| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B20Breast basal-like carcinoma (cqz 6)
-
Am J Surg Pathol. 2009 Apr 22. [Epub ahead of print]
-
Basal Cytokeratin and Epidermal Growth Factor Receptor Expression Are Not Predictive of BRCA1 Mutation Status in Women With Triple-negative Breast Cancers.
*Department of Pathology, Beth Israel Deaconess Medical Center daggerDepartment of Pathology, Brigham and Women's Hospital and Harvard Medical School parallelDepartments of Medical Oncology and Cancer Biology, Dana-Farber Cancer Institute, Boston, MA double daggerKlinik für Gynäkologie und Gynäkologische Onkologie, Dr Horst Schmidt Klinik, Wiesbaden, Germany section signDivision of Medical Oncology, Memorial Sloan-Kettering Cancer Center, New York, NY.
BACKGROUND: Over 80% of breast cancers in women with germline BRCA1 mutations are estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2-negative ("triple negative") and most of these have a basal-like phenotype by expression profiling and immunophenotypic analysis. However, whether or not expression of biomarkers characteristic of basal-like breast cancers helps to define a subset of women with triple-negative breast cancers who are likely to harbor BRCA1 mutations is an unresolved issue. METHODS: We randomly identified 165 women from the Dana-Farber/Harvard Cancer Center SPORE annotated specimen bank with primary invasive, triple-negative breast cancers. Tissue microarrays were constructed by obtaining triplicate 0.6 mm cores from available paraffin blocks from 130 cases: only unstained slides were available for immunostaining from 35 cases. Slides cut from the tissue microarrays and the unstained slides were immunostained for estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 (to confirm triple-negative status) and for several markers that have been reported to be useful in defining the basal-like phenotype, including basal cytokeratins CK5/6, CK14, and CK17 and epidermal growth factor receptor (EGFR). Full sequencing analysis for BRCA1 germline mutations was performed on blood specimens from all cases. The final study population consisted of 144 cases in which (1) triple-negative status was confirmed; (2) there was sufficient material for analysis of basal cytokeratins and EGFR; and (3) germline BRCA1 mutation status was known. RESULTS: Among these triple-negative breast cancer cases, 97 (67%) expressed one or more basal cytokeratins and 102 (71%) showed EGFR expression. Basal cytokeratin expression was detected in 65% of the tumor from the 20 BRCA1 mutation carriers and in 68% of the cancers from women without mutations (P=NS). EGFR expression was identified in a similar proportion of tumors from women with and without BRCA1 mutations (75% vs. 72%, P=NS). CONCLUSIONS: Basal cytokeratin and EGFR expression are both highly prevalent among triple-negative breast cancers. The frequency of expression of basal cytokeratins and EGFR was similar in women with and without BRCA1 mutations. Therefore, although the expression of basal cytokeratins and/or EGFR can be used to identify triple-negative breast cancers that have a basal-like phenotype, expression of these markers alone is not sufficient to distinguish which women with triple-negative breast cancers are likely to harbor BRCA1 germline mutations.
-
本帖最后由 于 2009-03-03 01:47:00 编辑
You know all sugjects. I only know some breast/gyn/cyto and no others. So you are more valuable.
In fact pathologists need to sign out all even in most hospitals in the US. Only in few very large academic centers, pathologists sign out for their own subspecielties.
Thank for teaching me the word. No I know a new chinese word.
Agree that pathologists 要广泛地学习,仔细地询问,缜密地思考,明确地分辨,踏踏实实地实践.
You pick a name which is consistent with your personality.
| 以下是引用kint123在2009-2-7 22:32:00的发言:
也就是说仅用于癌或非癌的鉴别诊断问题? 今天看了一篇有关“gene-expression profiling”的review,感觉世界发展太快了,有的东西国内跟不上 |
-
本帖最后由 于 2009-02-03 21:30:00 编辑
| 以下是引用kint123在2009-2-2 7:38:00的发言:
非常感谢赵教授,我还有两个问题: 1、对于正常乳腺型,在免疫组化检查中,有什么特殊的吗?与Null型(negative for all the markers)有多少关系? 2、曾有人将腺腔型分为三个亚型,对于其中的C型,并没有仔细的阐述,只是提到在6种分型中,预后最差,这个C型又怎么诊断? 这些问题在看文献时都找不到明显答案,还请赐教,谢谢 |
Just call me Dr. Zhao or Zhao.
You may know more than I know in this topic.
One thing should keep in mind. There are two different classifications, gene profile and IHC. Recent studies stated that 正常乳腺型 is not present.
2. The 2000 paper mentioned 3 luminal types, A, B, C. The same group of researchers had another paper in 2003 mentioned the luminal C may not be present. Until you are doing the study in gene profile, the gene profile classification is not very useful in clinic now. We only use the term basal-like ca. If cases with triple negative and some basal markers positive, we diagnose invasive ductal carcinoma with basal-like phenotype. The clinical treatment is the same for the cases with or without basal-like pheonotype. The oncologists care the results of ER, PR, her2/neu.
Now a california company, Genomic Health can use tissue block to do RT-PCR for expression of 21 genes (including er. pr, her2), called Onco type DX.
Oncotype DX analyzes a panel of 21 genes within a tumor to determine a Recurrence Score. The Recurrence Score is a number between 0 and 100 that corresponds to a specific likelihood of breast cancer recurrence within 10 years of the initial diagnosis. With this information, it may be possible for doctors and patients to make more informed decisions about breast cancer treatment options.
A lot of breast oncologists like the methods. In fact it is not better than simple ER/PR/Her2 IHC. One test needs more than 2000 dollors. The company earns a lot of money. Now few people care the cost of treatment.
From your questions I can tell you read a lot of papers already. I am trying to answer your quesions by my impression. I never did research on this topic. So they can be wrong.
1. There are four possibilities: ER+/PR+, ER+/PR-, ER-/PR-, ER-/PR+. The cases with ER-/PR+ are rare, but they can be present. We use triple negative.
