| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
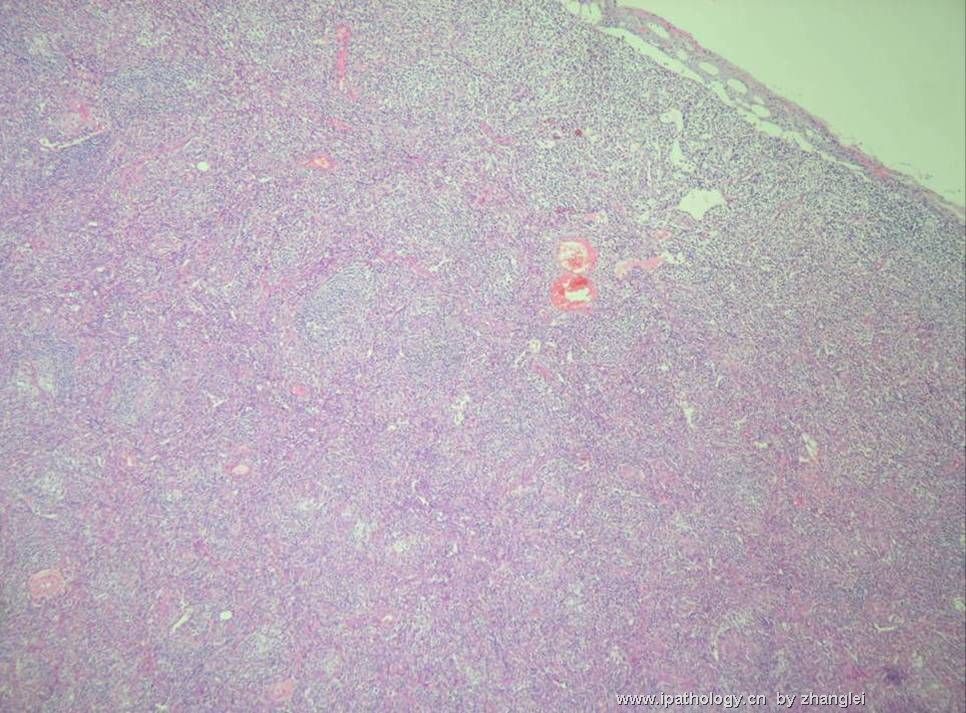
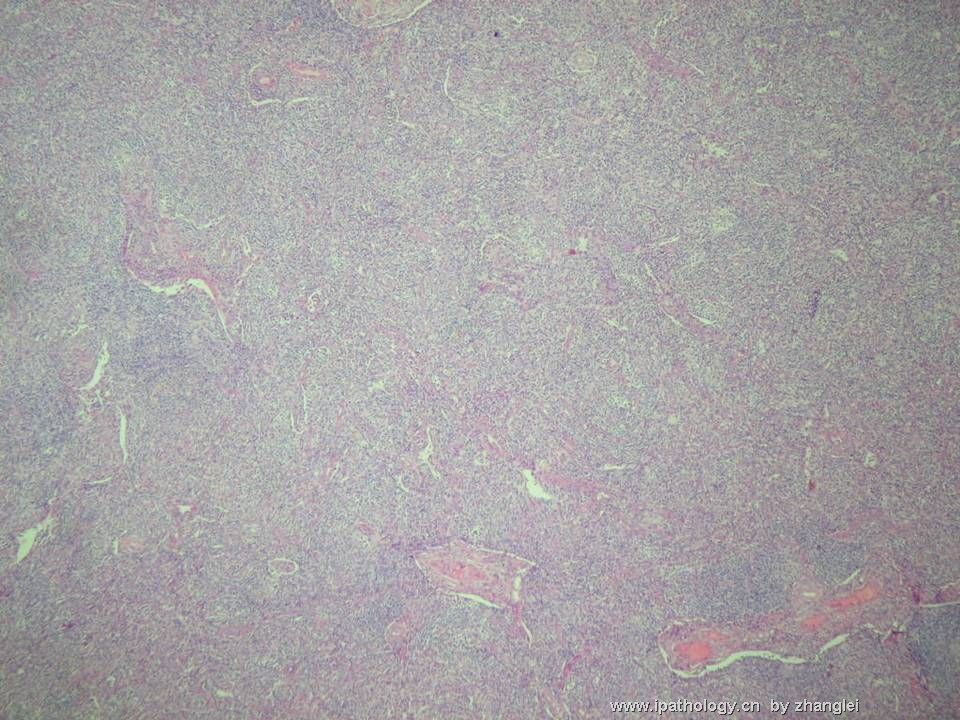
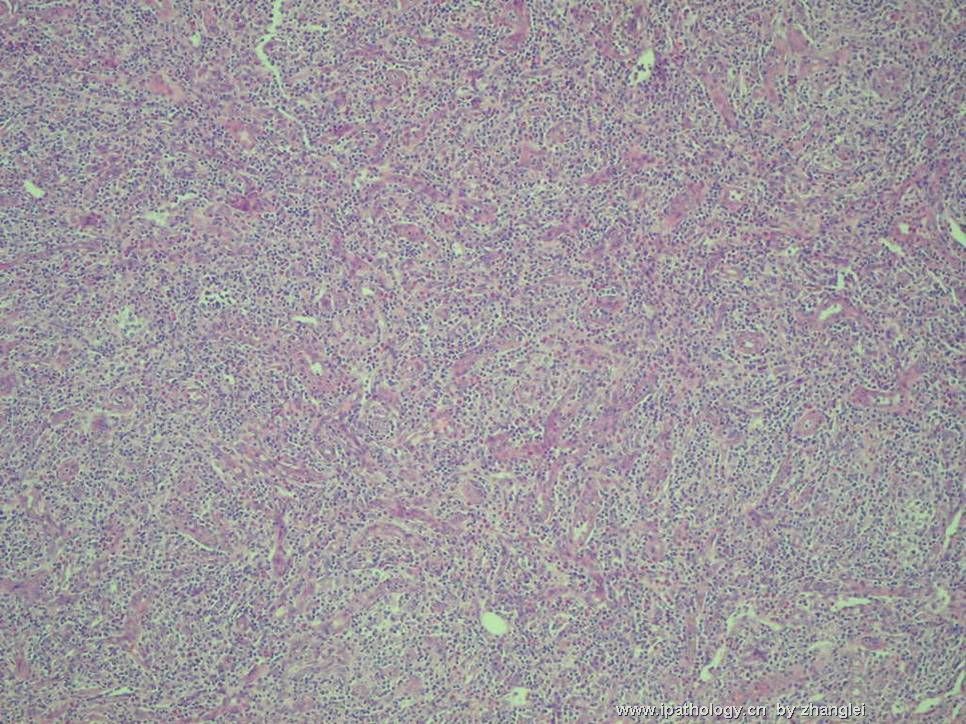
