| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 女,31岁,大网膜
| 姓 名: | ××× | 性别: | 女 | 年龄: | 31岁 |
| 标本名称: | 大网膜 | ||||
| 简要病史: | 女31,下腹痛13天,加剧2天。于2004年8月23日入院。 | ||||
| 肉眼检查: | 术中见淡黄色腹水500ml,腹膜尚光滑,大网膜明显增厚,表面粟粒状,大网膜与横结肠融合成团,与膀胱反折腹膜粘连。子宫直肠凹及小网膜表面见细小粟粒状结节。子宫双附件表面无异常。肝、脾、胃表面无结节,无肿块。切除横结肠以下饼状大网膜。病理大体检查:僵硬大网膜组织约24*15*2cm,表面及切面见多数灰白结节,结节0.1-1cm,切面灰白色,质地较硬。 | ||||
这个病史是我翻阅病历后整理出来的,图片也是我自己拍摄的。图8-10,13-14为油镜。
-
本帖最后由 于 2007-08-17 19:48:00 编辑

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
-
本帖最后由 于 2007-02-26 22:39:00 编辑
今天翻阅了病历,并复习了HE图片和免疫组化。主要更正:
1、术前6个月多(2004年1月,春节前)有“盆腔炎”住院治疗并“缓解”史,首次发作到死亡时间约1年;
2、免疫组化:
上皮标记:CK、CK18、EMA弥漫强阳性(可见刷状缘);Vimentin弥漫阳性。提示双相分化。
间皮标记:Calretinin散在阳性,Mes阴性,HBME-1和CK5/6未检测。提示可疑间皮分化。
激素及受体:HCG阳性(与此一致,血HCG轻度升高),HPL和PLAP可疑阳性;ER和PR未检测。提示可疑中间滋养细胞分化。
血管(内皮)标记:F-Ⅷ- CD34- CD31-
其他标记:S100、HMB45、α-inhibin、p63、E-Cadherin、EGFR均阴性,Ki67阳性细胞数<10%。
3、电镜未见微绒毛(石蜡组织做的电镜,但我们没有看到电镜照片)

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
应部分朋友的要求,提供逐句翻译:
Malignant deciduoid mesothelioma, a rare phenotype of epithelioid mesothelioma, arises more commonly from the peritoneum of young women, but it is also reported in the pleura of elderly people. 恶性蜕膜样间皮瘤是上皮样间皮瘤的一种罕见表型,多来源于年轻女性的腹膜,但也有报道来自年龄更大者的胸膜。We report a case of malignant deciduoid mesothelioma that occurred in a 41-year-old woman after cesarean section and was initially misdiagnosed as pseudotumoral deciduosis. 我们报道一例恶性蜕膜样间皮瘤,发生于41岁剖宫产后妇女,最初被误诊为假肿瘤样蜕膜病。Microscopically, the tumor was entirely composed of deciduoid areas, and only scattered tumor cells were positive for calretinin and keratin 5/6. 镜下,肿瘤全部由蜕膜样区域组成,仅散在的肿瘤细胞呈Calretinin和CK5/6阳性。The patient died 14 months after the first operation. This observation confirms the poor prognosis of this entity and the importance of the differential diagnosis of pseudotumoral deciduosis. 患者首次手术后14月死亡。这些观察证实了此类病变的预后差,及其与假肿瘤样蜕膜病鉴别的重要性。
Malignant deciduoid mesothelioma (MDM) is a recently characterized variant of epithelial malignant mesothelioma that closely simulates exuberant ectopic decidual reaction. 恶性蜕膜样间皮瘤(malignant deciduoid mesothelioma,MDM)是上皮样恶性间皮瘤的一个亚型,最近才认识到它的特征:与高度增生的蜕膜反应非常相似。 It was first described by Nascimento et al
REPORT OF A CASE
A previously healthy 41-year-old woman with an unremarkable medical history complained of abdominal pain 6 weeks after undergoing a cesarean section. 41岁妇女,既往体健,无明显就医史,剖宫产6周后诉腹痛。There was no history of asbestos exposure in the patient or her family. 患者及其家庭无石棉暴露史。At surgery, there was 900 mL of ascites. Numerous micronodules that affected the peritoneal cavity, omentum, and surface of the uterus and ovaries were observed. 术中腹水900ml,腹腔、网膜、子宫和卵巢表面见大量小结节。The intraoperative appearance suggested peritoneal carcinomatosis, and the patient underwent a total abdominal hysterectomy, bilateral salpingo-oophorectomy, and omentectomy. 术中外观提示为多处转移癌,行全腹子宫切除、双附件切除和网膜切除。The diagnosis of pseudotumoral deciduosis was initially rendered, and no treatment was administered.最初诊断为假肿瘤样蜕膜病,未作特殊治疗。
