管肉瘤,有近期随访
| 姓 名: | ××× | 性别: | 女 | 年龄: | 28 |
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
-
本帖最后由 于 2010-01-29 19:27:00 编辑

- 嫁人就嫁灰太狼,学习要上华夏网。
相关帖子
- • 乳腺肿物一例,请会诊。
- • 乳腺肿块
- • 右乳包块(男)
-
zhang197510 离线
- 帖子:409
- 粉蓝豆:2971
- 经验:448
- 注册时间:2009-03-22
- 加关注 | 发消息
Am J Surg Pathol. 2008 Dec;32(12):1896-904.![]()
Primary angiosarcoma of the breast: clinicopathologic analysis of 49 cases, suggesting that grade is not prognostic.
Nascimento AF, Raut CP, Fletcher CD.
Department of Pathology, Brigham and Women's Hospital,
Mammary angiosarcoma is a rare neoplasm, accounting for about 0.05% of all primary malignancies of the breast. It is currently believed that histologic grading of mammary angiosarcomas plays an important role in prognostication. Forty-nine cases of primary angiosarcoma of the breast were retrieved from our files. Clinical details and follow-up information were obtained from referring pathologists and clinicians, and by chart review. All statistics were performed using Fisher exact test and only P<0.05 was considered significant. Recurrence-free survival and overall survival curves were established using Statistica software version 5.5 (StatSoft Inc). All patients were female with ages ranging from 15 to 74 years (mean 41.5, median 40). Peak incidence was between the ages of 30 and 50 years. All tumors examined were located within breast parenchyma with or without minor cutaneous involvement. The right side was more commonly affected than the left side (66% vs. 29.5%). Tumor was bilateral at presentation in 2 cases (4.5%). Tumor size varied from 0.7 to 25 cm (mean 6.7, median 5). Most patients presented with a palpable, painless mass. Two patients had a history of prior radiation treatment for breast carcinoma. Histologically, primary tumors were graded using Rosen's 3-tier system: 17 tumors (35.4%) as low grade, 17 (35.4%) as intermediate grade, and 14 (29.2%) as high grade. Forty-six patients were treated surgically, 11 underwent chemotherapy, and 12 patients received radiotherapy. Follow-up was available in 41 patients (83.7%, median duration 29 mo). Ten patients (24.4%) showed evidence of local recurrence within 11 to 60 months (median 36) after diagnosis. Twenty-four patients (58.5%) thus far have developed metastases, which were most commonly to lung, liver, skin, and bone. Time interval between diagnosis and metastasis ranged from 2 to 144 months (median 34). Eighteen patients (44%) so far have died of disease and 1 died of presumably disseminated breast carcinoma. Five patients (12.2%) are alive with disease and 15 patients (36.6%) are alive with no evidence of disease. Statistical analysis evaluating correlation between tumor grade and size, and rate of local recurrence, metastasis, and death owing to disease showed no significant difference among tumors of different grades. The median recurrence-free and overall survival rates for the entire cohort were 2.8 and 5.7 years, respectively. In conclusion, mammary angiosarcoma is a rare disease that affects relatively younger patients. This tumor seems to have an overall similar clinical course as other types of angiosarcoma arising in skin or soft tissue; it carries a moderate risk of local recurrence, and a high risk of metastasis and death. In this large series, there is no correlation between histologic grade and patient outcome, more in line with angiosarcomas at other sites
-
I do not have any meaning to challenge your diagnosis. It is not necessary that expert pathologists must have correct diagnosis. Also it does not mean that your and other large hospitals' s sarcoma diagnosis msut be wrong. Their evaluation and comment from these experts are based on a few photos only. No pathologists would make true consulation based on the photos like in the website. Their oppinions are jsut for your reference.
| mentioned in all page in the website: 本网站内容仅供学术研讨、交流之用,不能作为临床诊疗依据 |
I think it is important for other pathologists to learn how to evaluate a complicated case in your true clinical practice. Cautious, cautious, and cautious.
I noticed that a lot of people above made sarcoma diagosis without doubt. I wish you treated this case just like when you took a test, but not in your true practice.
By studying this case I learn a lot about these kinds of lesions.
