| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B20Breast basal-like carcinoma (cqz 6)
续
7、预后
基底样癌(BBC)是高级别,预后差的乳腺癌。
由于基底样癌为三阴性(ER/PR/Her2),不能用ER和HER2为靶向治疗,主要是化疗。幸运的是新辅助治疗方面的进展发现,ER阴性的乳腺癌疗效甚至比ER阳性的要好,基底样亚型乳腺患者就可以受益。
病理上有完全反应的患者,预后好。基底样乳腺癌预后差的主要因素似乎是残存病灶的远处复发。
8、要记住这种分类和我们以前的分类是两个不同的分类系统。目前在美国,仍然用以前的分类方法,如浸润性导管癌、小叶癌、黏液癌、小管癌等。
对于基底样乳腺癌,我签发为浸润性导管癌,基底样型。
续:
4、发病率:
基底样癌占所有乳腺癌的15%。在年轻的非洲裔美国人发病率偏高,占乳腺癌39%(?)
5、遗传学:
与BRCA1基因突变有关,但应注意大多数基底样乳腺癌是散发性的。
6、与髓样癌(MBC)之间的关系:
一项研究显示MBC属于基底样癌亚型。基底样癌至少可分为两个亚型:MBCs and 基底样 DBCs. (François Bertucci et al Gene Expression Profiling Shows Medullary Breast Cancer Is a Subgroup of Basal Breast Cancers Cancer Research 66, 4636-4644, May 1, 2006).
事实上MBC是非常罕见的,我们现在很少诊断了。在诊断MBC前应仔细考虑。我们每天有大约29例乳腺粗针穿刺活检,15例节段性切除或全切乳腺标本,但最今几年我们几乎没有诊断过MBC。
另外,我认为大多数化生性癌也属于基底样癌亚型。
续:
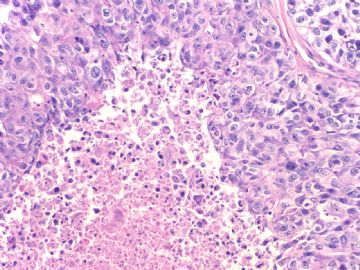
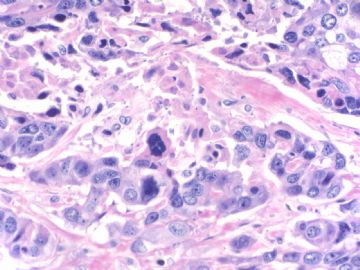
3、典型病理学特征:实性生长方式,高级别的核,显著的淋巴细胞浸润和地图样的坏死。但并不是一定具备上述特怔。
诊断:
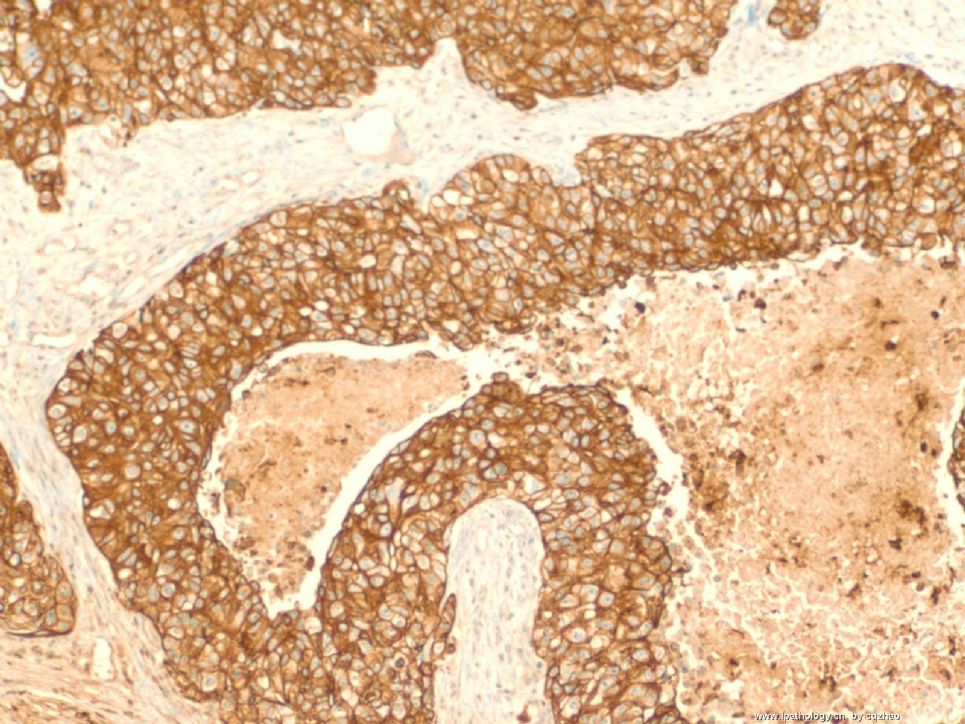
A.免疫组化(ER/PR/Her2) 三阴性。
B.至少有一种基底样标记阳性,CK5/6或 EGFR,或其他基底样标记如CK14, CK17, CD63, 34bE12,我们通常用CK5/6 (or CK5), EGFR, CK14, CK17这一组抗体。有人只用CK5/6 和EGFR。事实上很多病例EGFR阴性或弱阳性。我的同事Dr. Bhargava证实
CK5是最敏感的抗体(Am J Clin Pathol. 2008 Nov;130(5):724-30)。我们通常对所有浸润性乳腺癌都做ER/PR/Her2 ,如果是三阴性,再做基底细胞样免疫标记。
cqzhao 老师的回复:
看来你们很多人对这一类型的乳腺癌都有认识。我复习了一些文献,摘录了一些要点,供大家参考。
1、概念的来源:
用cDNA微阵列技术发现不同类型的乳腺癌,根据534个内源性基因的表达方式,乳腺癌可分为5个亚型:腺腔型A、腺腔型B、基底样型、Her2过表达型和正常乳腺样型。有兴趣的话,可看看以下文献:
2、免疫组化染色和基因微阵列之间的关系:根据肿瘤表达ER 和 Her2的情况。
肿瘤细胞表达ER者可分为:腺腔型A和腺腔型B两个亚型
肿瘤细胞不表达ER者可分为:基底样亚型、HER2过表达亚型、正常乳腺样亚型。