There was a short remission period following the surgery, but the patient complained of recurrent abdominal pain and a laparoscopy was performed. 术后暂时缓解,但患者诉复发性腹痛,并行腹腔镜检查。 Two months later, she was referred to our hospital for the treatment of multiple intestinal fistulas. 2月后因多处肠瘘再次入院治疗。Laboratory investigations showed an elevated CA 125 level (300 U/mL; reference range, ,36 U/mL), but the other tumor markers, including serum b-human chorionic gonadotropin (bhCG) level, were within the reference ranges. 实验室检查:CA
Two weeks later, a subsequent laparotomy showed loops of small bowel matted together and covered by numerous deposits of firm white tissue, which formed nodules and plaques both on the visceral and parietal peritoneal surface and in the Douglas cavity. 二周后,剖腹手术发现小肠缠成环状,覆无数白色质硬沉积物,在内脏表面、壁层腹膜和Douglas窝形成结节和斑块。 A resection of the matted loops of small bowel was performed. The patient’s condition gradually deteriorated, and she died 14 months after the onset of symptoms.切除了缠结成环的小肠。术后患者情况逐渐恶化,首发症状14月后死亡。
MATERIALS AND METHODS
All specimens were fixed in 10% buffered formalin and embedded in paraffin. 所有标本固定于10%缓冲福尔马林内,石蜡包埋。 Serial 4-mm-thick sections were stained with hematoxylin-eosin. 连续切片,片厚4μm,HE染色。Immunostaining was performed using antibodies for cytokeratin (KL1, Immunotech, Marseille, France), keratin 5/6 (Dako Corporation, Carpinteria, Calif), epithelial membrane antigen (Dako), vimentin (Dako), calretinin (Zymed, San Francisco, Calif), smooth muscle actin (Dako), desmin (Dako), S100 protein (Dako), CD15 (Immunotech), carcinoembryonic antigen (Dako), b-hCG (BioGenex, San Ramon, Calif), placental alkaline phosphatase (Dako), estrogen receptor (Dako), and progesterone receptor (BioGenex). 免疫组化:CK(KL1)、CK5/6、EMA、Vimentin、Calretinin、SMA、Desmin、S100、CD15、CEA、HCG、PLAP、ER、PR。
PATHOLOGIC FINDINGS
The thoracic nodule measured up to
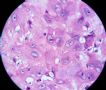
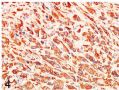
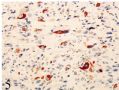
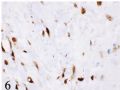
In the tumor cells, immunohistochemical analysis revealed diffuse and strong positivity for keratin (Figure 4) and vimentin and moderate positivity for epithelial membrane antigen. 免疫组化分析发现:肿瘤细胞CK和Vimentin弥漫强阳性(图4),EMA中等强度阳性。 Only scattered tumor cells were positive for keratin 5/6 (Figure 5) and calretinin (Figure 6). 仅散在细胞呈CK5/6阳性(图5)和Calretinin(图6)。All other stains, including germ cell markers and hormonal receptors, were negative. The diagnosis of MDM was made.其它染色阴性,包括生殖细胞标记和激素受体。诊断:MDM。