Thank wfbjwt for sharing this challenge case again, and also thank many people in China and the USA for your comment.
Ok, I will paste a abstract a soft tissue pathologist emailed me.
-
本帖最后由 于 2009-06-16 12:24:00 编辑
I mentioned in the begining I am gyn/breast pathologist and know a little about soft tissue tumor.
我在一开始就提到,我是妇科/乳腺病理医生,对软组织肿瘤了解不多。
However I am very interested in your case, 28 y/f with b/l angiosarcoma. For learing purpose, I downloaded the photos and sent to several experts for evaluation. I copied their comment and paste here:
然而我对这一例非常感兴趣,28岁女性有双侧血管肉瘤。出于学习目的,我把图片下载,发给几位专家供评价。我把他们的评论复制如下:
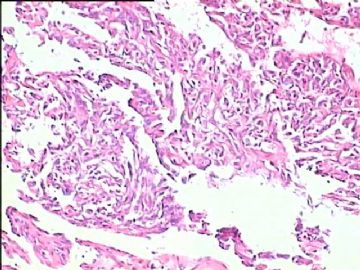
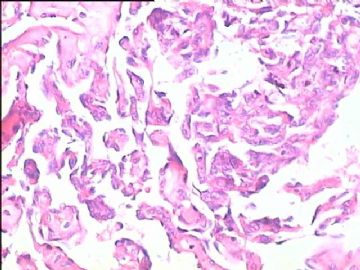
1. Dr. A (full professor of soft tissue pathology) is worried it could be an angiosarcoma because of the anastomosing channels and angiosarcoma in the breast can have very subtle nuclear features. She suggested they might get a ki-67 and CD34.
Dr.A(软组织病理教授)担心它可能是血管肉瘤,因开放的血管腔且乳腺的血管肉瘤可能仅有非常细微的核特征。她建议做ki-67 和CD34免疫组化。
2. Dr. B (full professor of soft tissue pathology) thought it was best to look at the glass slides. Did not give her comment.
Dr.B(软组织病理教授)认为最好要看到切片,没有给评论。
I called her and asked her comment for learning.
我打她电话,询问她的评论以求学习。
She comment:
Dr Zhao,
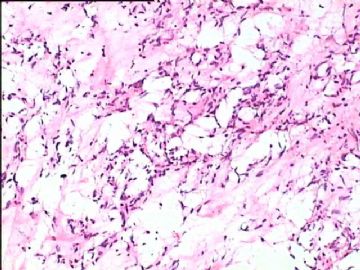
The case is difficult to evaluate from my end---is this bilateral biopsy?? Is the lesion localized like papillary endothelial hyperplasia “Masson’s”?? She is young if this were a older pateient the complex channels would meet would meet woodruf’s originl criteria for grade 1 if you find infiltration of the complex spaces INBETWEEN glands and expanding/ widely displacing the acinar unit
她的评论:
Dr Zhao,
本例难以评论,超出了我的能力---这是双侧活检吗?病变的部位像乳头状血管内皮增生吗?“Masson's?”患者太年轻,假如她是老年患者那么复杂的血管腔、假如发现浸润到腺体之间并且扩展到/广泛取代腺单元----可能符合woodruf关于1级血管肉瘤的最初标准。
3. Dr. C (outsite institute, national well-known expert in soft tissue pathology).
It Looks like papillary endothelial hyperplasia. A hemangioma can be behind this also. Need to read glass slides for definite diagnosis.
Dr. C(outsite institute,本国著名软组织病理专家):它看上去像乳头状血管内皮增生。血管瘤也可能有这样的表现。需要阅片进一步明确诊断。
4. Dr. D (outsite institute, breast pathology expert).
Without any history of irradiation, I also suspect a benign vascular lesion,probably associated with her prior lactation. A Masson's intravascular papillary endothelial hyperplasia like Dr. xxxxx suggested sound like a great thought!
Dr. D (outsite institute, 乳腺病理专家):没有放射病史,我也怀疑是良性血管病变,可能与她以前的哺乳有关。Dr.B提出的Masson's血管内乳头状血管内皮增生,可能是非常好的考虑!
5. Another 3 breast pathologists:
Cannot make sarcoma diagnosis based on the photos. Need to read true slides for evaluation.