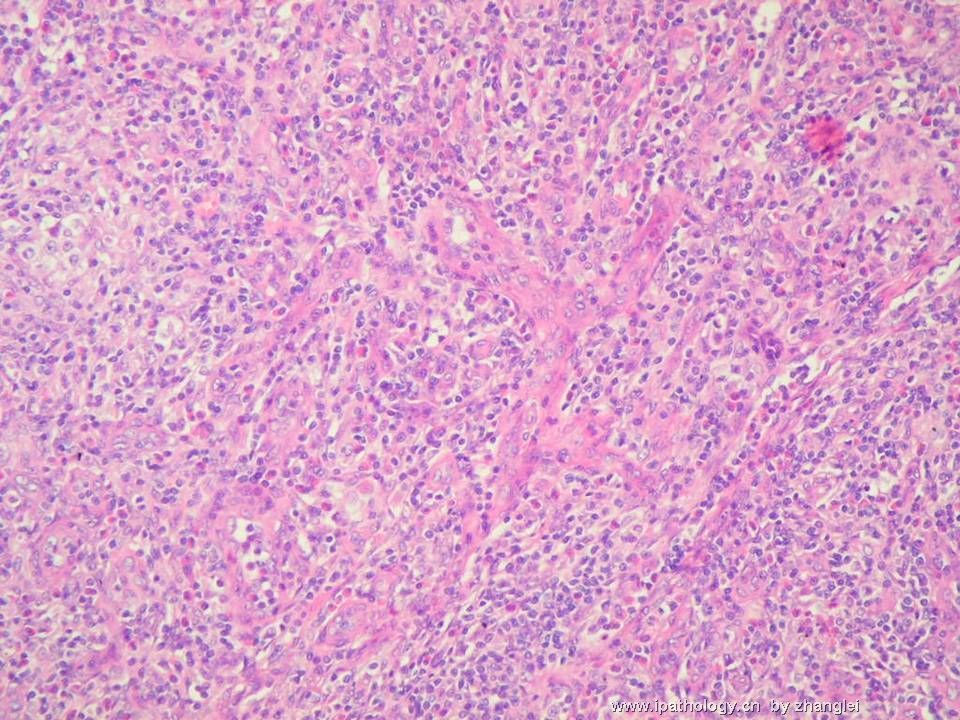
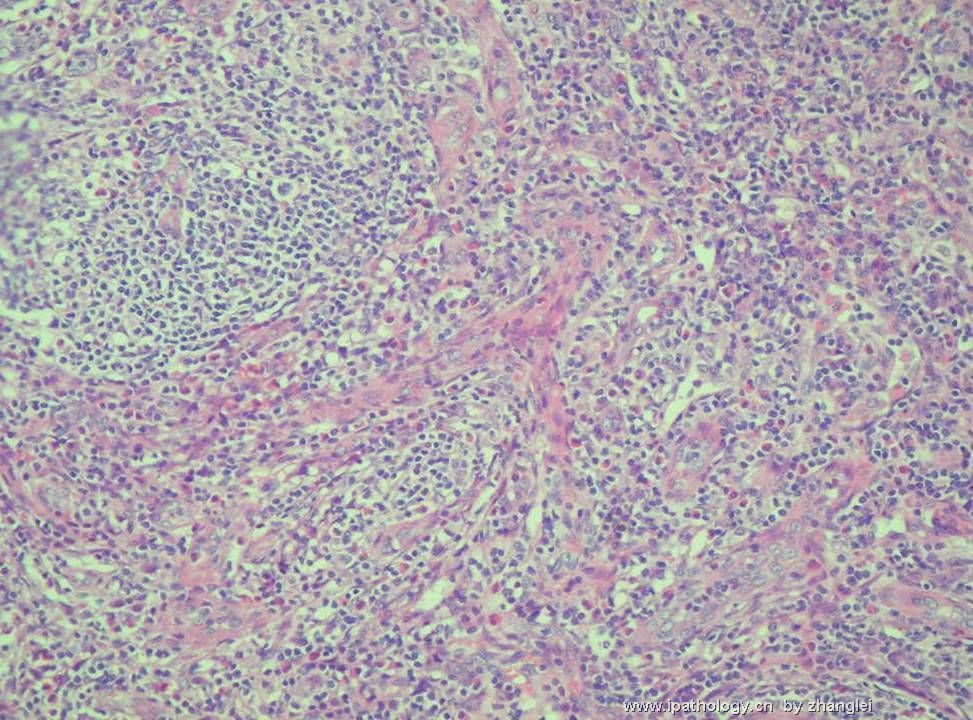
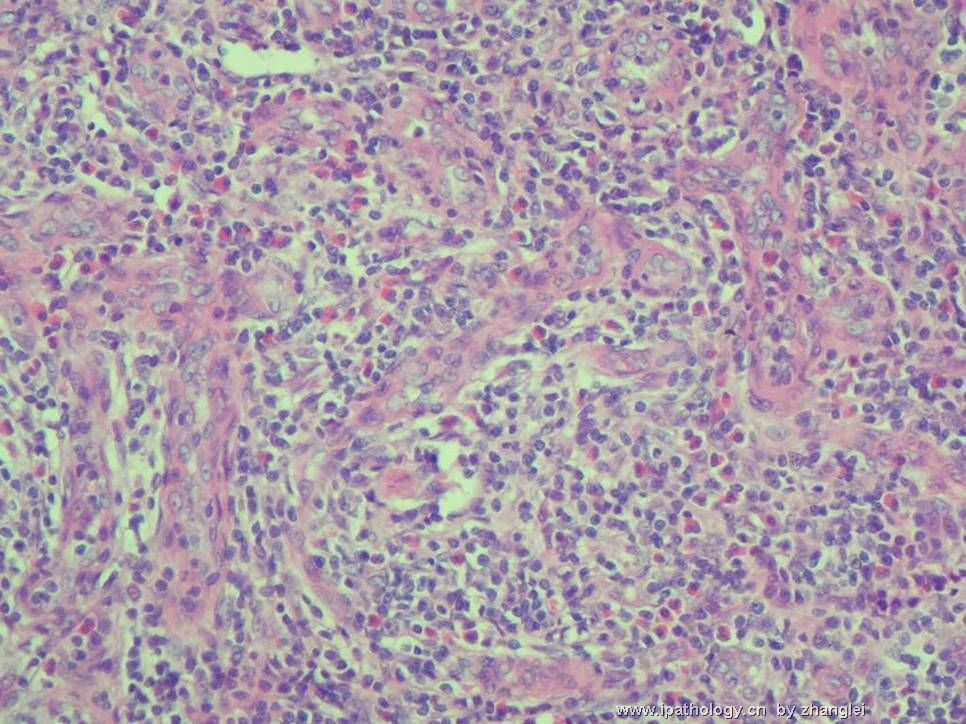
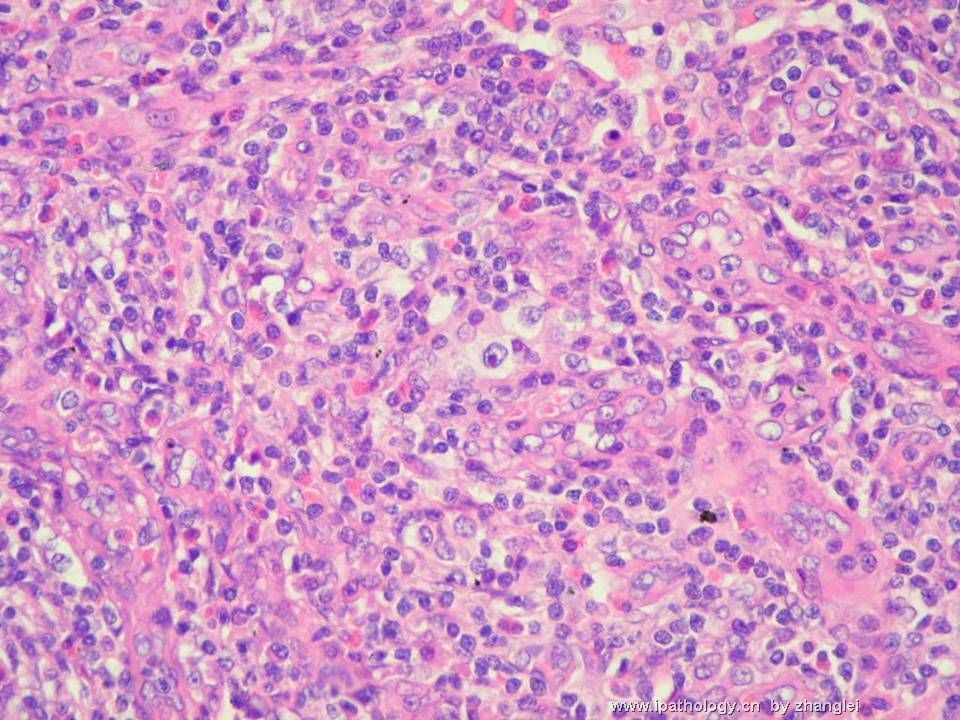
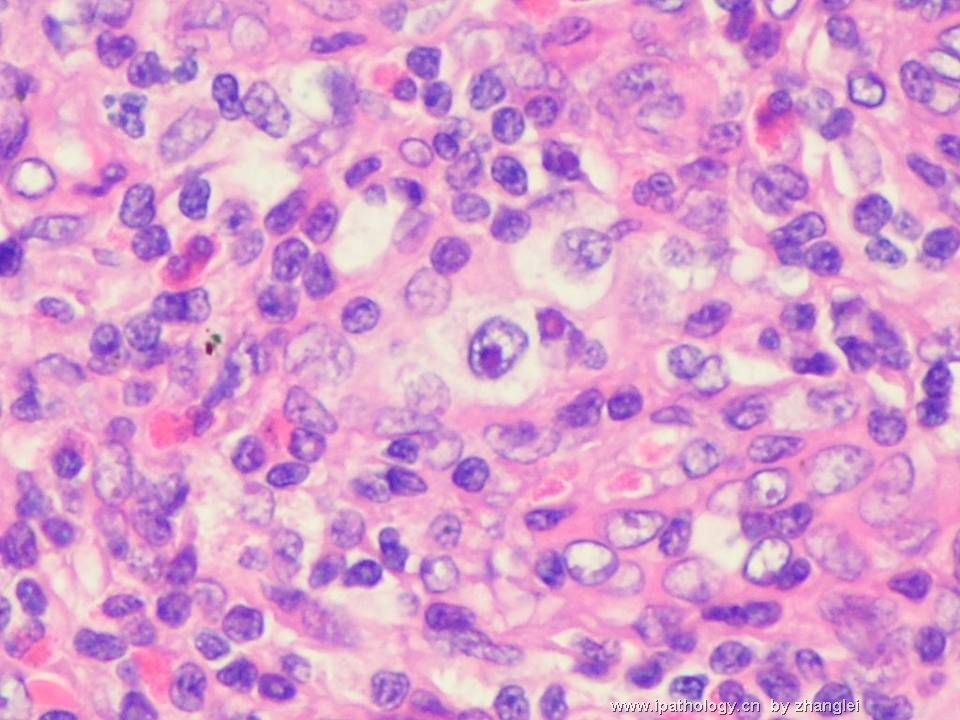