COMMENT
Malignant deciduoid mesothelioma was defined by Nascimento et al
Malignant deciduoid mesothelioma apparently is rare, accounting for less than 5% of the mesotheliomas cases reviewed by Shia et al5 and for less than 2% reviewed by Ordonez.2 MDM显然罕见,据Ordonez回顾,不到间皮瘤病例的5%,而Ordonez回顾中<2%[2]。In contrast to classic mesothelioma, several features noted in patients with MDM are worth mentioning: its predilection to peritoneum (54% to 20%), the female preponderance (female-male ratio, 1.4:1), the young age of patients (40 years or younger), and the lower rate of asbestos exposure (35% to 80%).5与经典的间皮瘤相比,MDM有几个特征值得重视:好发于腹膜(54%~20%),女性占优势,年轻(40岁或以下),石棉暴露率低(35%~80%)。
The deciduoid morphologic features appear to be a spectrum from mesotheliomas of conventional appearance with focal deciduoid areas to mesotheliomas that are predominantly or possibly entirely, as in our case, deciduoid.3蜕膜样形态特点似乎是一个谱系,从间皮瘤的普通表现伴蜕膜样区,到蜕膜样区为主,或可能全部为蜕膜样区,正如我们这例[3]。 In addition, MDMs are composed of a proliferation of large, round, ovoid, and polygonal cells with sharp cellular outlines, abundant glassy eosinophilic cytoplasm, and round vesicular nuclei with prominent eosinophilic nucleoli. 而且,MDM的组成细胞呈大、圆、卵圆和多角形,伴清晰的细胞轮廓,丰富的毛玻璃样嗜酸性胞浆,圆的空泡状核有显著嗜酸性核仁。 Binucleation forms are occasionally present, but despite the cellular atypia and anaplasia, mitotic figures are infrequent.1–3偶尔出现双核,但尽管细胞异型性和间变性显著,核分裂却少见[1-3]。 The cell cytoplasm is often more dense and darker around the nucleus and lighter at the periphery. 5胞浆通常在核周更致密、更深染,而周边部较透亮[5]。 The cells are arranged in anastomosing sheets or in small clusters, separated by a fibrous or loose edematous stroma. 细胞排列成吻合的片状或小簇状,隔以纤维性间质或疏松水肿的间质。The histologic description of MDM was given by Talerman et al
In our case, the diagnostic confusion betweenMDMand diffuse pseudotumoral deciduosis could have been avoided by careful study of the macroscopic and histologic features. 我们这例MDM与弥漫性假肿瘤样蜕膜病的混淆,本来可以通过仔细研究大体和镜下特点而避免。 Macroscopically, deciduosis, frequently described in pregnancy but also observed in the perimenarchal and postmenopausal periods, manifests as small discrete nodules or excrescences on the peritoneal surface and not as large, firm plaques and nodules. 大体上,蜕膜病通常发生于妊娠期,但也可见于月经期前后和绝经期前后,在腹膜表面呈小而分散的结节或赘生物,而不是大而坚硬的斑块和结节。 However, an occasional case of exuberant decidual reaction can give rise to bulky pseudotumoral lesions in which necrosis and cellular pleomorphism can be observed.7然而,高度增生的蜕膜反应偶尔能引起大块的假肿瘤样病变,可见坏死和细胞多形性[7]。 The extensive involvement of the peritoneal cavity and the presence of ascites militate against the diagnosis of deciduosis. 广泛的腹腔累犯和存在腹水,不支持蜕膜病的诊断。