五个亚型概括为:
腺腔型A:ER+/Her2+
腺腔型B:ER+/Her2-
基底样型:ER-/Her2-
HER2过表达型:ER-/Her2+
正常乳腺样型:ER- ...?
| 以下是引用cqzhao在2008-12-7 4:55:00的发言:
Continue: 3. Typical Pathologic features: solid growth pattern, high nuclear grade, presence of marked lymphocytic infiltrate, and geographic necrosis. It is not necessary they must have above features.
Diagnosis: A. Triple negative. B: At least one of basal-like markers is positive, CK5/6 or EGFR, or other basal-like marker CK14, CK17, CD63, 34bE12, We generally use CK5/6 (or CK5), EGFR, CK14, CK17 as a panel. Some use only CK5/6 and EGFR. In fact a lot of cases show EGFR negative or weakly positive. My colleague, Dr. Bhargava demonstrated CK5 is the most sensitive marker (Am J Clin Pathol. 2008 Nov;130(5):724-30). We do ER/PR/Her2 for all invasive tumors. If triple negative, then basal-like markers will be done for all cases. |
Happy to see some study about basa-like ca in China
Hum Pathol. 2008 Feb;39(2):167-74. Epub 2007 Nov 28.
Basal-HER2 phenotype shows poorer survival than basal-like phenotype in hormone receptor-negative invasive breast cancers.
Liu H, Fan Q, Zhang Z, Li X, Yu H, Meng F.
Department of Pathology,
:Zhonghua Bing Li Xue Za Zhi. 2008 Feb;37(2):83-7.
[Morphological features of basal-like subtype invasive carcinoma of breast]
[Article in Chinese]
Gao LX, Yang GZ, Ding HY, Li L.
: Zhonghua Bing Li Xue Za Zhi. 2008 Feb;37(2):83-7.
[Morphological features of basal-like subtype invasive carcinoma of breast]
[Article in Chinese]
Gao LX, Yang GZ, Ding HY, Li L.