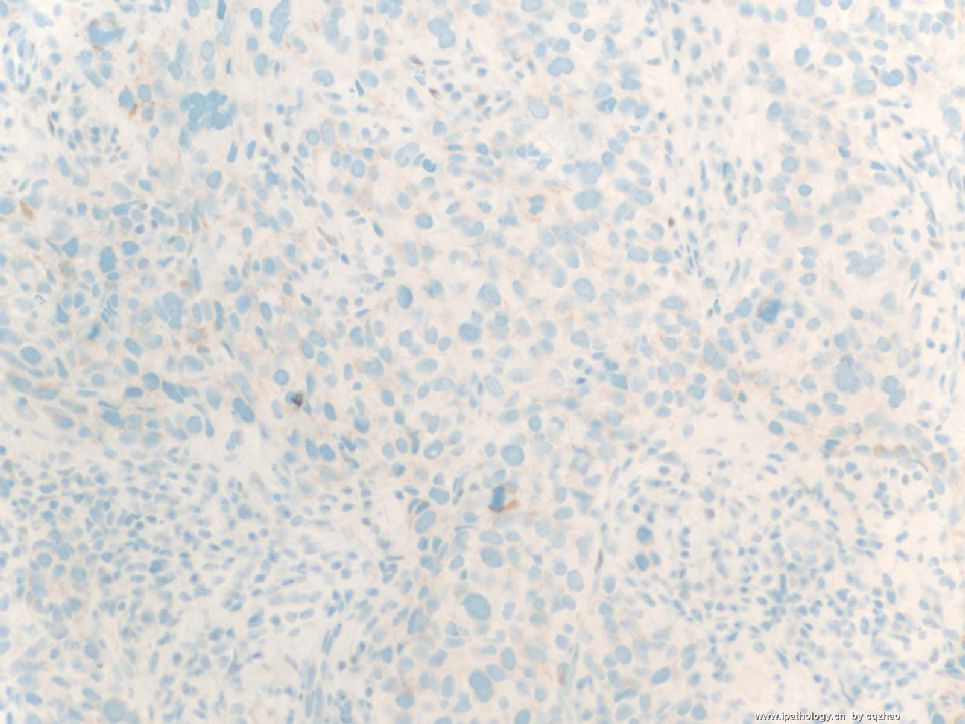
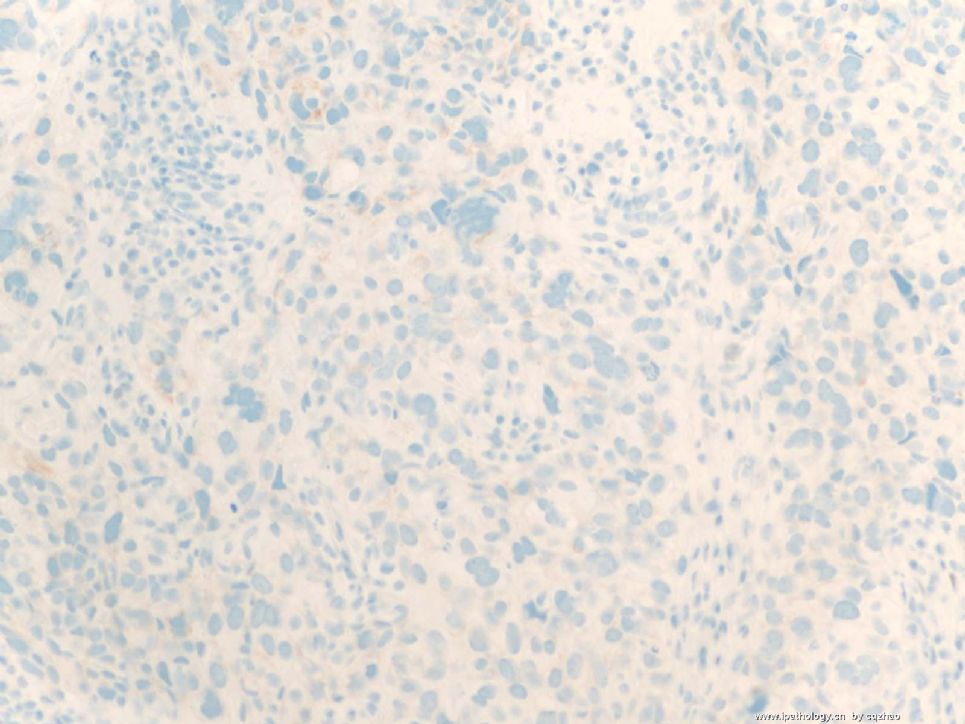
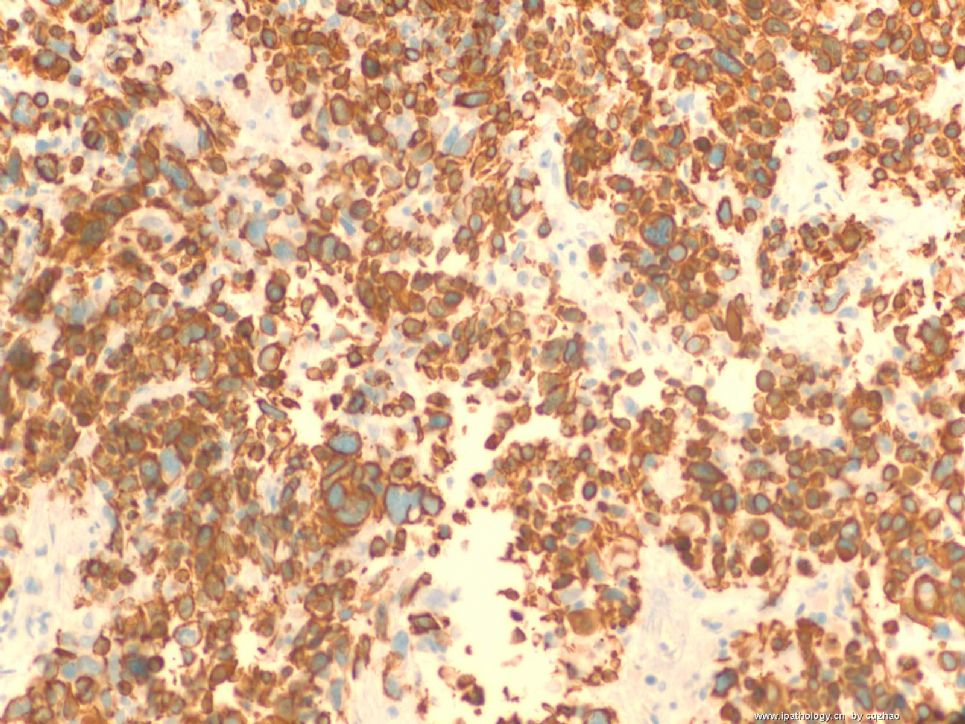
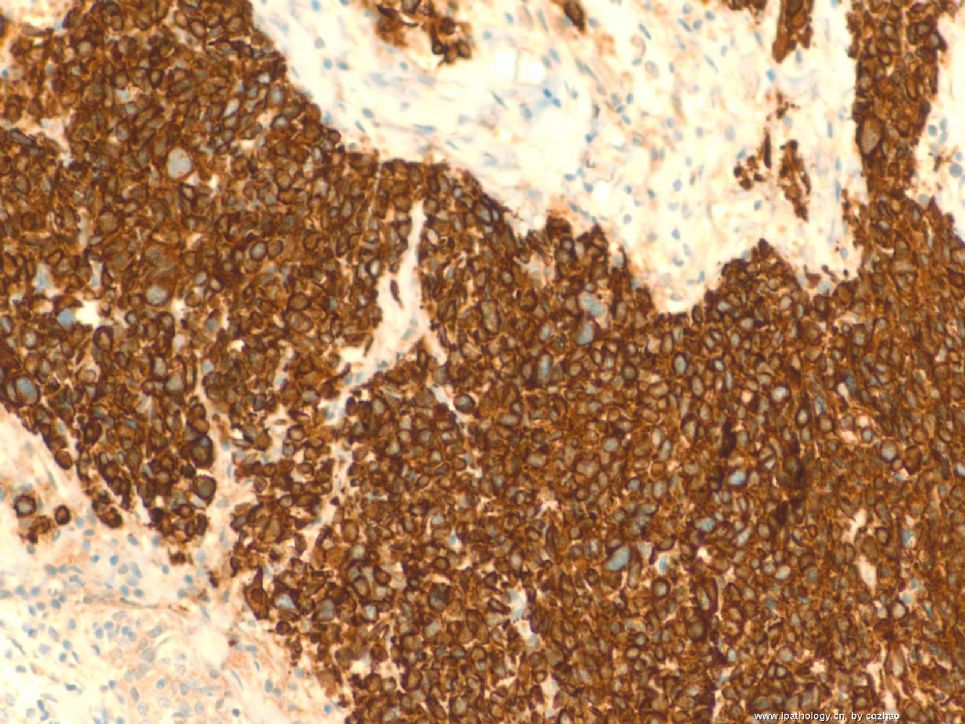
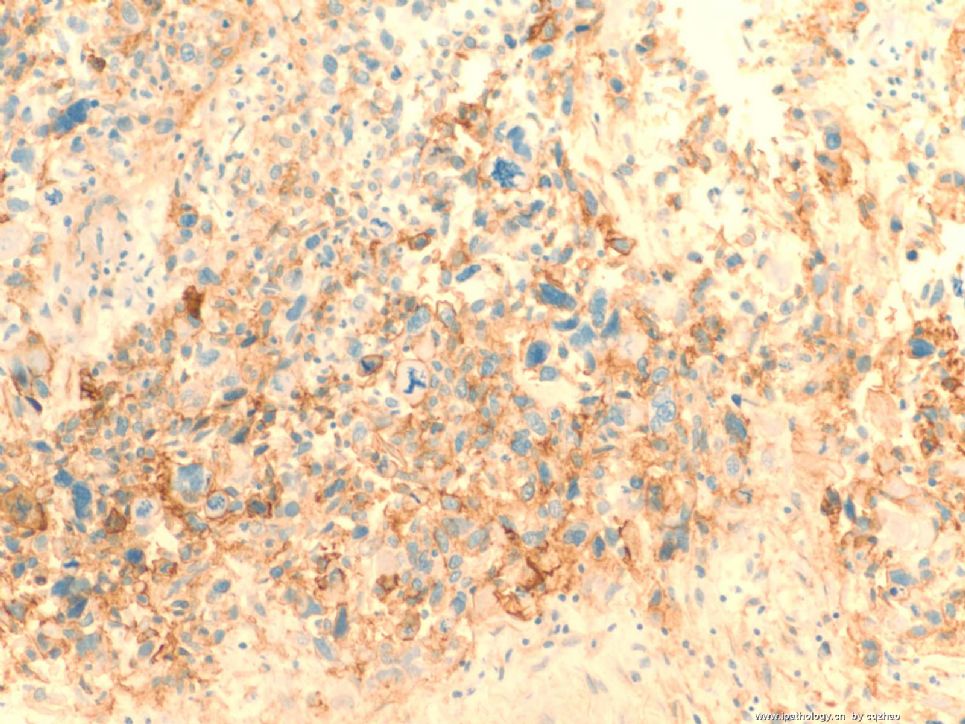