另3位乳腺病理专家:不能根据图片诊断肉瘤。需要阅片评价。(abin译)
-
本帖最后由 于 2009-04-29 19:12:00 编辑
Thank you very much for your detailed explaination. cz
| 姓    名: | ××× | 性别: |   | 年龄: |   |
| 标本名称: |   | ||||
| 简要病史: |   | ||||
| 肉眼检查: |   | ||||
-
<!--
/* Font Definitions */
@font-face
{font-family:宋体;
panose-1:2 1 6 0 3 1 1 1 1 1;
mso-font-alt:SimSun;
mso-font-charset:134;
mso-generic-font-family:auto;
mso-font-pitch:variable;
mso-font-signature:3 135135232 16 0 262145 0;}
@font-face
{font-family:"\@宋体";
panose-1:2 1 6 0 3 1 1 1 1 1;
mso-font-charset:134;
mso-generic-font-family:auto;
mso-font-pitch:variable;
mso-font-signature:3 135135232 16 0 262145 0;}
/* Style Definitions */
p.MsoNormal, li.MsoNormal, div.MsoNormal
{mso-style-parent:"";
margin:0cm;
margin-bottom:.0001pt;
text-align:justify;
text-justify:inter-ideograph;
mso-pagination:none;
font-size:10.5pt;
mso-bidi-font-size:12.0pt;
font-family:"Times New Roman";
mso-fareast-font-family:宋体;
mso-font-kerning:1.0pt;}
/* Page Definitions */
@page
{mso-page-border-surround-header:no;
mso-page-border-surround-footer:no;}
@page Section1
{size:595.3pt 841.9pt;
margin:72.0pt 90.0pt 72.0pt 90.0pt;
mso-header-margin:42.55pt;
mso-footer-margin:49.6pt;
mso-paper-source:0;
layout-grid:15.6pt;}
div.Section1
{page:Section1;}
-->
感谢大家对帖子的关注,提出的问题也很有借鉴性,感谢了!
此例石蜡切片经西南医院、北京协和、山东省立等医院会诊,诊断为高分化血管肉瘤。
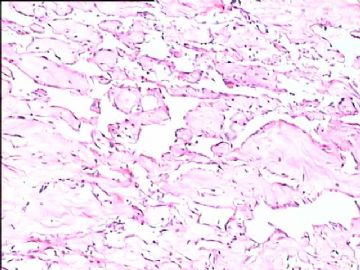
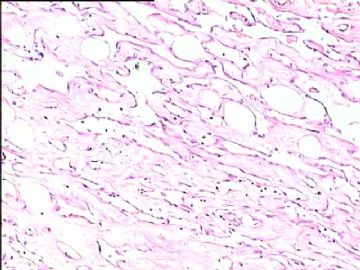
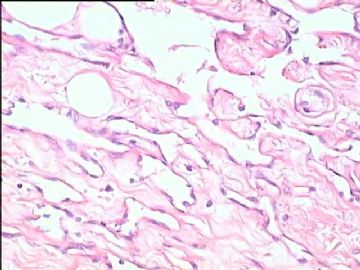
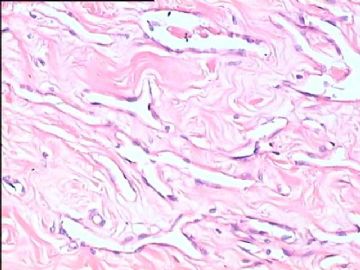
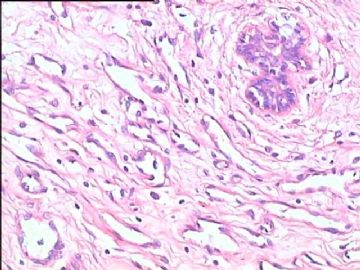
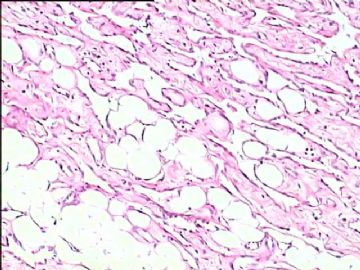
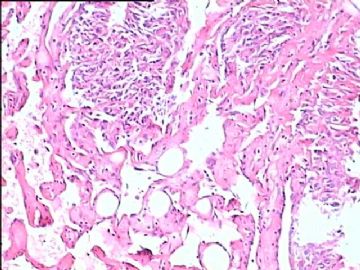
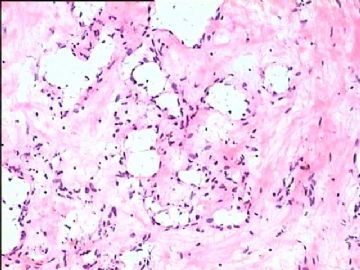