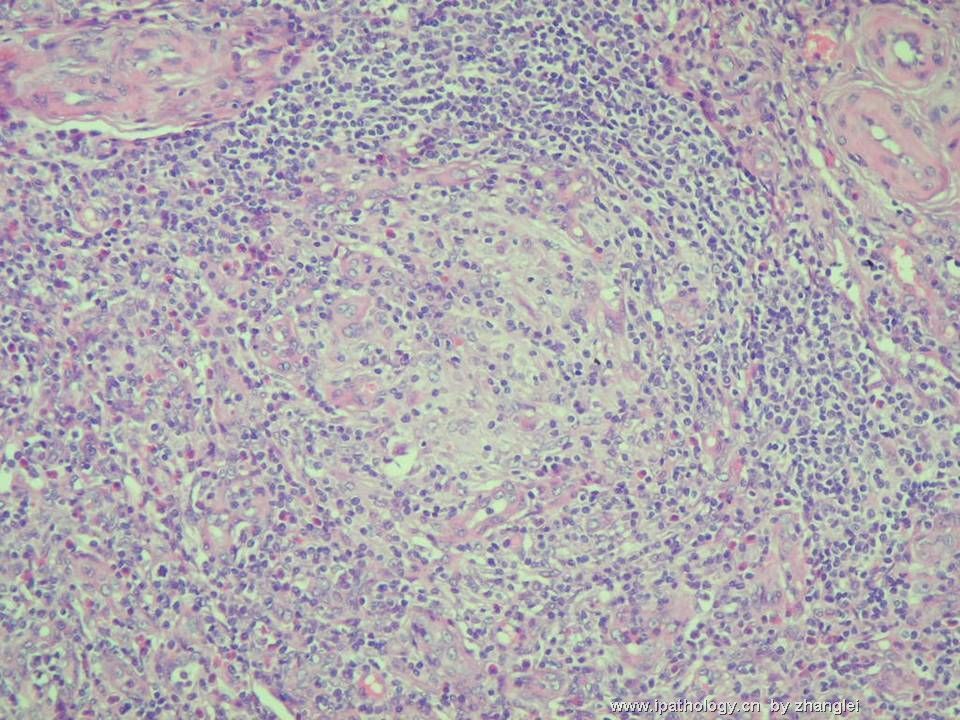
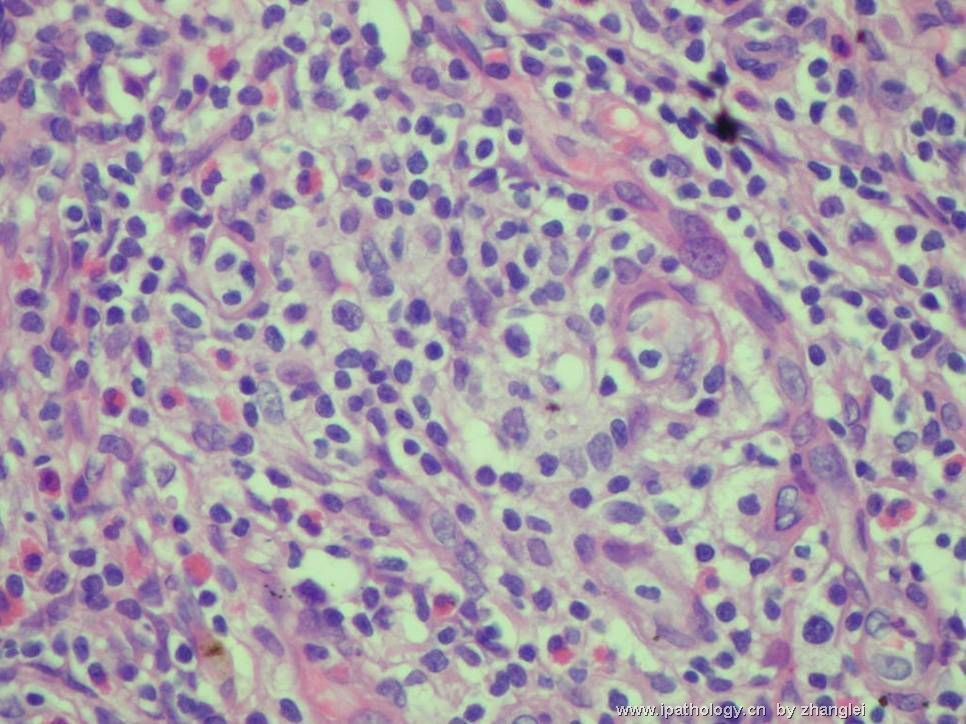
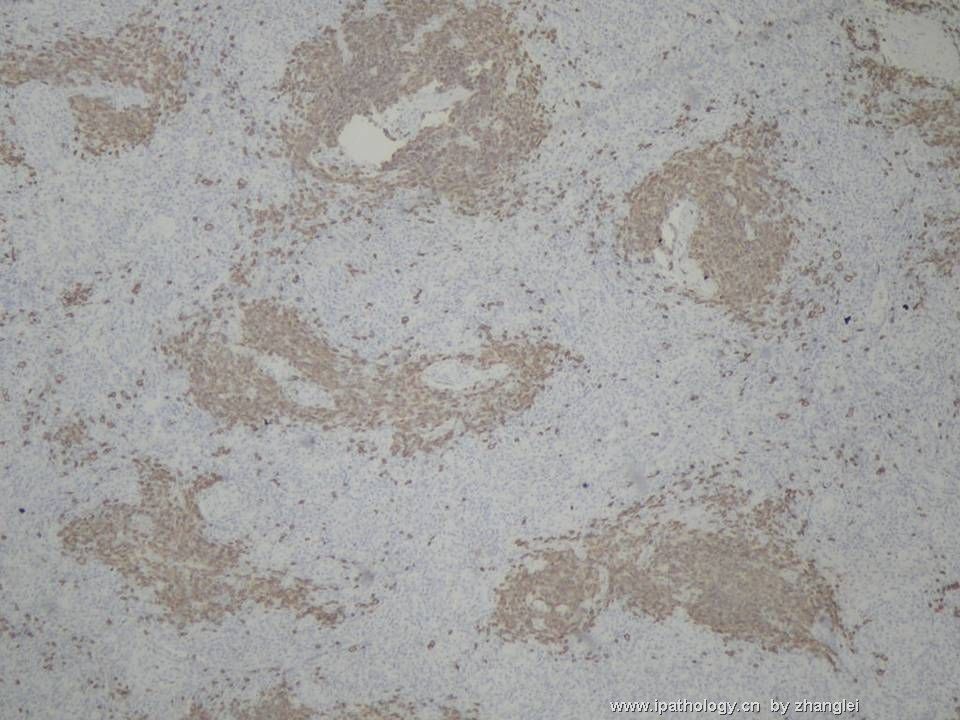
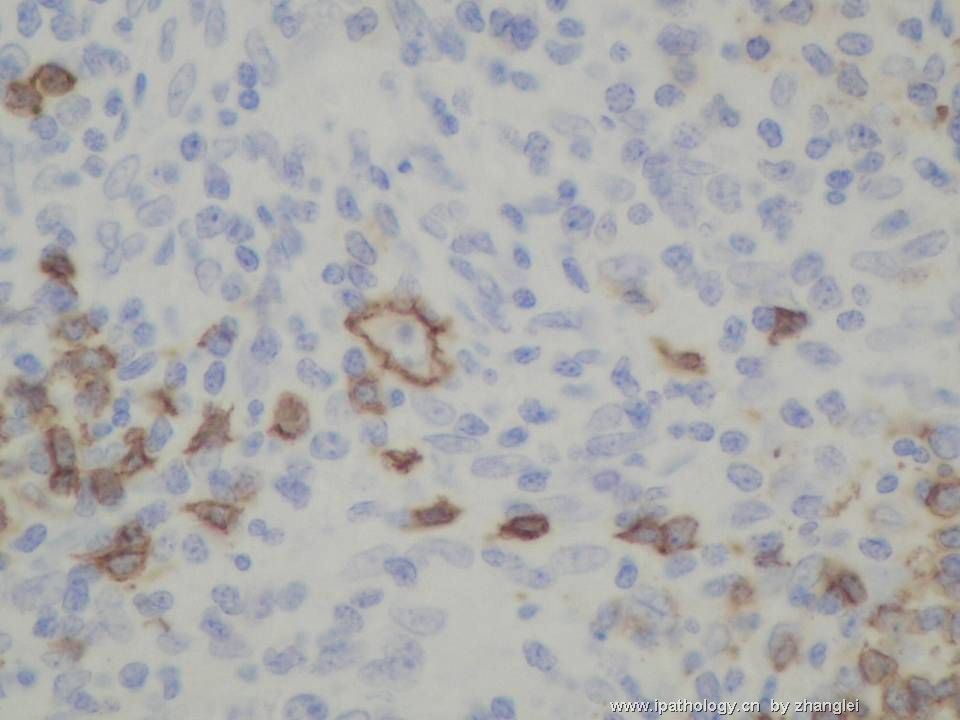