Department of Pathology, the General Hospital of Beijing Military Command,
continue.
7. Prognosis
Basal-like breast carcinoma (BBC) associated with high grade, poor prognosis.
Given the triple-negative status of basal-like breast cancer, it cannot be treated with ER-targeted or HER2-targeted therapies, so is primarily treated with chemotherapy. Fortunately, advances in adjuvant therapy appear to benefit ER-negative breast cancer even more than ER-positive breast cancer, and women with the basal-like subtype have similarly benefited.
The women with pathologic complete response have good outcome; the poor prognosis of basal-like breast cancer appears to relate to a particularly high risk of early distant relapse among those that had residual disease.
8.
Remember the classification and our previous classification are two different systems. In the
For the basal-like breast carcinoma like my case, I sign out as invasive ductal carcinoma, basal-like phenotype.
Continue:
4. Rate:
Accounting for about 15% of all breast carcinoma. It over-presented in young African American women who developed breast ca, comprising 39 of breast ca.
5. Genetic:
Related to BRCA1 mutation, but be aware that most basal-like ca patients are sporadic.
6.
Relation to medullary carcinoma (MBC): One study shows that MBC belongs to the basal molecular subtype. Basal subtype can be subdivided in at least two subgroups: MBCs and basal DBCs. (François Bertucci et al Gene Expression Profiling Shows Medullary Breast Cancer Is a Subgroup of Basal Breast Cancers Cancer Research 66, 4636-4644, May 1, 2006). In fact MBC is very rare. We seldom make this dx now. Please think over before you want to disgnose MBC. The clinician will think the patient has a good tumor. Every day we have about 20 breast core biopsies and about 15 breast segmental or total mastectomies, We almost never diagnose MBC in recent years. In addition, I think most metaplastic carcinoma may belong to the group of basal-like ca also.
Relation to medullary carcinoma (MBC):
One study shows that MBC belongs to the basal molecular subtype. Basal subtype can be subdivided in at least two subgroups: MBCs and basal DBCs. (François Bertucci et al Gene Expression Profiling Shows Medullary Breast Cancer Is a Subgroup of Basal Breast Cancers Cancer Research 66, 4636-4644, May 1, 2006).
In fact MBC is very rare. We seldom make this dx now. Please think over before you want to disgnose MBC. The clinician will think the patient has a good tumor. Every day we have about 20 breast core biopsies and about 15 breast segmental or total mastectomies, We almost never diagnose MBC in recent years.
In addition, I think most metaplastic carcinoma may belong to the group of basal-like ca also.
Continue:
3. Typical Pathologic features: solid growth pattern, high nuclear grade, presence of marked lymphocytic infiltrate, and geographic necrosis. It is not necessary they must have above features.
Diagnosis:
A. Triple negative.
B: At least one of basal-like markers is positive, CK5/6 or EGFR, or other basal-like marker CK14, CK17, CD63, 34bE12, We generally use CK5/6 (or CK5), EGFR, CK14, CK17 as a panel. Some use only CK5/6 and EGFR. In fact a lot of cases show EGFR negative or weakly positive. My colleague, Dr. Bhargava demonstrated CK5 is the most sensitive marker (Am J Clin Pathol. 2008 Nov;130(5):724-30).
We do ER/PR/Her2 for all invasive tumors. If triple negative, then basal-like markers will be done for all cases.
Seem many of you know this entity well. I almost finished my preparation to our fellows next week. I reviewed some papers and summaried the main points here for your reference.
1. The origin of the terminology
Gene expression analyses with cDNA microarray technology identified distinct groups of breast cancers. Based on the patterns of expression of 534 intrinsic genes, the breast carcinoma were sub-classified in to 5 groups, Luminal A, Luminal B, Basal-like, Her2 over-expression, and normal breast-like.
Open to see the original papers in 2001, 2003 if you are really interested
http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=166244&blobtype=pdf
http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=58566&blobtype=pdf
2. The relation between IHC stains and microarray gene classification: tumors by ER and Her2:
Tumors with ER expression could be divided into two groups “luminal A” and “luminal B” and no ER expression could be divided into three subgroups: "basal-like" subtype, HER2-positive subtype, and "normal breast-like".