Microscopically, in deciduosis, the sheets of decidual cells are present within the connective tissue and do not usually affect its surface, as in the case of mesothelioma. 镜下,蜕膜病的片状蜕膜细胞存在于结缔组织内,通常不像间皮瘤那样影响其表面。 In both entities, the cells have large amount of cytoplasm, but the nuclei differ considerably. The nuclei of the decidual cells are smaller and have dark clumped chromatin, whereas the nuclei of mesothelioma cells are vesicular with fine chromatin, prominent nucleolus, and occasional mitotic figures. 2,4,6这两种病变的细胞都有大量胞浆,但核明显不同。蜕膜细胞的核较小,有深染的粗块状染色质,而间皮瘤细胞的核呈空泡状伴纤细的染色质、显著的核仁和偶见的核分裂[2,4,6]。 The presence of typical areas of classic mesothelioma leads to the diagnosis. In our case, such areas were not discovered even after careful sampling of the specimen.存在经典间皮瘤的区域可导致诊断。在我们的这例,即使仔细取材,这样的区域也未观察到。
Immunohistochemical data appear not to be particularly useful in differentiating these 2 processes. 免疫组化对这两种病变的区分似乎作用不大。Nascimento et al1 considered the negativity of deciduoid cells for cytokeratin to be significant. However, in a more recent study, Healthy et al8 reported a positivity for cytokeratin (AE1/3 and CAM 5.2) in 30% of extrapelvic deciduosis. Nascimento等[1]认为蜕膜样细胞CK阴性有意义;然而,最近Healthy等的研究发现30%的盆腔外蜕膜病呈CK(AE1/3和CAM5.2)阳性。Cytokeratin 5/6 has recently been reported as a sensitive and relatively specific positive finding in the diagnosis of mesothelioma, particularly when staining is strong and diffuse.3最近认为CK5/6是敏感和相对特异性的间皮瘤标记,特别是呈强而弥漫的着色时[3]。Only scattered tumor cells were positive for this marker in our observation. 我们这例仅散在的肿瘤细胞呈CK5/6阳性。 Calretinin, a molecule considered sensitive and relatively specific for mesothelioma, was expressed in scattered tumor cells in our case. Calretinin是间皮瘤敏感而相对特异性的标记物,在我们这例也仅有散在的肿瘤细胞表达。Riera et al9 found calretinin to lack sensitivity and to a lesser extent specificity. Riera等[9]发现calretinin缺乏敏感性且特异性小。In fact, only 2 of 5 cases reported by Shia et al5 were positive for calretinin. Tumor cells in the case published by Orosz et al10 were also focally positive for this antibody. 事实上,Shia等[5]报道仅2/5病例呈calretinin阳性,Orosz等[10]报道此抗体呈局灶阳性。The diagnosis was made in these cases by ultrastructural study. 这些病例的诊断是依据电镜研究。 The presence of numerous cytoplasmic intermediate filaments, either dispersed or bundled, appears to be the likely ultrastructural basis for the deciduoid histologic appearance.5存在无数的胞浆内中间丝,或弥漫或束状分布,可能是蜕膜样组织学表现的超微结构基础[5]。
From the prognostic point of view, MDMs are highly malignant; the mean survival time is 7.33 months (range, 1–21 months).5从预后角度看,MDM为高度恶性,平均生存期7.33月(范围1-22月)[5]。A recent study11 of peritoneal malignant mesothelioma in women found that 40% of the patients survived longer than 4 years. 最近对女性腹膜间皮瘤的一项研究[11]发现40%患者的生存期超过4年。The poor prognosis of our observation confirms the particularly aggressive nature of this entity.我们这例的预后差,可证实本病特殊的侵袭性特点。