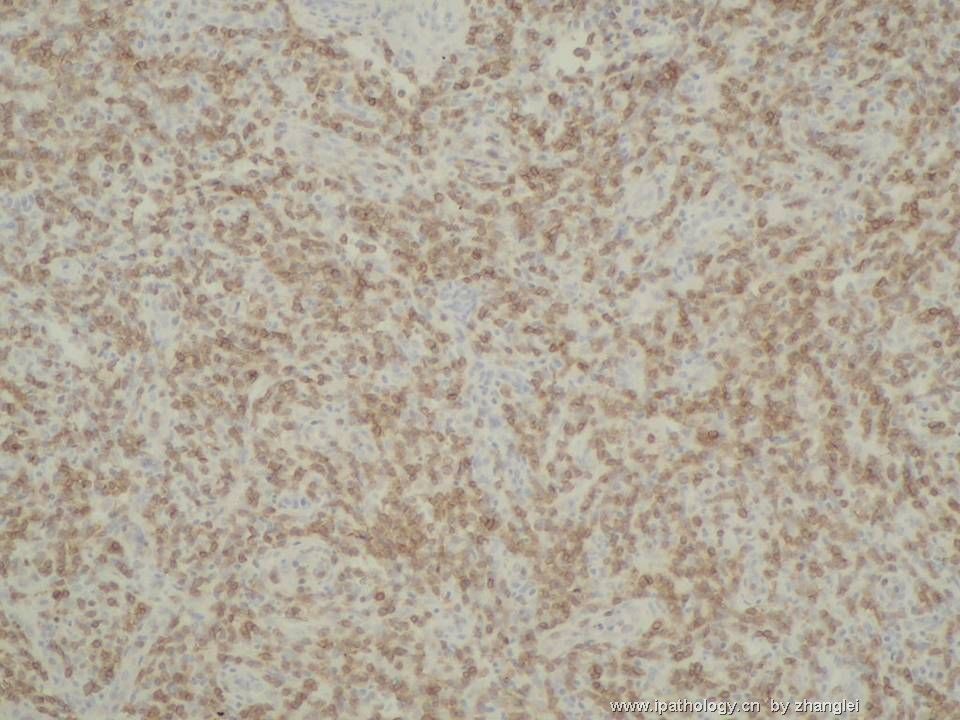
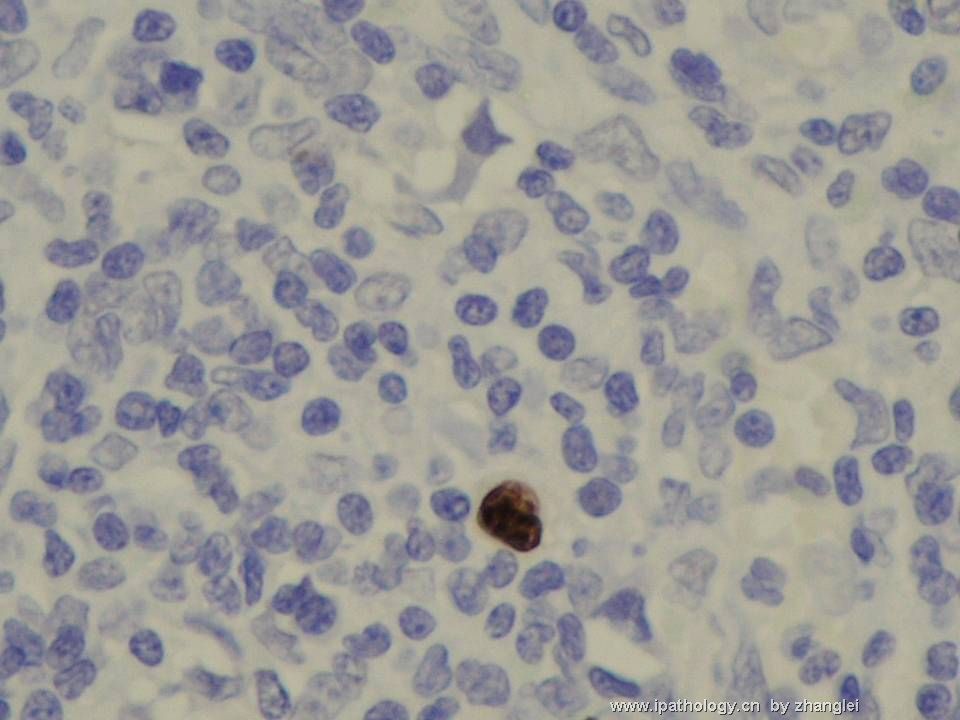
- (转贴)颈部淋巴结--血管免疫母细胞性T细胞淋巴瘤(angioimmunoblastic T cell lymphoma)
| 姓 名: | ××× | 性别: | 男 | 年龄: | 53岁 |
| 标本名称: | 颈部淋巴结 | ||||
