| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
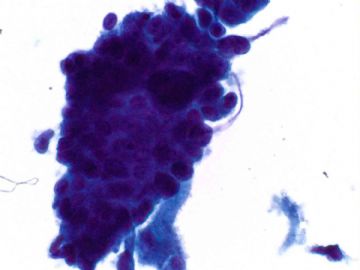
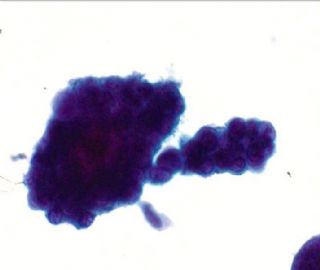
- an easy case for you-Pap test (cqz 3)
-
Recommend one paper from a very good Chinese pathologist- Fan Lin
Cancer. 2007 Apr 25;111(2):74-82.
Immunohistochemical detection of p16INK4a in liquid-based cytology specimens on cell block sections.
Liu H, Shi J, Wilkerson M, Huang Y, Meschter S, Dupree W, Lin F.
Department of Pathology,
BACKGROUND: Colposcopy biopsy procedure is a standard recommendation for atypical squamous cell cannot exclude high-grade lesion (ASC-H) in abnormal Papanicolaou smears. p16 (p16INK4a), a cell cycle regulator, has been shown to be overexpressed in squamous dysplasia. To further improve the diagnostic accuracy of the ASC-H Papanicolaou smear and to reduce unnecessary procedures, the authors evaluated the utility of immunodetection of p16 in liquid-based cytology specimens on cell blocks. METHODS: Seventy-five liquid-based (SurePath; TriPath Imaging, Inc.
| 以下是引用小荷在2008-12-18 21:41:00的发言:
深深谢意!收获多多! 请教一个问题:“无论什么年龄段出现了非典型的的子宫内膜腺上皮细胞都应该做活检,.如果刮宫标本正常还应该再做阴道镜,所以非典型的子宫内膜细胞是一定要报出来。” 如果是非典型腺细胞,不能明确是子宫内膜,还是宫颈管,需要活检吗?! 如果能明确是非典型宫颈管腺细胞,需要活检吗? |
You are right:
AGC, endometrial: endometrial and endocervical sampling. need to do colposcopy if no endometrial lesion noted.
All other AGC, (AGC, NOS; AGC, endocervical):
Colposcopy with endocervical sampling, high risk HPV testing. In additon, endometrial sampling is needed for patients are >35 year, or patients have risk for endometrial lesions ---family history, overweight et al.
So AGC is critical call. You have to be think over and try to not overcall or mis-call. A big challenge for all pathologists. I did AGC research for many years and reviewed more than 1000 AGC cases with follow up. I still feel struggle for most cases. Ha, ha. We all need learning from the practice.
It seems my online talk about AGC was not very effective for your guys. Sorry about this. In fact pathologists cannot learn pathology from few talks. Importance is that we learn from our practice and mistakes.
| 以下是引用月新在2008-12-18 11:23:00的发言: It does mean u answer is wrong. 并非说你们的回答是错的,但是不完整。It is true most serous carcinomas are from endometrium, but some can arise from endocervix. 虽然大部分浆液性癌起源于子宫内膜,但是也有部分起源于子宫颈,Just wonder you think you can tell the difference between cervical papillary serous carcinoma and endometrial papillary serous carcioma. 你肯定认为你可以鉴别宫颈或子宫内膜的乳头状浆液性癌,In fact it is very difficult. Endometrioid carcinoma, clear cell carcinoma can arise from endometrium and endocervix. 实事上,子宫内膜样癌,透明细胞癌都可以起源于子宫内膜,也可以起源于子宫颈,Often it is difficult to tell the origins even though you try to use IHC in the biopsy specimens.认清起源是非常困难的,就是用免疫组化也没有用。
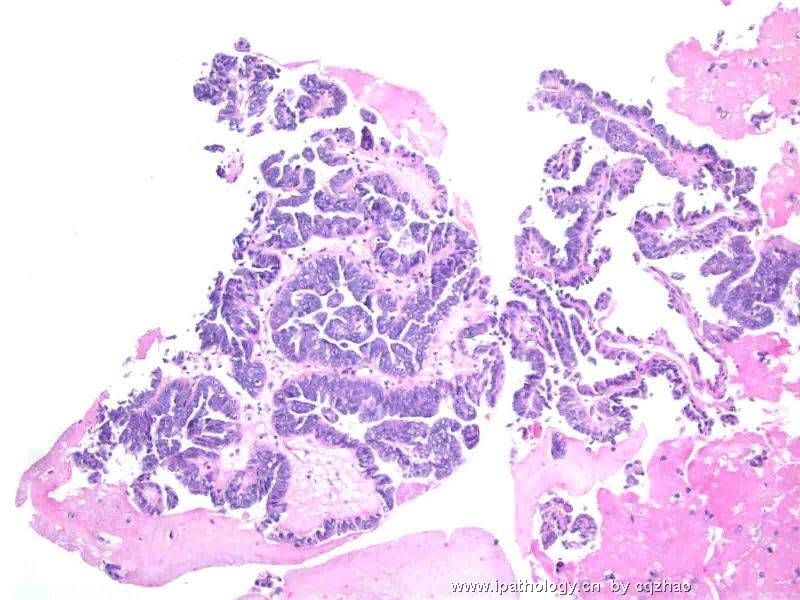
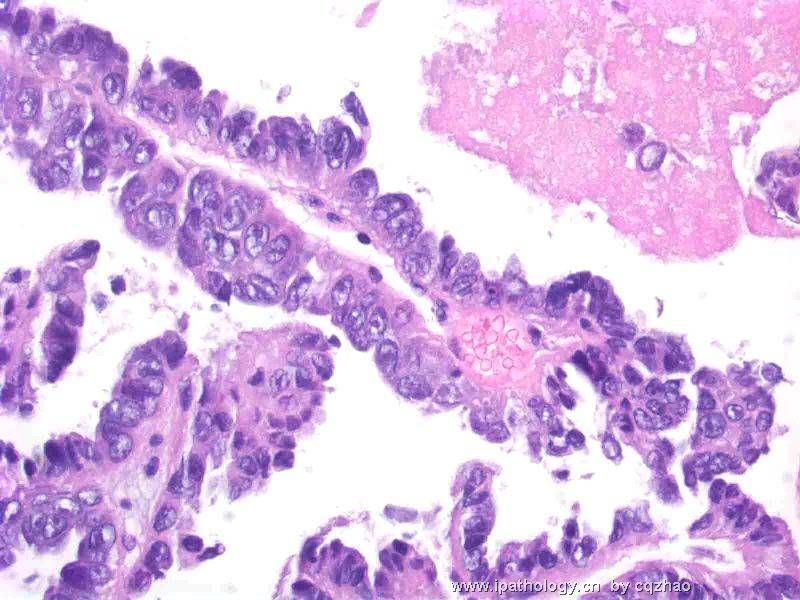