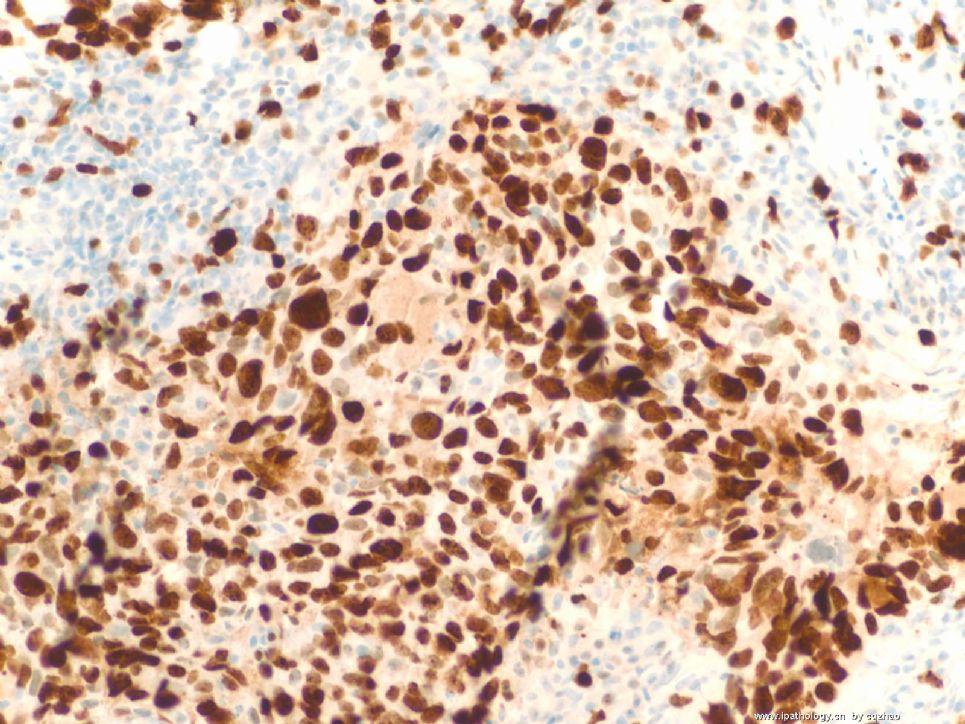
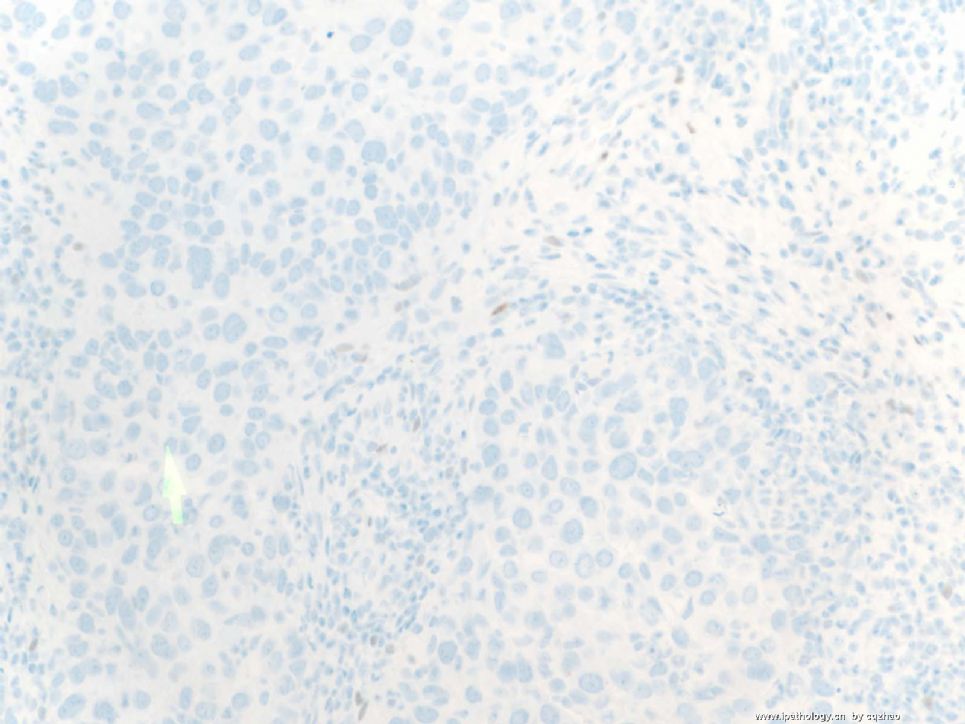
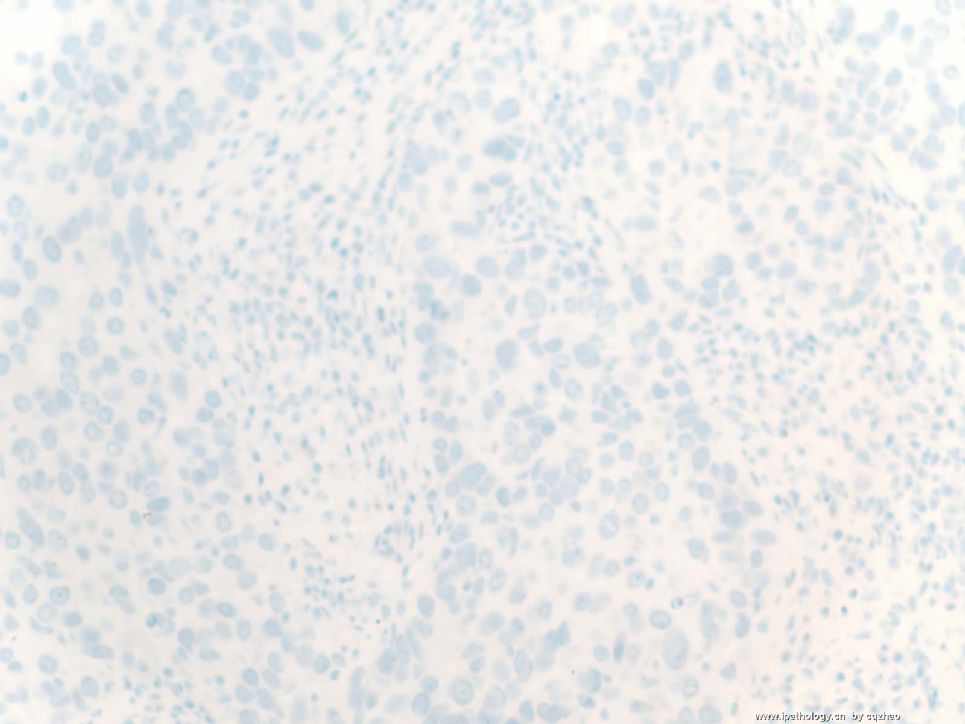
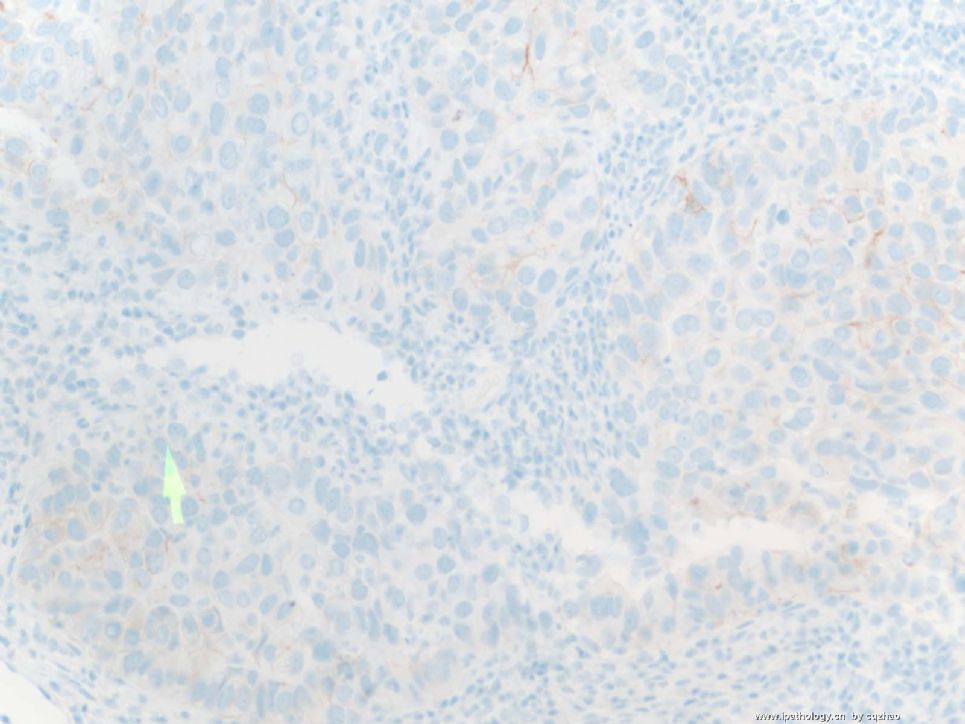
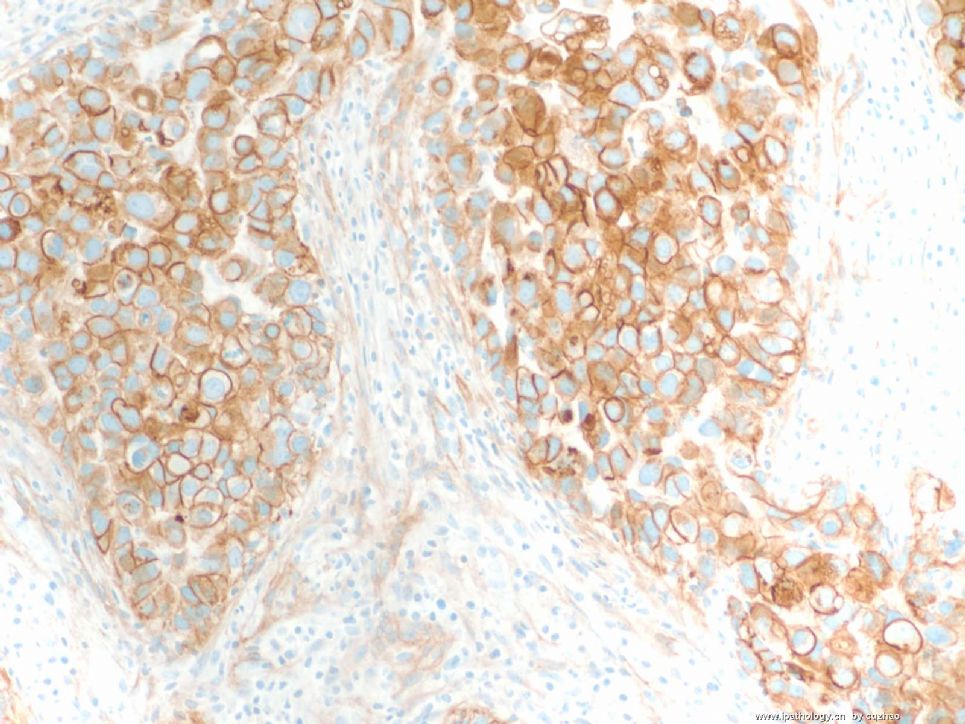