| 简要病史: | 间断高烧40余天,住院发现全身淋巴结肿大。 | ||||
| 肉眼检查: | 图11、12--CD20,13--CD3,14、15—CD21,16、17—CD10,18――BCL-6,19---EBER | ||||
名称:图1
描述:图1
名称:图2
描述:图2
名称:图3
描述:图3
名称:图4
描述:图4
名称:图5
描述:图5
名称:图6
描述:图6
名称:图7
描述:图7
名称:图8
描述:图8
名称:图9
描述:图9
名称:图10
描述:图10
名称:图11
描述:图11
名称:图12
描述:图12
名称:图13
描述:图13

名称:图14
描述:图14
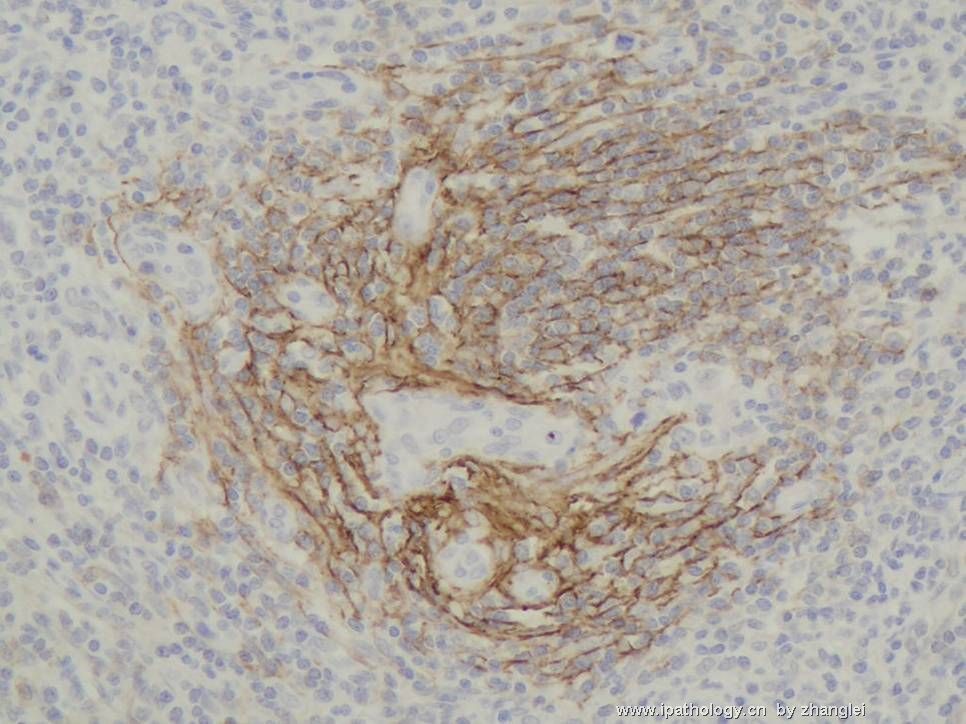
名称:图15
描述:图15