Our case shows similar morphologic and clinical features to previously published examples of MDM that occurred in young women. 我们这例相似于以往报道的发生于年轻女性MDM病例。 We advocate distinguishing this clinicopathologic subtype of MDM from the deciduoid mesothelioma variant, which arises in the pleura and peritoneum of elderly individuals with a prior history of asbestos exposure. 我们提议将MDM的临床病理亚型与蜕膜样恶性间皮瘤亚型区分开,后者发生于较年老者的胸膜和腹膜,有石棉暴露史。Further studies on a large number of cases may be helpful in more fully delineating the clinical and pathologic features of this rare variant of mesothelioma.进一步研究更多病例,将有助于更全面地描述这一罕见间皮瘤亚型的临床和病理特征。
In summary, we report a case of MDM that occurred in a 41-year-old woman 6 weeks after cesarean section and was misinterpreted as pseudotumoral deciduosis. 总之,我们报道这例41岁女性剖宫产后6周发生的MDM,最初误诊为假肿瘤样蜕膜病。 This case highlights the need of the pathologist to be aware of this subtype of malignant mesothelioma to avoid a misdiagnosis of a benign process. 此例强调病理学家需要了解恶性间皮瘤的这一亚型,以避免误诊为良性病变。 We share the opinion that MDM may still represent a distinct subtype of epithelioid mesothelioma, with specific clinical and pathologic features.我们提出一个观点,即MDM可能仍代表上皮样间皮瘤的一个独特亚型,伴特殊的临床和病理特征。
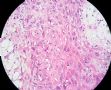
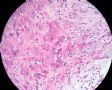
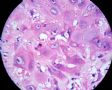
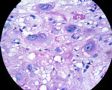
Figure 1. Large polygonal cells with abundant eosinophilic cytoplasm, sharp cellular outlines, and a peripheral zone of cytoplasmic pallor. Nuclei are pleomorphic, with vesicular chromatin and a single prominent nucleolus. Rare mitotic figures are identified (hematoxylin-eosin, original magnification *400). 图1 大的多角形细胞有丰富的嗜酸性胞浆,细胞轮廓清晰,有一胞浆周围空白区。核多形性,空泡状染色质,单个显著核仁。罕见核分裂。(HE400X)
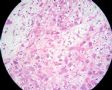
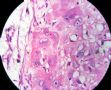
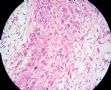
Figure 2. Tumor cells invading the dermis and separated by a hyalinized areas (hematoxylin-eosin, original magnification *100). 图2 肿瘤细胞侵犯真皮,隔以透明变性区。(HE100X)
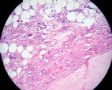
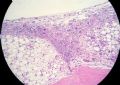
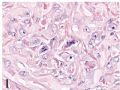
Figure 3. Tumor cells invading the intestinal submucosa (hematoxylin-eosin, original magnification *50). 图3 肿瘤细胞侵犯肠粘膜下层。(HE50X)
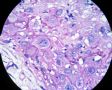
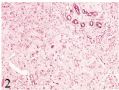
Figure 4. Tumor cells are strongly positive for cytokeratin (KL1, original magnification *200). 图4 肿瘤细胞CK(KL1)强阳性。(200X)
Figure 5. Only scattered tumor cells are positive for keratin 5/6 (original magnification *200). 图5 仅散在肿瘤细胞呈CK5/6阳性。(200X)
Figure 6. Only scattered tumor cells are positive for calretinin (original magnification *400).图6仅散在肿瘤细胞呈calretinin阳性。(400X)

