| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
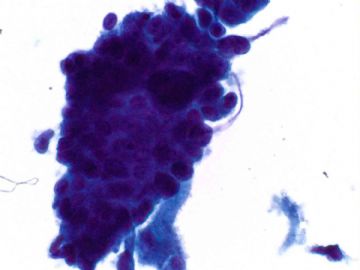
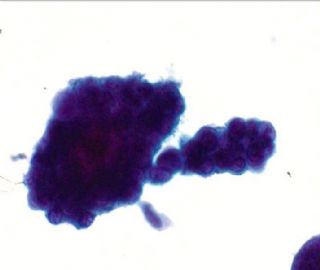
- an easy case for you-Pap test (cqz 3)
-
本帖最后由 于 2009-01-23 12:20:00 编辑
| 以下是引用abin在2009-1-19 0:07:00的发言:
这两例提出同一个问题,值得我们深入学习并在实际工作中形成明确的充满自信的思路和处理方法。这个问题就是: 细胞学AGC的进一步处理? 我的休会,请Dr.cqzhao批评指正: 1 AGC充满风险,一定要非常谨慎,不能放过,特别是老年女性 2 可疑病例,细胞块做HE和IHC 3 临床分段诊刮 4 有时起源部位难定,更需要结合临床和影像学资料。 |
Abin's summary is very good.
I showed you two cases of glandular lesions on Pap test in this topic. I want to close this topic today. Hope you can get some sense about AGC diagnosis. I have a online talk about AGC here. You can review it if you are interested in AGC. I think it is a very well prepared summary of AGC.
http://www.ipathology.cn/news_display.asp?id=2648
Thank all of you who read the cases and joined in the discussion.
I am waiting in my office for a middle night surgery for frozen. I finished this case before the frozen.
Happy Chinese New Year. But I have to work in the New Year day and week.
-
本帖最后由 于 2009-01-23 12:04:00 编辑
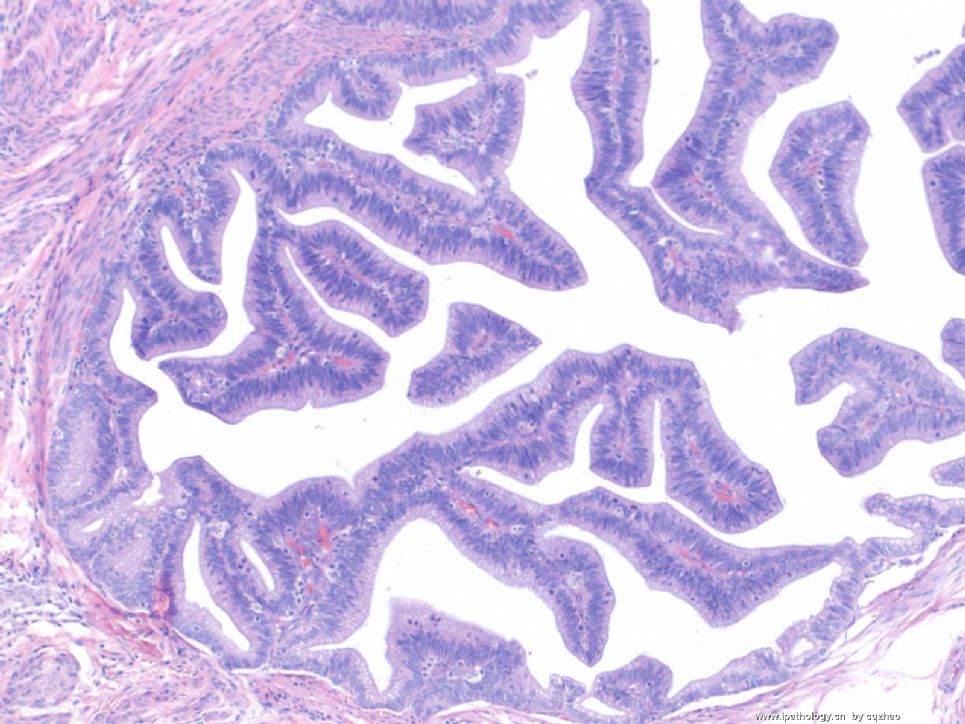
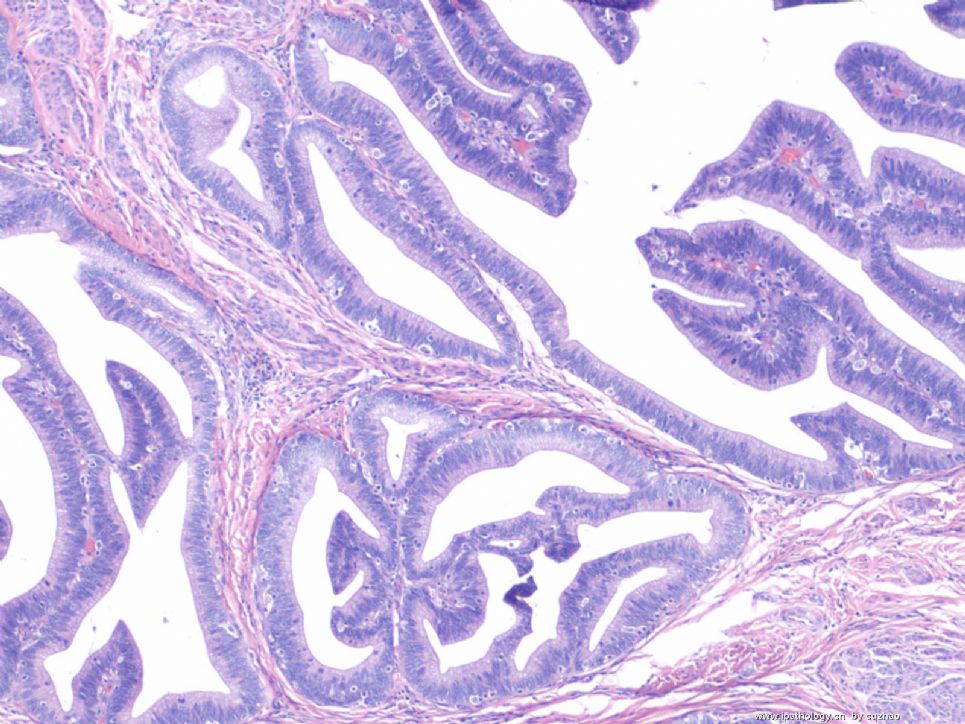
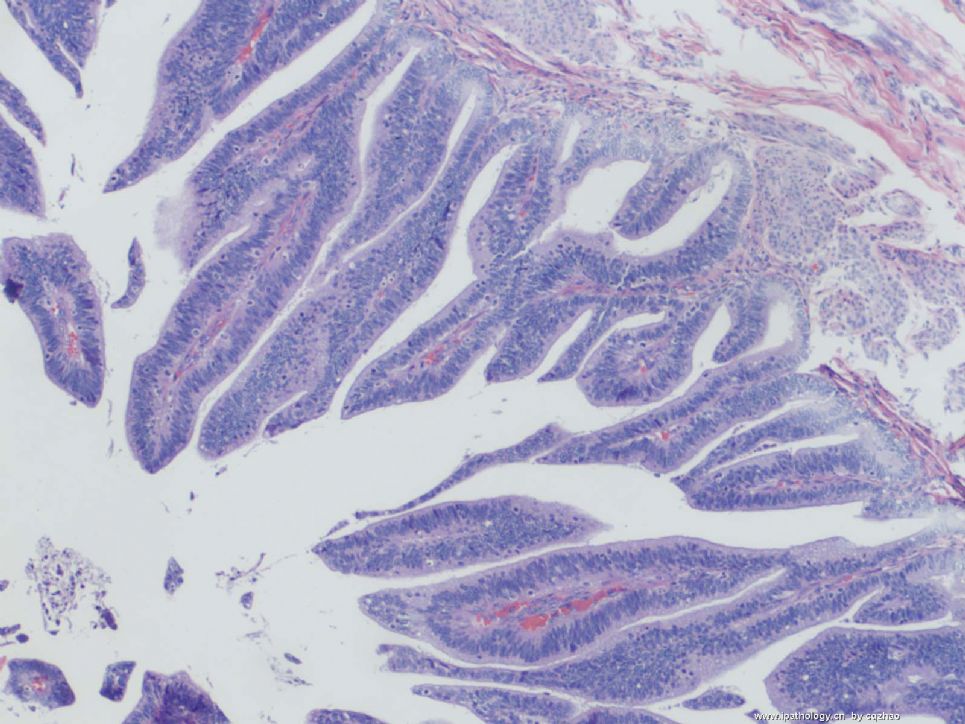
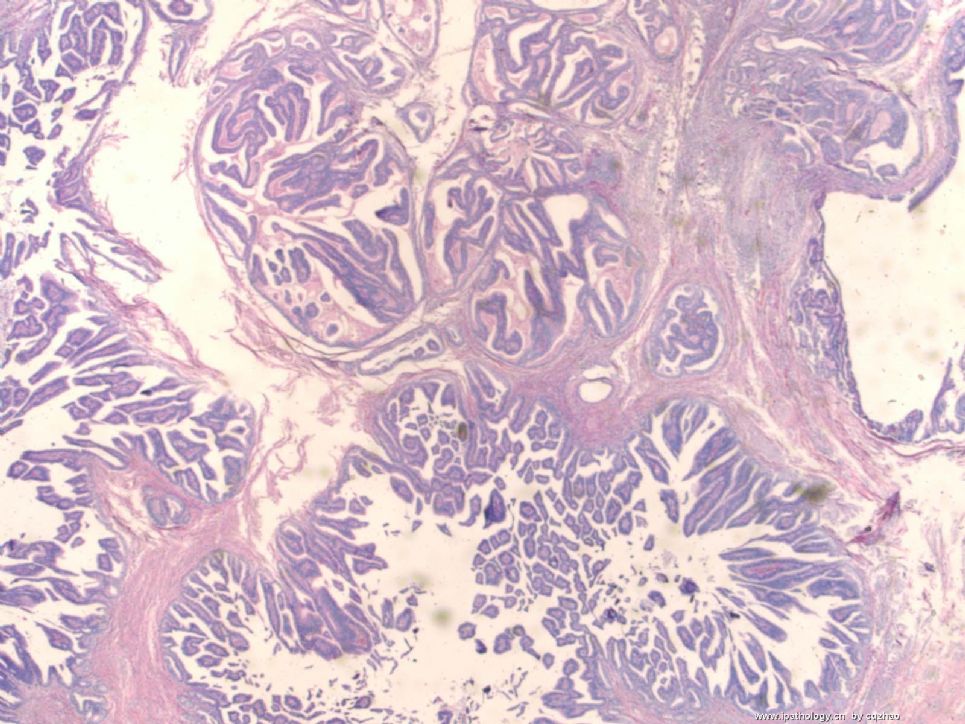
Patient had hysterectomy. The tumor was located in endocervix, and endometrim was no tumor. So final dx is well-differentiated villoglandular adenocarcinoma.