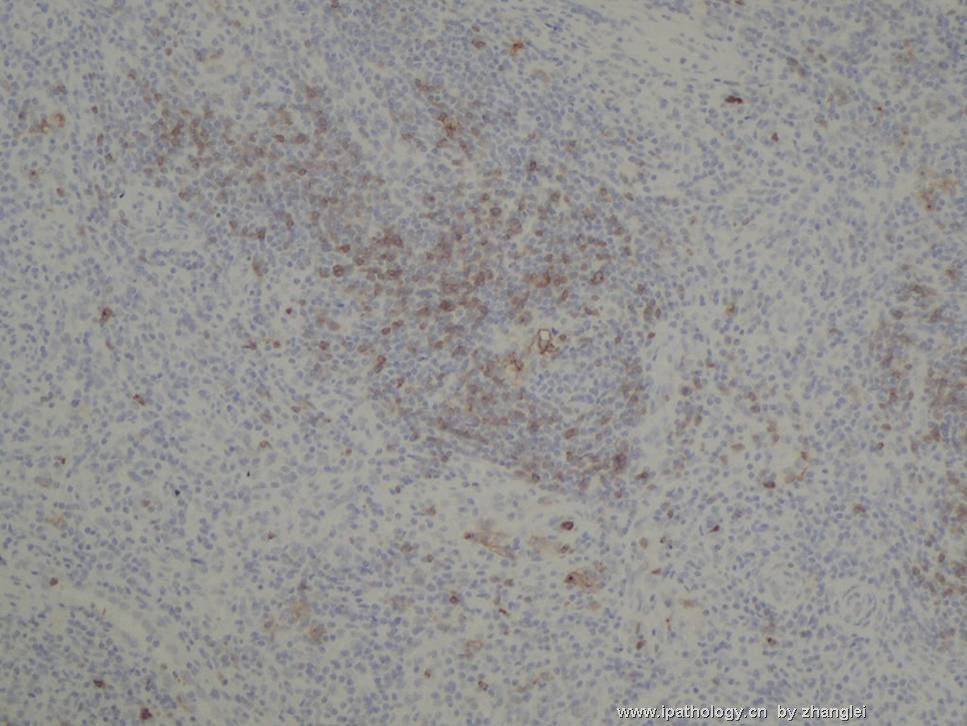
名称:图16
描述:图16
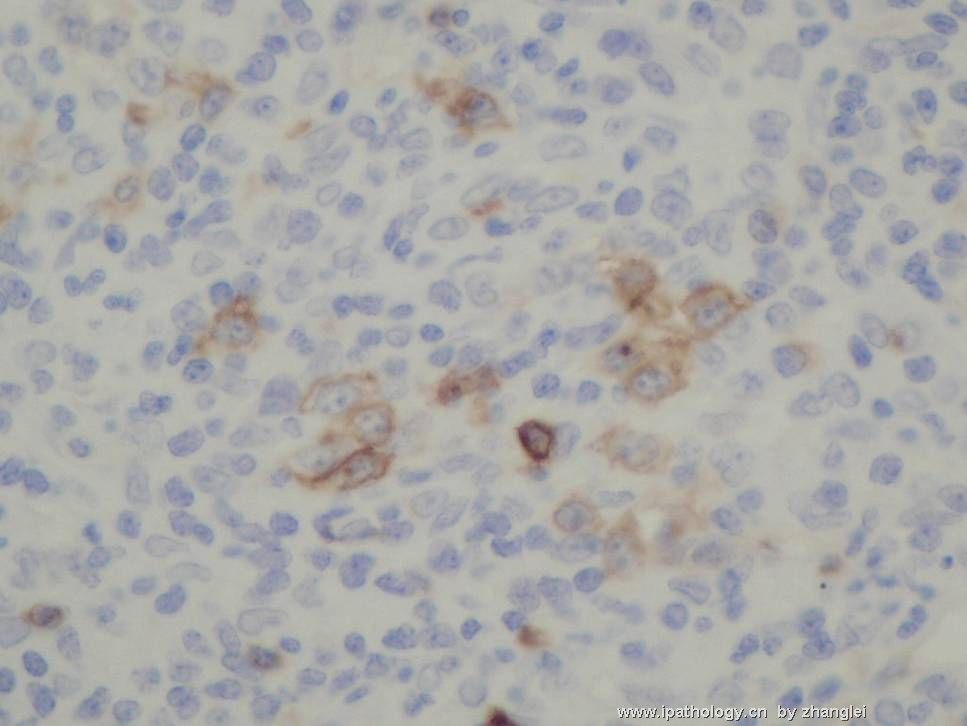
名称:图17
描述:图17
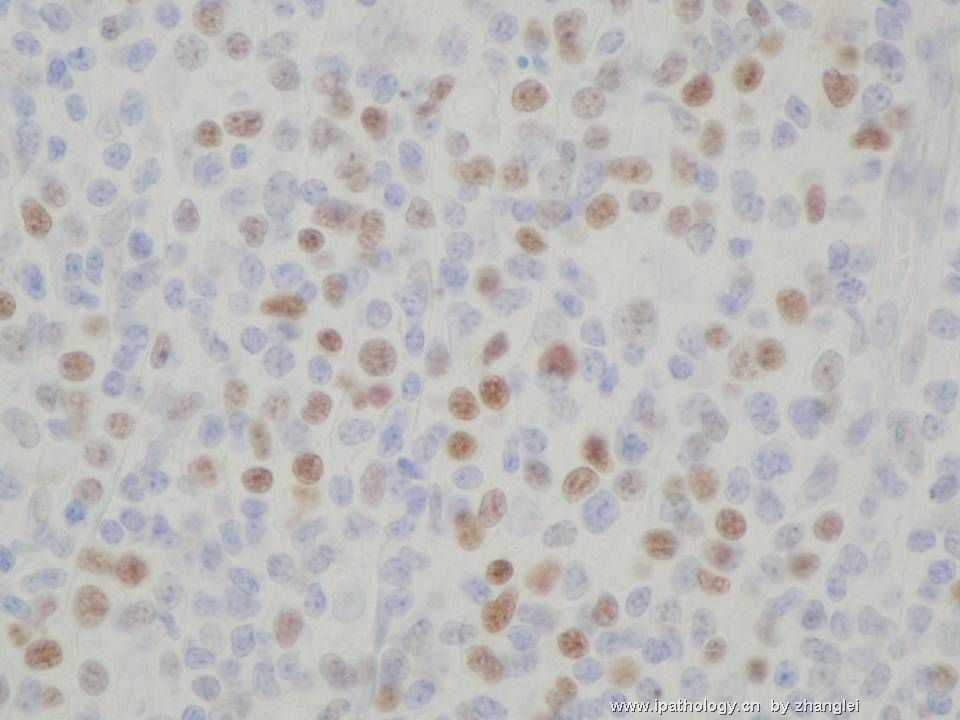
名称:图18
描述:图18
名称:图19
描述:图19
标签:
-
本帖最后由 于 2007-03-13 22:08:00 编辑
×参考诊断
血管免疫母细胞性T细胞淋巴瘤
-
zhongshihua 离线
- 帖子:1608
- 粉蓝豆:0
- 经验:1651
- 注册时间:2006-09-11
- 加关注 | 发消息
-
panzenggang 离线
- 帖子:189
- 粉蓝豆:480
- 经验:246
- 注册时间:2008-01-09
- 加关注 | 发消息