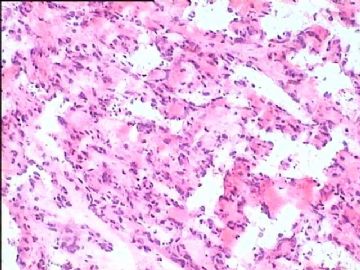
我 们的诊断依据:1、肿瘤暗红色,质韧,多发结节状生长,无包膜,周围组织界限不清;2、镜下表现为相互吻合的窦隙样血管,血管壁薄扩张状,部分呈乳头状突入腔内,乳腺组织萎缩,仅存少量导管;3、内衬细胞不明显,异型性难以观察(这也是乳腺高分化血管肉瘤的表现之一);4、肿瘤血管弥漫浸润于胶原纤维、脂肪组织、乳腺组织之中(见上传 图)。双侧乳腺基底部可见肿瘤残余,左侧乳腺局部有实性区,约10%-20%,此区细胞异型性有所表现,大概左侧肿瘤划到中分化亦可,帖子中个别图也显示了此类区域。右侧乳头、皮肤有累及。免疫组化,包括内皮标记和激素受体无鉴别诊断作用,故未做。鉴别诊断基本上应该是各种良性和中间型血管源性肿瘤,组织图像及生物学特征有助鉴别,另外,乳腺间质假血管瘤样增生有如下特点,可鉴别:体积小,局限,病变广泛者罕见;切面灰白而不是暗红;可见血管样裂隙,有的相互吻合,但少有乳头形成,管腔常挤压闭合状,而非扩张状;乳腺小叶常存在;无脂肪浸润。
此例患者是我一位朋友的亲戚,术前我看过患者,有点心理准备,术中也想报的保守点,不过现场压力很大(决定手术范围及是否安放假体),最后才下了决心。再次感谢各位专家和同行,也让我学了不少东西,以后遇到这样的诊断确实要慎之又慎。

- 嫁人就嫁灰太狼,学习要上华夏网。
-
Dear Dr. Wfbjwt,
| 以下是引用wfbjwt在2009-4-28 21:05:00的发言:  此例病例双侧乳腺均见两个结节,大小相近,直径约5cm,术后病理经5家国内大医院会诊,结果均是血管肉瘤。这也是我们的结果。患者目前恢复良好,后续治疗没好办法,如有知道好的治疗方案,请提供,谢谢! |
我很吃惊这么多人诊断血管肉瘤。我基本不同意该诊断,倾向良性。无核异性,无核分裂,细胞非常小且一致。请问你们诊断血管肉瘤的依据。同意赵大夫意见。血管肉瘤基本不能冰冻切片诊断。
本病例考虑良性血管瘤,pseudoangiomatous stromal hyperplasia (PASH), PASH 细胞ER阳性,a low grade vascular lesion is also in the differential。
我在以前的贴上看到有人说:乳房血管瘤都是恶性,这是不对的,我看到很多乳房良性血管瘤,相反恶行较少。
-
本帖最后由 于 2009-06-16 12:28:00 编辑
Seems most people think it is angiosarcoma case. This is soft tissue pathology area. Clearly it is not a obvious dx for benign or malignant. I know very little on soft tissue and will think more about this case. Hemangioma is not a very uncommon lesion in breast. I was in breast core biopsy banch in the past week. I had about 90 breast core biopsy cases. I saw two cases of small hemangioma.
I have a quesion for your guys especially for 楼主。Obviously the differential dx for this case includes low grade angiosarcoma and benign hemangioma. What is your criteria for diangosis of angiosarcoma for this case?
Just for learning purpose. Thanks, cz