感谢赵老师给我上了一课,一幅图,引出这么多的思维差距,虽然我可以感觉到这是一个恶性的腺上皮细胞团,但是如何进一步工作,如何发病理报告又是不同。看到了宫颈涂片中有上述的异形上皮细胞团,如果光说话让临床医生做这做那,自已不再做实际工作,不行,赵老师用剩余的TCT液体做成细胞块,一下子解决了大问题,把肿瘤的组织形态弄到手了,但是如何描述这样的形态,如何写报告又是一个思维落差。比如是乳突状浆液性腺癌,是子宫颈,还是子宫内膜,大包大揽,肯定说子宫内膜,当然子宫内膜多见,但是宫颈完全可以有。病理报告错一个字,意谓着不完整不科学,也就是完全错误。这一例给我的经验。应该象赵老师这样,做事有缜密性,自已应该做工作一定要做完,思维有多样性,考虑问题复杂,报告有原则性,不能说过头话,原则无论如何不能偏离。这次举一反三。大有收获。 |
-
本帖最后由 于 2008-12-18 01:58:00 编辑
It does mean u answer is wrong. It is true most serous carcinomas are from endometrium, but some can arise from endocervix. Just wonder you think you can tell the difference between cervical papillary serous carcinoma and endometrial papillary serous carcioma. In fact it is very difficult. Endometrioid carcinoma, clear cell carcinoma can arise from endometrium and endocervix. Often it is difficult to tell the origins even though you try to use IHC in the biopsy specimens.
| 以下是引用天山望月在2008-12-17 13:28:00的发言:
Yes,i know that is from some residual fluid left in the lab . So important! hehe
|
What are the likely diagnosis?
A. Endometrial Endometroid adenocarcinoma
B. Malignant Mixed Mullerian Tumor
C. Endometrial Papillary Serous Adenocarcinoma
D. Reactive Mesothelial Cells
E. Malignant Mesothelioma
F. Endocervical Papillary serous adenocarcinoma| 以下是引用法师在2008-12-15 19:38:00的发言:
1、如果是宫颈管内膜细胞,除非是腺癌,因为正常的宫颈管内膜细胞一般不会呈乳头状,如果是腺癌,又感觉差了点什么。 2、如果是子宫内膜细胞,也除非是癌,正常的子宫内膜细胞没这么大,但也觉得差了什么,子宫内膜癌形成的乳头细胞核之间或多或少有间隙,这个好像很紧凑。 幸好我没遇到,万一真遇到了,就真的糊涂了,就报个非典型腺细胞,无法明确来源,然后再慢慢查去。 |
| 以下是引用天山望月在2008-12-14 20:15:00的发言:
回复赵老师: 1、在做TCT时,我喜欢每次将剩余的液体,再离心沉淀备用,如果液基图片有可疑细胞,或制片欠佳,再将备用液制片或做细胞块,再染色观察或做免疫组化等。 2、常与临床沟通,只要有异常细胞,都要和临床联系,询问病史和其它相关检查,并建议做相关的检查,如宫颈外观情况、B超示内膜情况、既往史等。可建议分段清宫、宫颈活检、查HPV、查内分泌激素等。
|
It is not uncommon to see the normal endometrial cells in women age >45 even the LMP more than 12 days.
We should report the presence of endometrial cells if women 40 y or above. Then we need to mention the EM cells are consistent with LMP, or > 12 days after LMP or do not know the LMP of the patient.
Normal EM cells in women <40, do not need to report regardless of LMP
Normal EM cells in women 40 or above: Clinical correlation.
Atypical EM cells: should have endometrial and endocervical sampling for all ages. If no endometrial pathology identified, colposcopy should be performed. So atypical EM cells are critical report.
My discussion is no relation to the interpretation of my above case (I do not mean which of your answers is right or wrong). So continue to guess.
Thank 月新 for your good translation
Normal EM cells in women 40 or above: Clinical correlation. 大于40岁以上的人宫颈涂片中出现正常的子宫内膜细胞. In this situation we can write the comment: Clinical correlation is suggested. It means that clinical physicians should consider patient's clinical stituation to decide how to handle the case. Basically I give the ball to the patient's physicians.
i did not say above answers are right or wrong. Just give a resonable interpretation based on your knowledge.