So total five subgroups:
Luminal A: ER+/Her2+
Luminal B: ER+/Her2-
Basal-like: ER-/Her2-
Her2 over expression: ER-/Her2+
-
本帖最后由 于 2008-12-05 08:59:00 编辑
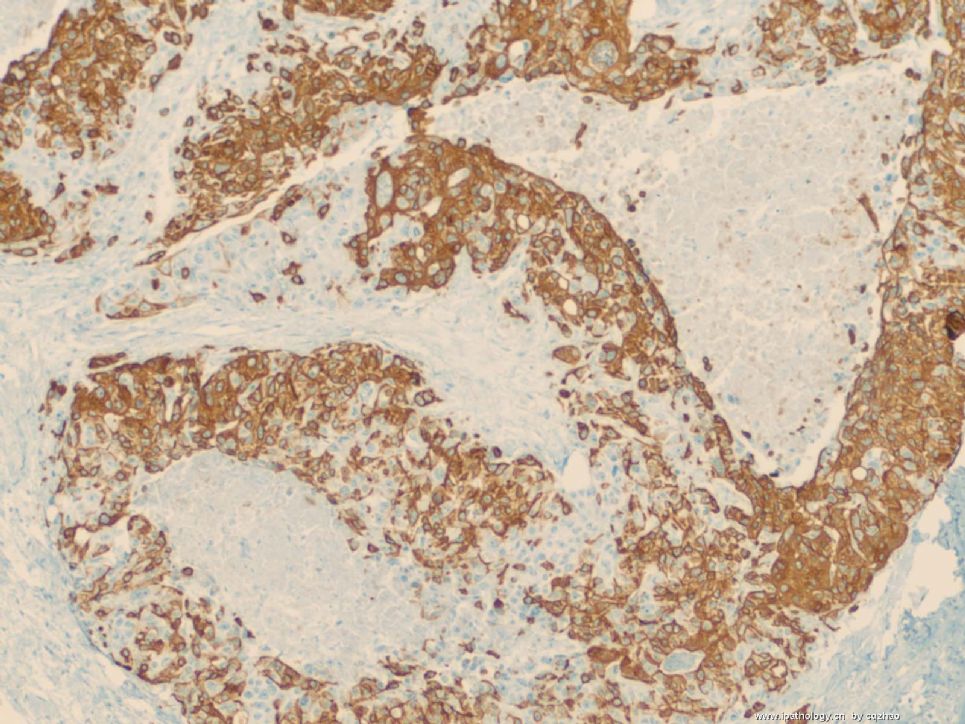
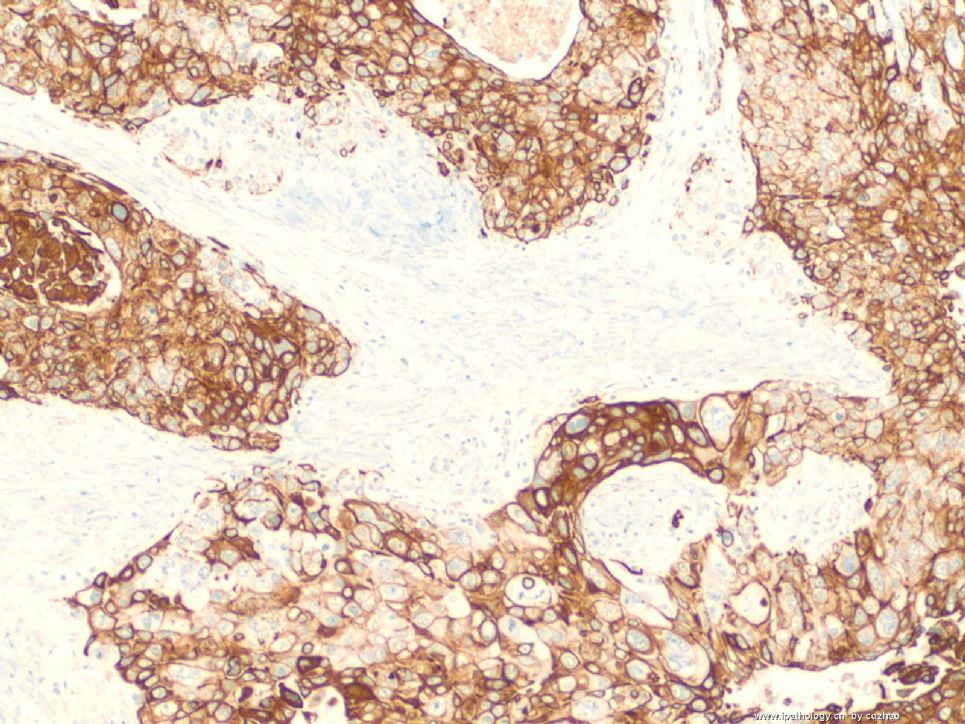
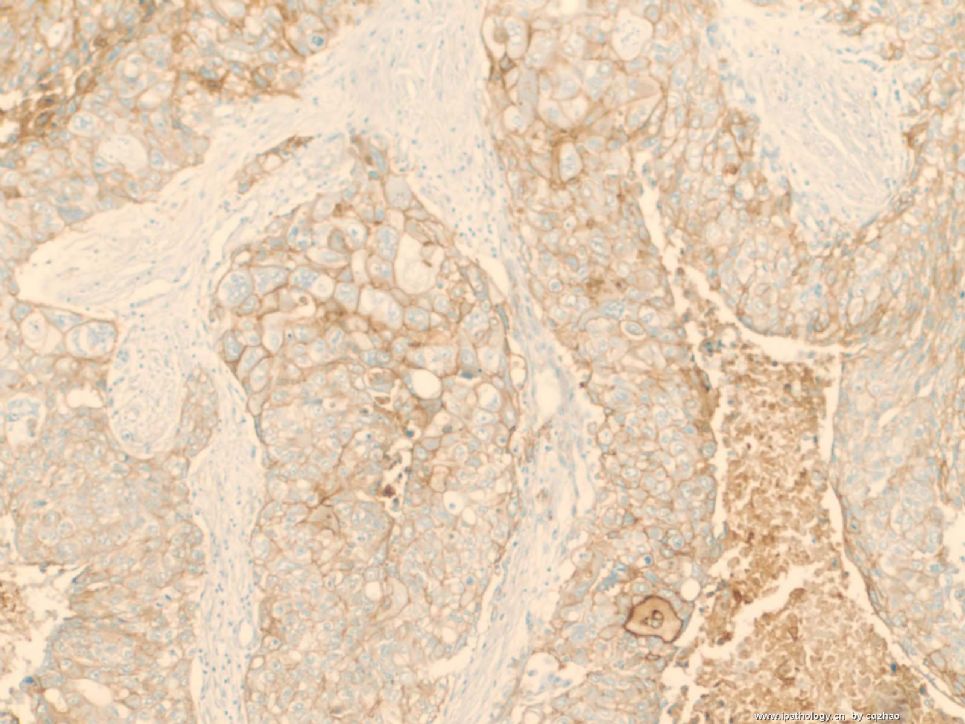
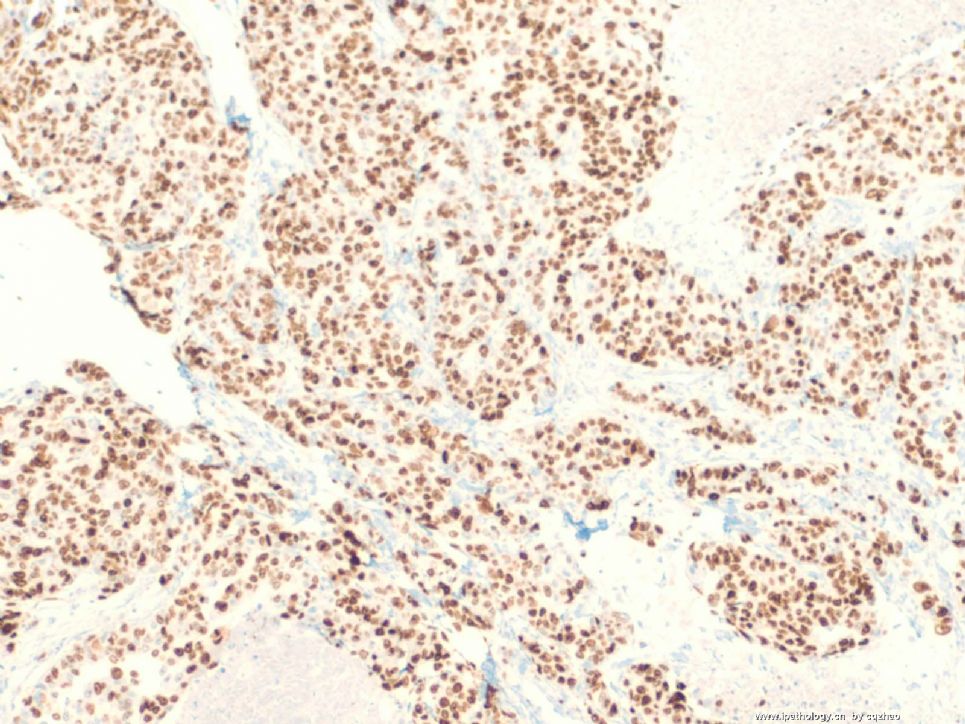
IHC results
F1 ck5
F2 ck14
F3 ck17
F4 EGFR
F5 Ki67
Hope every one can make your dx. please write down u questions or have some discussion. I will have a relatively detailed discussion