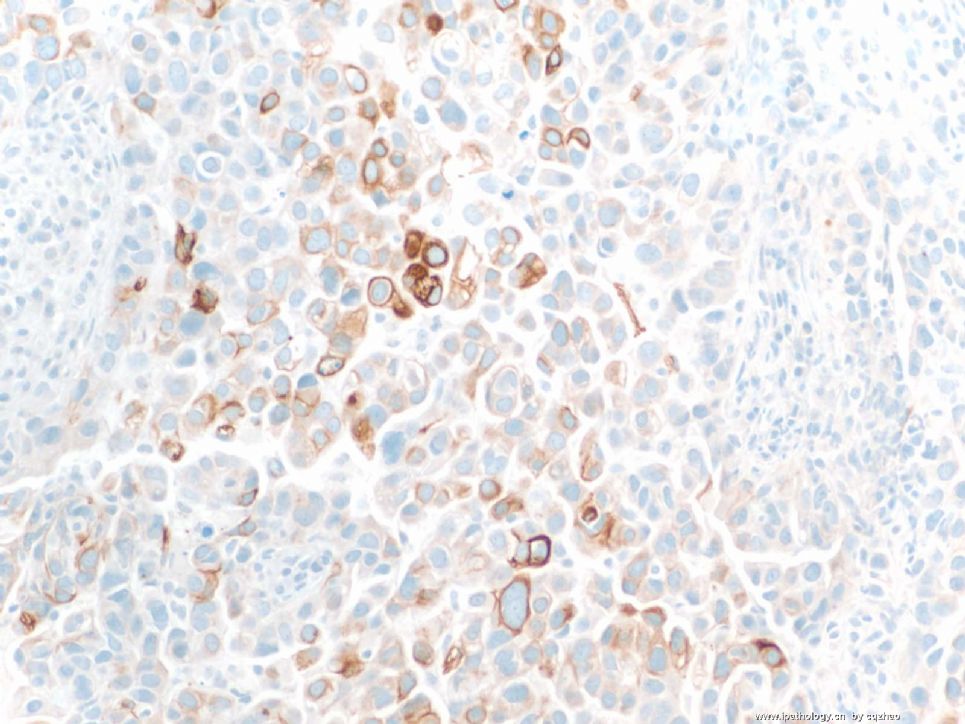
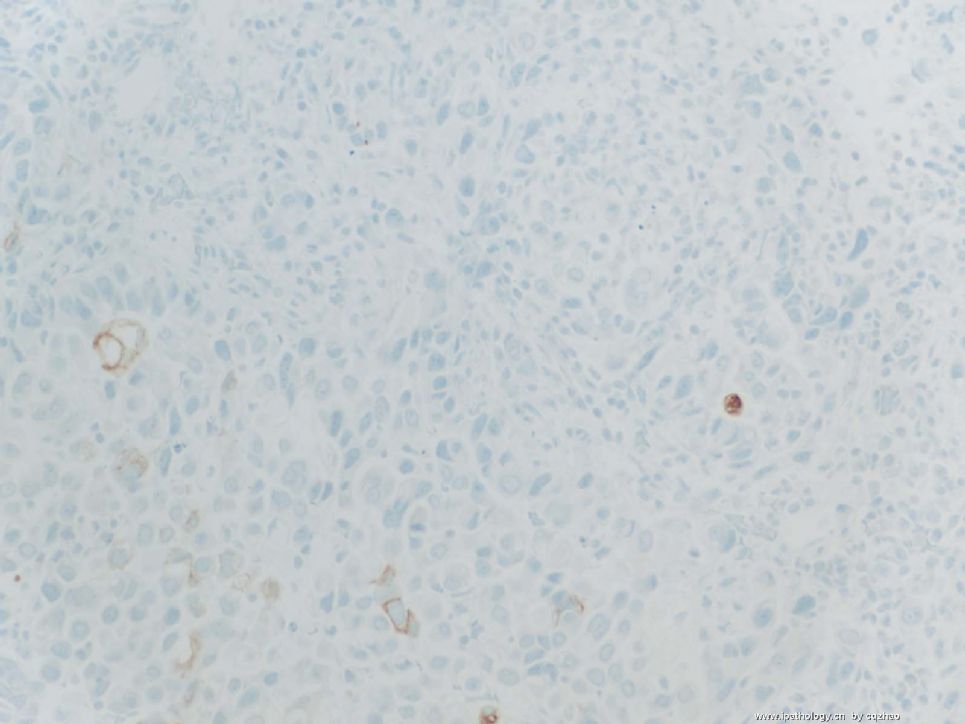
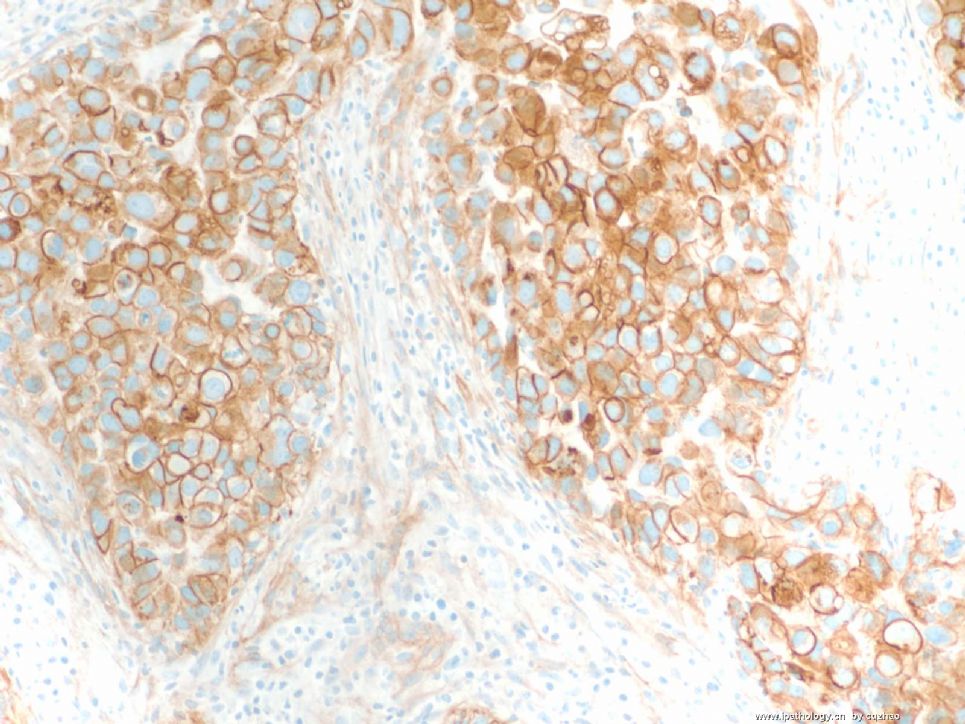
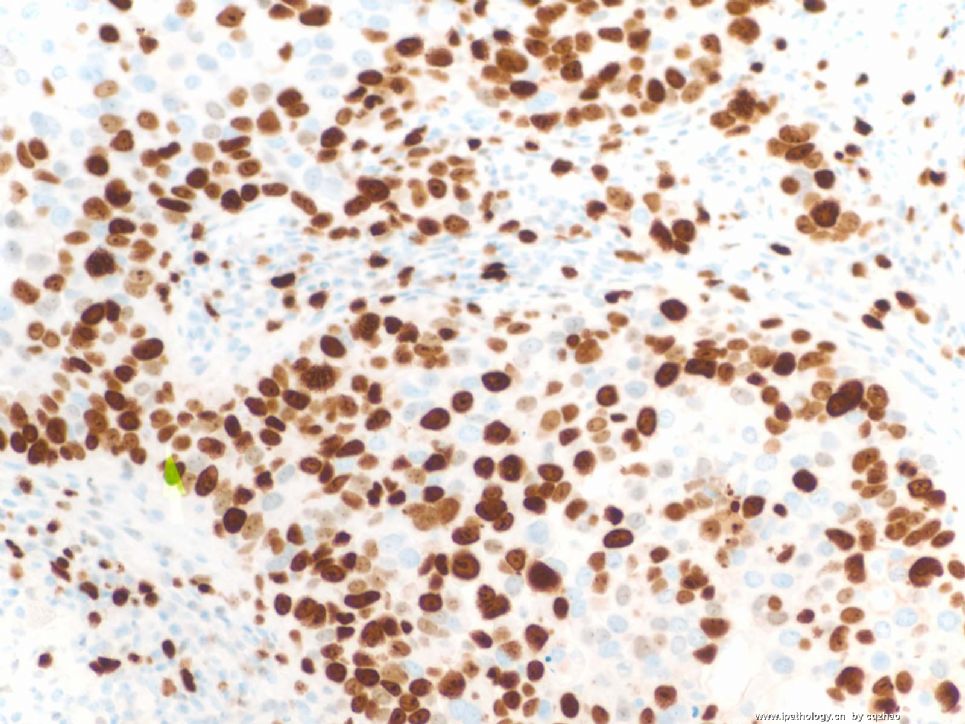
2. Generally we use 4 markers (ck14, ck17, ck5 or ck5/ck6, EGFR). I did not meet the cases with positivity <10% for all four markers. Generally some markers may be more stronger or intensity stains than others.