See Photos of hysterectomy.
First three Fgs: 100x
Last one: 20x
名称:图1
描述:图1
名称:图2
描述:图2
名称:图3
描述:图3
名称:图4
描述:图4
| 以下是引用cqzhao在2009-1-19 12:21:00的发言并发翻译:
|

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
Thank Abin's good analysis.
For the second case, it is a villoglandular carcinoma, a variant of well differentiated endometrioid carcinoma based on the H&E biopsy. Villoglandular carcinoma can occur in both endometrium or endocervix. The same as other adencarcinomas it is often difficult to tell the diffience by morphology. IHC can be helpful sometimes, but many times it can not help you.
I general use 4 markers, CEA, Vimentin, p16, ER.
Most endocervical adenocarcinomas: positive for cea, p16, negative for er and vimentin
Most endometrial carcinomas: positive for vimentin, ER, negative for CEA, p16.
Most endocervical carcinomas are relative to HPV infection, so p16 often diffuse and strong positive.
Ki67 and p16 stains are very useful if you are not sure for some possible high grade squamous lesions. In the same way, the two makers are very useful for confirming cervical AIS lesions. please remember p16 and ki67.
Going back to our case the IHC pattern favors an endocervical origin, even CEA is negative.
Diagnosis of cervical biopsy: Adenocarcinoma, favor endocervical origin. In the comment you can mention the IHC favors endocervical orgin. Please clinial correlation wtih imaging is suggested. Remember even though IHC 100% match with endometrial or endocervical orgins you still do not need to say it must be...... Anyway give yourself some space. Of cause for Pap diagnosis you should give you more space, especially for the origin issue. For the type of tumor in biopsy if you are confident you can call villoglandular carcinoma. Otherwise it is good enough if you call well-differentiated adenocarcinoma. However it is not a good call if you call papillary serous carcinoma. They are different if you compare my first case with the second case. This is why I put the two cases in the same topic.
抱歉在天山望月提醒下才知道Dr.cqzhao点名,主要是我很少看细胞学专栏。现在集中回答如下:
第1楼的细胞学:
AGC,疑癌。老年女性更应该警惕,需要临床进一步检查(分段诊刮)、影像学资料等。
第26楼的细胞块,HE:
高级别腺癌,可能是浆液性腺癌。需要进一步工作确定组织分型和起源部位(宫颈vs宫腔?),一组免疫组化(ER,PR,p53,Ki67,CK,VIM,CEA,P16)可能有帮助。临床进一步检查和影像学资料更有帮助。
第35楼,选择:
C. Endometrial Papillary Serous Adenocarcinoma
或
F. Endocervical Papillary serous adenocarcinoma
第52楼诊刮:
(宫腔)高级别子宫内膜腺癌,可能是浆液性腺癌。
第57楼,手术分期,完整的病理报告:
全子宫及双附件切除标本,子宫(?部位)肿瘤大小4x3x1.2 cm,浸润子宫肌层深达75%,浆液性腺癌。肿瘤
累犯右卵巢表面约4cm大小,宫颈、左附件及右输卵管未见癌。(有无盆腔淋巴?若有,注明:送检盆腔各组淋巴结共?/?枚见癌转移,或送检盆腔各组淋巴结共?枚未见癌转移)。另送盆腔冲洗液找到癌细胞。
(宫颈、左附件及右输卵管若有特殊病变,也要报)
第81楼:
深染拥挤的细胞团,核深染,立体感,没有偏位的胞浆和蜂窝、羽毛等结构。因此考虑AGC,可能来自子宫内膜。50岁左右的女性,不能放过,要进一步检查。
第97楼,细胞块,HE:
高分化腺癌,可能来自子宫内膜。IHC for ER,PR,P16,CEA,VIM,CK can help.