here sometimes next week. Now I need to prepare a formal powerpoint presentation to our fellows and residents next week.
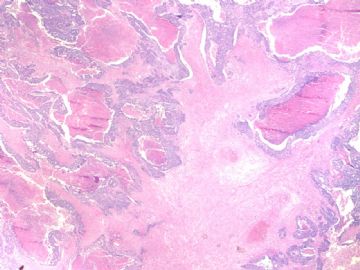
名称:图1
描述:图1
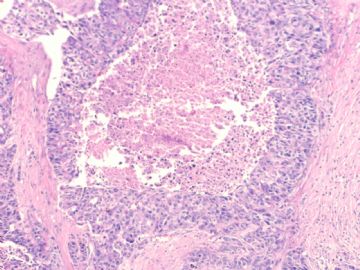
名称:图2
描述:图2
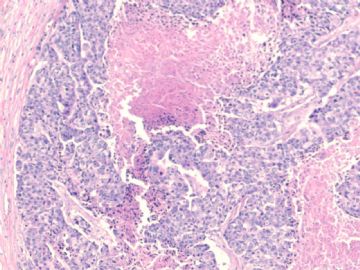
名称:图3
描述:图3
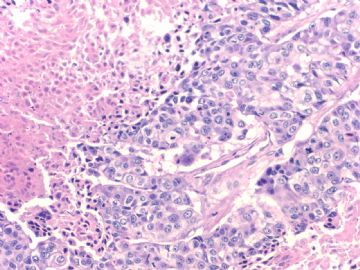
名称:图4
描述:图4
名称:图5
描述:图5
-
文献记载 乳腺基底细胞样癌形态学特征
• 膨胀性生长方式,推挤性边缘
• 周边多量淋巴细胞浸润
• 肿瘤中央出现无结构的纤维瘢痕,往往还伴有地图样坏死
• 肿瘤细胞多呈合体状,界限不清,胞质不丰富
• 核分裂象多见,常>20个/10HPF
• 肿瘤组织常出现梭形细胞、透明细胞、基底细胞样或鳞状细胞化生
IHC表型
ER、PR和HER2(-)
CK5/6、CK14(+)
EGFR常(+)
但不知道只有免疫表型而无形态学特征者是否可以诊断
期待赵老师讲解


Saw you above response. Can you make the final dx based on morphology and IHC results I showed you?
I hope every one can write down your dx and reasons. I am interested in knowing your thinking. Then I know what I should discuss. Internet is good. You can write what you want to and you do not have any responsibility. I do not know any one of you. It is a free stage for every one.
Anyway I will discuss this topic in details later.