3. EGFR is not specific and is positive for many tumors. Clinically anti-EGFR drugs can be used to treat the cancers with positive EGFR, for example lung carcinoma..In my impression EGFR often is weak staining or negative for basal-like breast carcinoma. People use this marker for basal-like ca becasue it was used in the begining study. If the cases with only EGFR positive and all other basal-like markers negative, I do not think they are basal-like ca.
just for your reference.
-
本帖最后由 于 2009-01-11 23:01:00 编辑
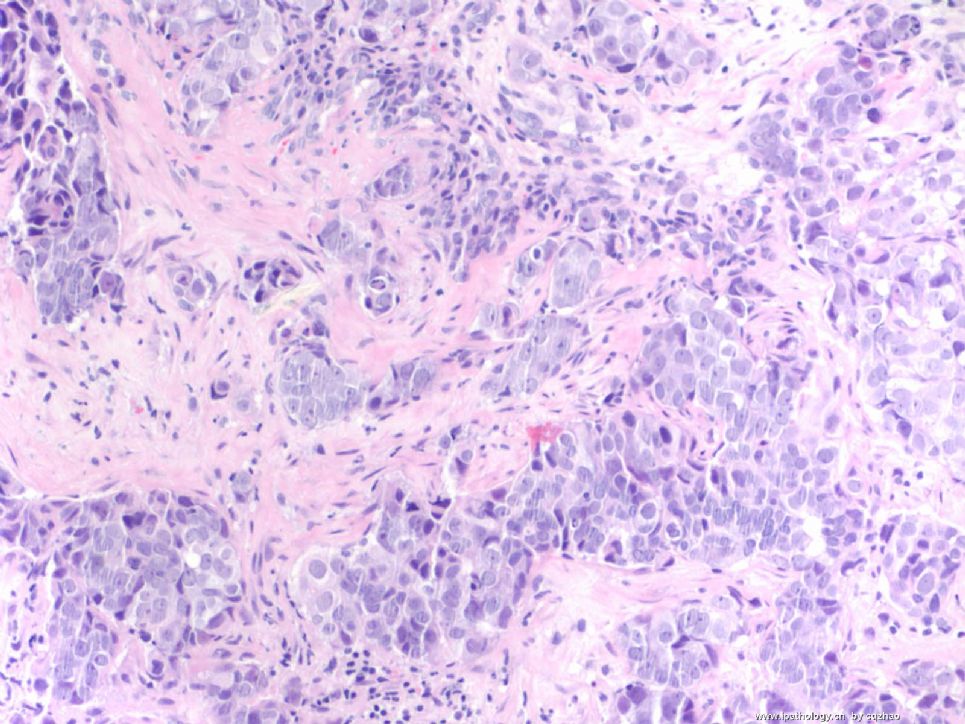
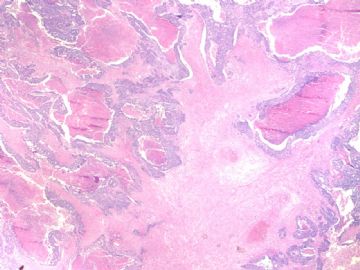
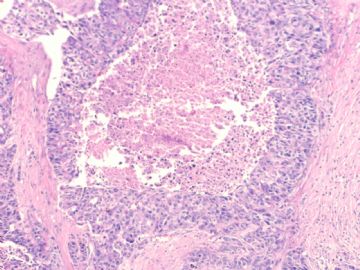
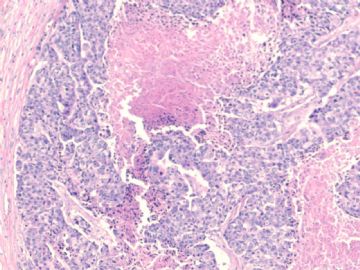
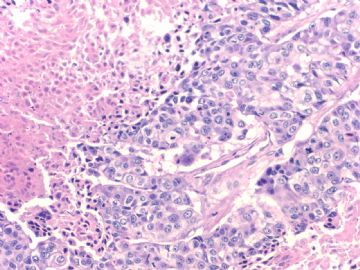
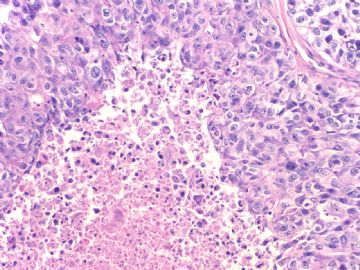
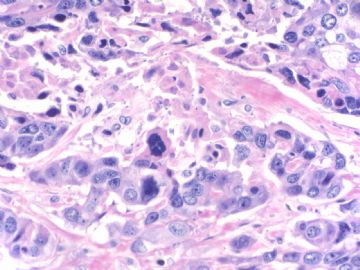
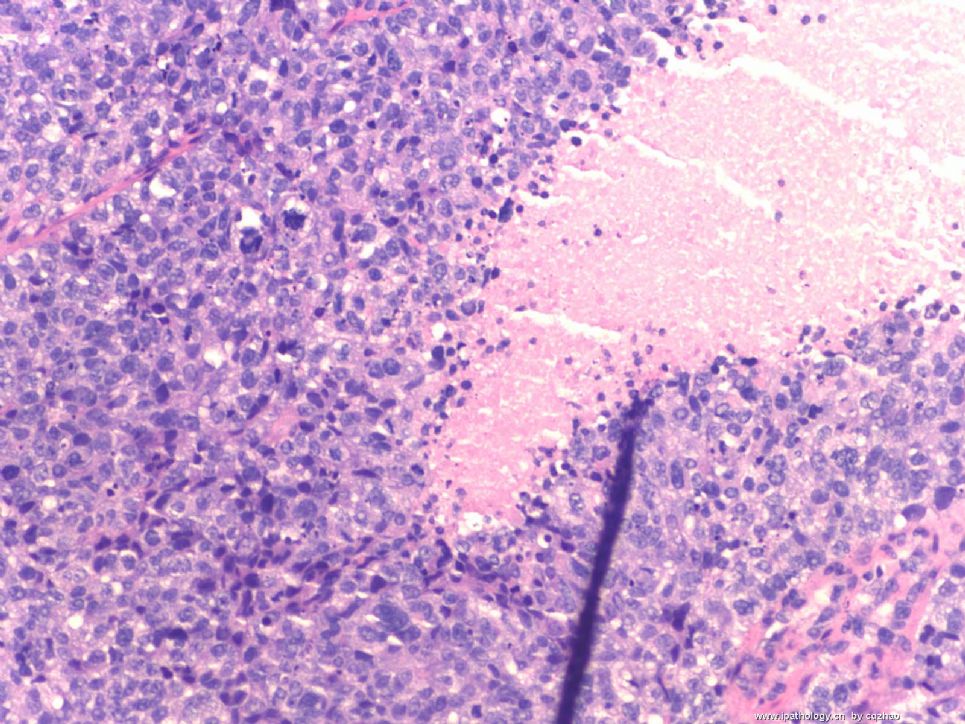