第116楼,HE:
高分化腺癌,更像来自宫颈管。如此分化好的腺癌不可能是浆液性腺癌。
第118楼,IHC:
CEA- ER- p16+++ VIM-
仍不能肯定来自宫颈或宫腔。因为典型者,来自宫颈应该CEA+ ER- p16+++ VIM-,来自宫腔者应该CEA-/+ ER+ p16+ VIM+

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
-
copy:
浆液性乳头状癌比子宫内膜腺癌具有更强侵袭性,免疫组化结果显示,子宫内膜腺癌及浆液性乳头状癌Vimentin表达阳性率分别为95.45%(21/22例)。0%(0/16例),P53表达阳性率分别为9.09%(2/22例),100%(16/16例),两者P〈0.00。结论:子宫内膜腺癌预后与肿瘤分化程度及肌层侵及深度有关,而浆液性乳头状癌发展快,具有极强侵袭性,早期易发生淋巴管、血管腔和肌层侵犯,预后差,化疗和放了效果均不理想。
A(A) 21:23:50
P16应该是阴性
A(A) 21:24:09
网速慢
A(A) 21:25:45
A(A) 21:23:34
P16应该是阴性
A(A) 21:24:00
内膜癌应该是阳性
A(A) 21:24:08
网速慢
A(A) 21:25:55
网站发不上表情
B 21:26:17
http://www.cnki.com.cn/Article/CJFD2005-BQEB200501045.htm
B 21:28:22
P16是一种重要的抑癌基因,当P16基因突变和丢失时细胞增殖失控使细胞无限制增殖而发生肿瘤。在宫颈上皮内瘤变及癌的发生是以P16阳性表达为特征,这与宫颈上皮内瘤变与宫颈癌是由HPV感染所造成细胞不死性有关
A(A) 21:28:24
A(A) 21:30:17
I型癌发生于较年轻女性,表达ER和PR,通常在内膜增生的基础上发生,预后较好;II型癌发生于较年长的女性,不表达ER和PR,通常发生于萎缩的或静止的内膜,预后较差。组织学上,I型癌相当于内膜样癌,II型癌包括子宫乳头状浆液性癌和透明细胞癌等。分子遗传学上,两型癌显著的不同。I型癌常显示微卫星不稳定性、PTEN和K-ras突变,很少显示p53突变、p16表达缺失和her2/neu表达扩增;相反,II型癌显示高频的p53突变、常有p16表达缺失和her2/neu表达扩增。PTEN突变和MIN被认为是I型癌的早期事件,与癌的进展有关;而p53突变被认为是II型癌发生的早期事件,在II型癌假定的前驱病变中即已发生[1]。
B 21:31:05
目的比较子宫浆液性乳头状癌 ( uterine papillary serous carcinoma, UPSC ) 和子宫内膜样癌 ( uterine endometrioid carcinoma, UEC)的组织病理学和免疫组化表达,以了解两种肿瘤生物学行为的差异。方法对24例UPSC和54例UEC进行组织学复查和应用免疫组化SP法检测肿瘤的p53蛋白、ER和PR的表达。结果24例UPSC占子宫内膜癌的3.77%,平均年龄UPSC组为60岁,UEC组为51.7岁(P〈0.01),晚期癌(FIGO Ⅲ-Ⅳ)UPSC组占62.5%,UEC组占35.1%(P〈0.025)。p53蛋白的表达UPSC组16例阳性(66.7%),UEC组10例阳性(18.5%),两组比较(P〈0.01)。ER阳性表达UPSC组(8.3%),UEC组(42.5%),PR阳性表达UPSC组(12.5%),UEC组(35.2%),两组比较:ER(P〈0.01),PR(P〈0.05),差异有显著性。UPSC组p53蛋白表达与肿瘤分期、分级、及肌层浸润无明显关系,而UEC组Ⅲ-Ⅳ期肿瘤的p53蛋白的表达率高于Ⅰ-Ⅱ期(P〈0.005)。UPSC的5年生存率为25%,UEC组5年生存率为80.9%(P〈0.01),两组差异有显著性。结论UPSC为p53高表达,而缺乏雌激素和孕激素受体,为高度恶性的肿瘤。它的生物学行为不同于UEC,因而强调诊断时需和其他类型的子宫内膜癌相区别。

- “人生没有彩排,每一天都是现场直播”