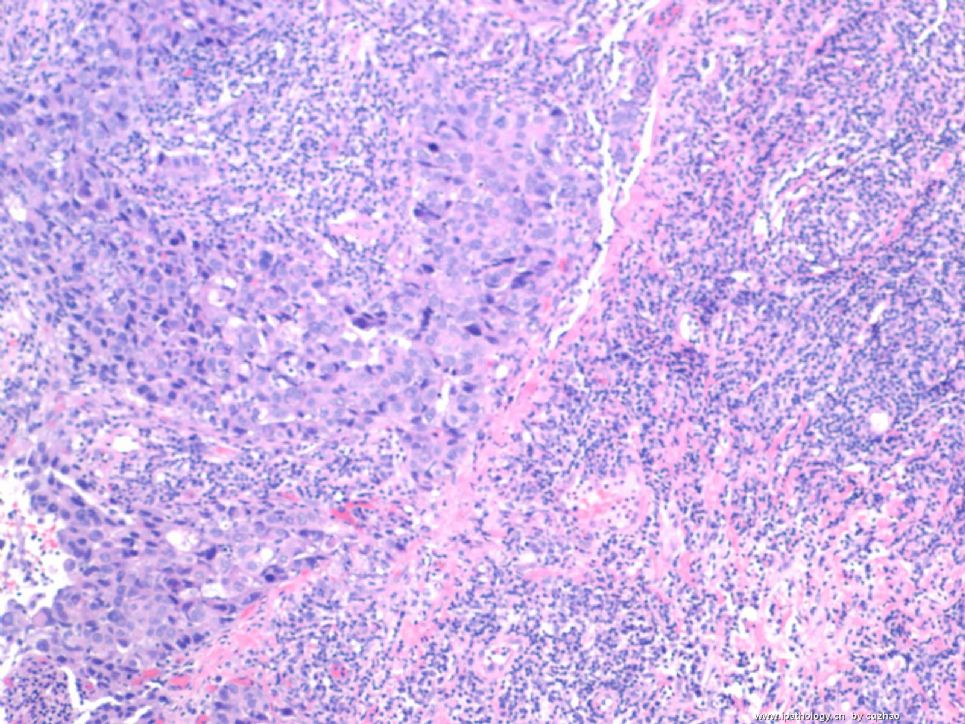
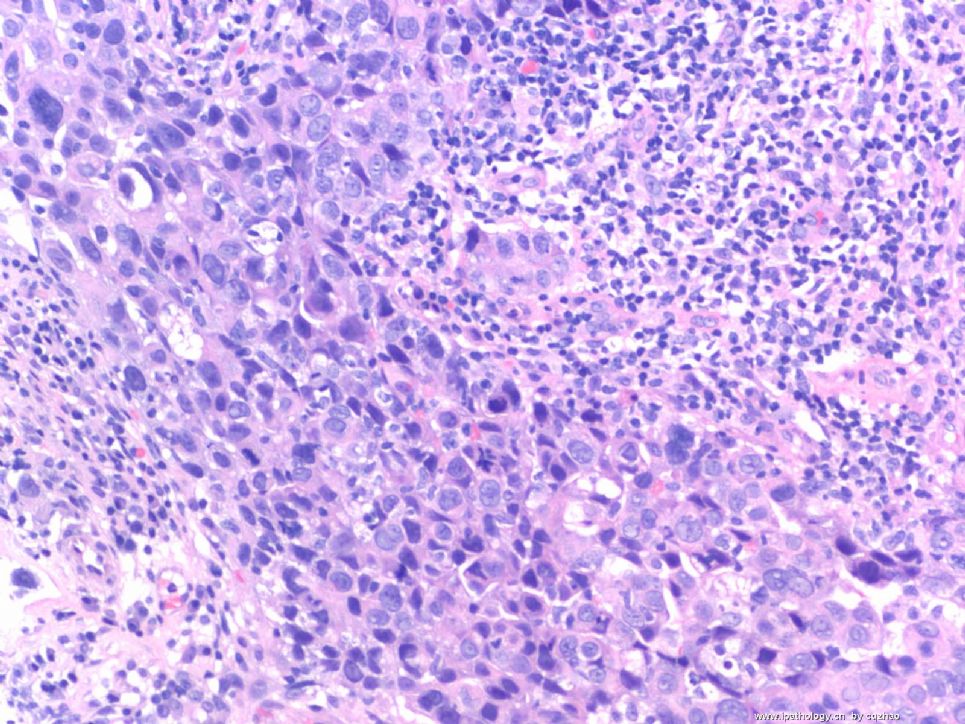
Ok, every one, totally I sent here 6 basal-like ca here with three cases showing the IHC panel we used. Also I briefly discussed characteristics of this cancer.
You should learn from 天山望月 to summary some main cytomorphologic and IHC featrures by yourself. Generally breast pathologists will know the case may be a basal-lik ca by H&E. Hope you know it also. Variations occure always. My friend's study indicated that CK5 is most sensitive marker. However Ck5 essentially is negative for above case 1. We always should order few markers, but not one only. Ki67 is not cecessary for dx. But you can see most of the cases showed very high proliferative index.
I will enclose this topic here.
Thank you all for reviwing the this topic, especially for some ones who joined the discussion.
| 以下是引用天山望月在2008-12-17 0:07:00的发言:
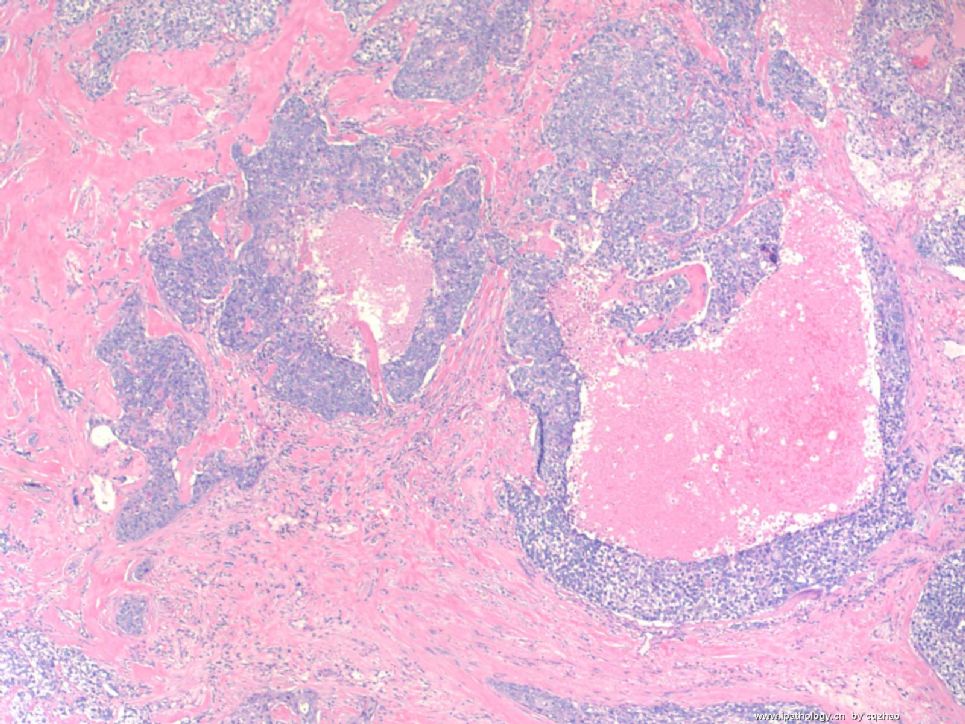
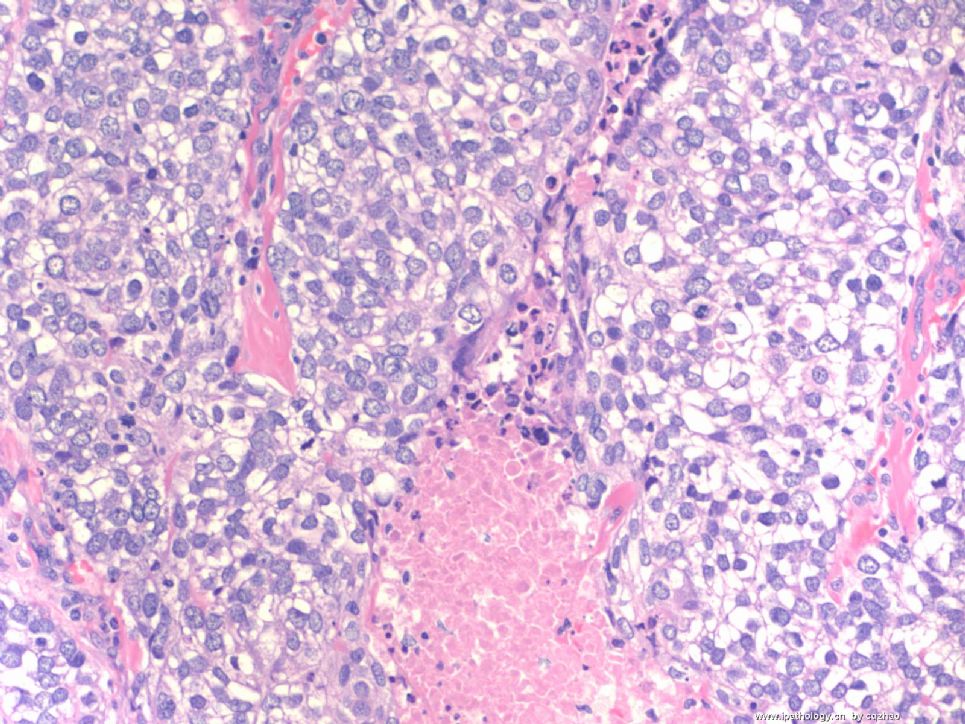
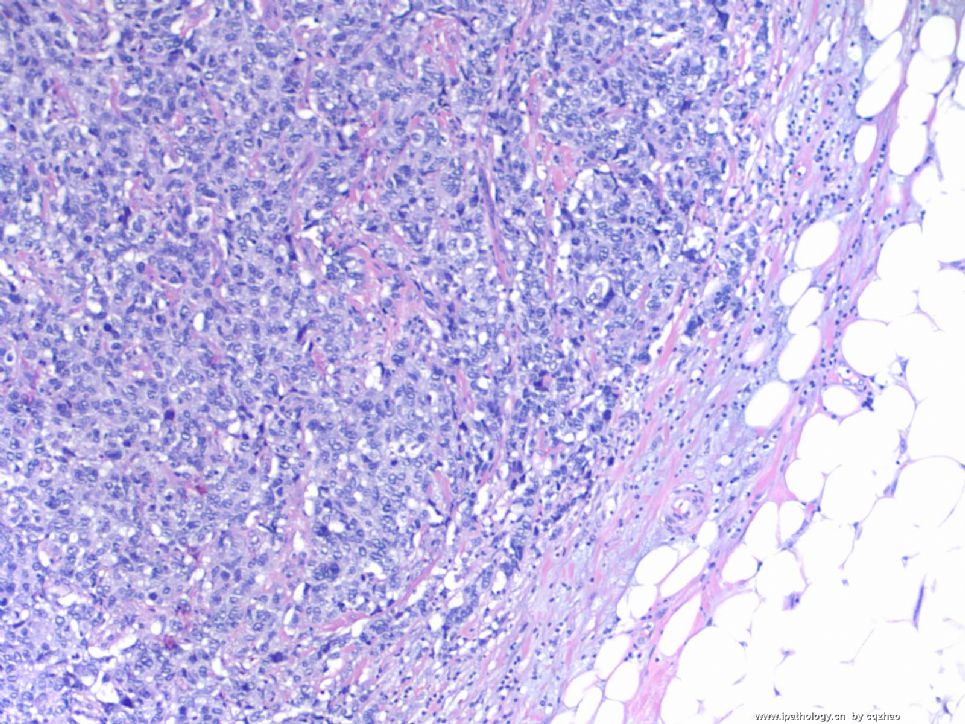
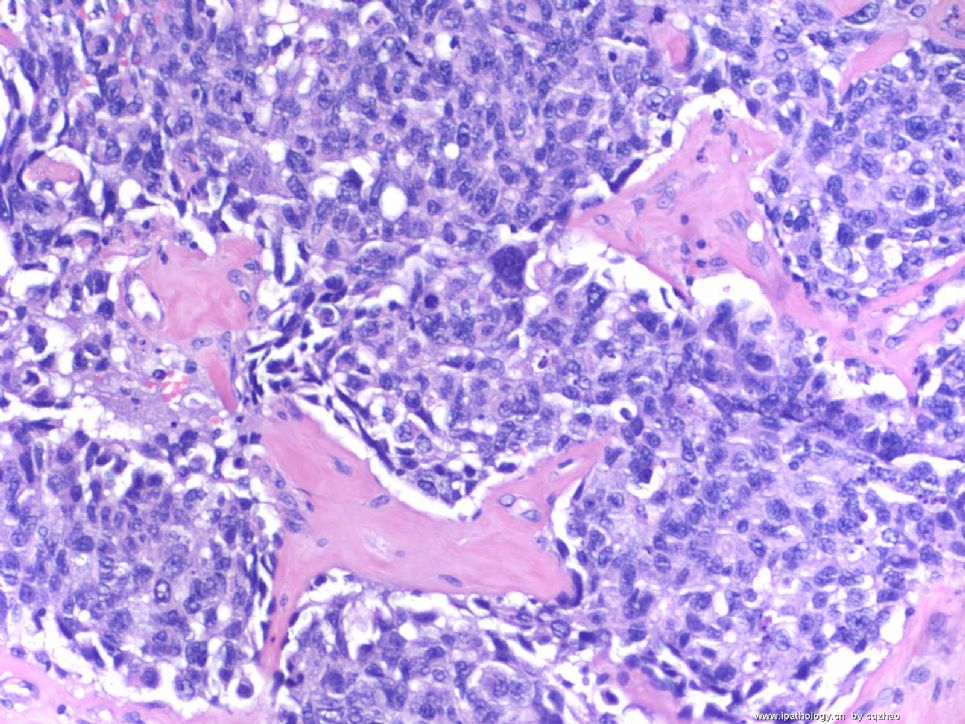
谢谢Dr.zhao无私奉献这么多好病例! 反复仔细阅读这几例,深深领会,肿瘤的膨胀性、浸润性生长方式,不规则片状排列,胞界不清,浆少、多形性的瘤细胞,核细沙粒样,有核仁,易见核分裂,疤痕样胶原化,地图样坏死等特点。 |




 对我们非常有帮助!
对我们非常有帮助!