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
-
本帖最后由 于 2007-02-22 22:47:00 编辑
全文翻译:
恶性蜕膜样间皮瘤的诊断挑战
摘要:恶性蜕膜样间皮瘤是上皮样间皮瘤的一种罕见表型,多来源于年轻女性的腹膜,但也有报道来自年龄更大者的胸膜。我们报道一例恶性蜕膜样间皮瘤,发生于41岁剖宫产后妇女,最初被误诊为假肿瘤样蜕膜病(pseudotumoral deciduosis)。镜下,肿瘤全部由蜕膜样区域组成,仅散在的肿瘤细胞呈Calretinin和CK5/6阳性。患者首次手术后14月死亡。这些观察证实了此类病变的预后差,及其与假肿瘤样蜕膜病鉴别的重要性。
恶性蜕膜样间皮瘤(malignant deciduoid mesothelioma,MDM)是上皮样恶性间皮瘤的一个亚型,最近才认识到它的特征:与高度增生的蜕膜反应非常相似。它最初由Nascimento[1]等于1994年描述,发生于年轻女性的腹膜,但更多观察也指出它可发生于较年长者以及胸膜[2]。这一少见的恶性间皮瘤亚型极罕见,据我们所知,文献中仅报道过29例。我们报道1例46岁妇女剖宫产后发现的MDM,最初被误诊为假肿瘤样蜕膜病。
病例报道
41岁妇女,既往体健,无明显就医史,剖宫产6周后诉腹痛。患者及其家庭无石棉暴露史。术中腹水900ml,腹腔、网膜、子宫和卵巢表面见大量小结节。术中外观提示为多处转移癌,行全腹子宫切除、双附件切除和网膜切除。最初诊断为假肿瘤样蜕膜病,未作特殊治疗。
术后暂时缓解,但患者诉复发性腹痛,并行腹腔镜检查。2月后因多处肠瘘再次入院治疗。实验室检查:CA125升高(300U/ml,参考范围<36 U/ml),但其他肿瘤标记包括HCG等均在参考值范围内。CT发现胸膜壁层异源性结节,侵及真皮,伴肋骨溶骨性破坏。切除部分结节作组织学检查。
二周后,剖腹手术发现小肠缠成环状,覆无数白色质硬沉积物,在内脏表面、壁层腹膜和Douglas窝形成结节和斑块。切除了缠结成环的小肠。术后患者情况逐渐恶化,首发症状14月后死亡。
材料和方法
所有标本固定于10%缓冲福尔马林内,石蜡包埋。连续切片,片厚4μm,HE染色。免疫组化:CK(KL1)、CK5/6、EMA、Vimentin、Calretinin、SMA、Desmin、S100、CD15、CEA、HCG、PLAP、ER、PR。
病理学发现
胸部结节最大径3cm,白色,质硬。镜下,结节由大的多角形或卵圆形细胞组成,含丰富的嗜酸性毛玻璃样胞浆,细胞轮廓清晰。核多形性、空泡状,有单个显著核仁(图1)。核分裂罕见,部分细胞胞浆有一偏心的外围苍白区,与中央的核周毛玻璃样区分界明显(图1)。肿瘤细胞排列成实性片状,由纤维性或疏松水肿的间质分隔,有时伴透明变性区(位于肿瘤边缘或位于肿瘤片内)(图2)。部分肿瘤坏死,肿瘤细胞侵犯真皮(图2)。大量切片未见间皮瘤的其它典型形态,如乳头结构、管状结构或索状结构。肠切除标本显示成片的蜕膜样肿瘤细胞,侵犯粘膜下层(图3)。
免疫组化分析发现:肿瘤细胞CK和Vimentin弥漫强阳性(图4),EMA中等强度阳性。仅散在细胞呈CK5/6阳性(图5)和Calretinin(图6)。其它染色阴性,包括生殖细胞标记和激素受体。诊断:MDM。
评注
MDM由Nascimento等1994年定义,典型者为年轻女性,发生于腹膜,高度侵袭性行为,预后差,病因学上与石棉接触无关。然而,后来也有发生于较年老和胸膜的报道,有时与石棉暴露有关。
MDM显然罕见,据Ordonez回顾,不到间皮瘤病例的5%,而Ordonez回顾中<2%[2]。与经典的间皮瘤相比,MDM有几个特征值得重视:好发于腹膜(54%~20%),女性占优势,年轻(40岁或以下),石棉暴露率低(35%~80%)。
蜕膜样形态特点似乎是一个谱系,从间皮瘤的普通表现伴蜕膜样区,到蜕膜样区为主,或可能全部为蜕膜样区,正如我们这例[3]。而且,MDM的组成细胞呈大、圆、卵圆和多角形,伴清晰的细胞轮廓,丰富的毛玻璃样嗜酸性胞浆,圆的空泡状核有显著嗜酸性核仁。偶尔出现双核,但尽管细胞异型性和间变性显著,核分裂却少见[1-3]。胞浆通常在核周更致密、更深染,而周边部较透亮[5]。细胞排列成吻合的片状或小簇状,隔以纤维性间质或疏松水肿的间质。由Talerman等[6]1985年报道第一例13岁女孩的MDM时作了组织学描述,和我们这例一样,最初误诊为弥漫性假肿瘤样蜕膜病。
我们这例MDM与弥漫性假肿瘤样蜕膜病的混淆,本来可以通过仔细研究大体和镜下特点而避免。大体上,蜕膜病通常发生于妊娠期,但也可见于月经初潮前后和绝经期前后,在腹膜表面呈小而分散的结节或赘生物,而不是大而坚硬的斑块和结节。然而,高度增生的蜕膜反应偶尔能引起大块的假肿瘤样病变,可见坏死和细胞多形性[7]。广泛的腹腔累犯和存在腹水,不支持蜕膜病的诊断。镜下,蜕膜病的片状蜕膜细胞存在于结缔组织内,通常不像间皮瘤那样影响其表面。这两种病变的细胞都有大量胞浆,但核明显不同。蜕膜细胞的核较小,有深染的粗块状染色质,而间皮瘤细胞的核呈空泡状伴纤细的染色质、显著的核仁和偶见的核分裂[2,4,6]。存在经典间皮瘤的区域可导致诊断。在我们的这例,即使仔细取材,这样的区域也未观察到。
免疫组化对这两种病变的区分似乎作用不大。Nascimento等[1]认为蜕膜样细胞CK阴性有意义;然而,最近Healthy等的研究发现30%的盆腔外蜕膜病呈CK(AE1/3和CAM5.2)阳性。最近认为CK5/6是敏感和相对特异性的间皮瘤标记,特别是呈强而弥漫的着色时[3]。我们这例仅散在的肿瘤细胞呈CK5/6阳性。Calretinin是间皮瘤敏感而相对特异性的标记物,在我们这例也仅有散在的肿瘤细胞表达。Riera等[9]发现calretinin缺乏敏感性且特异性小。事实上,Shia等[5]报道仅2/5病例呈calretinin阳性,Orosz等[10]报道此抗体呈局灶阳性。这些病例的诊断是依据电镜研究。存在无数的胞浆内中间丝,或弥漫或束状分布,可能是蜕膜样组织学表现的超微结构基础[5]。
从预后角度看,MDM为高度恶性,平均生存期7.33月(范围1-22月)[5]。最近对女性腹膜间皮瘤的一项研究[11]发现40%患者的生存期超过4年。我们这例的预后差,可证实本病特殊的侵袭性特点。
我们这例相似于以往报道的发生于年轻女性MDM病例。我们提议将MDM的临床病理亚型与蜕膜样恶性间皮瘤亚型区分开,后者发生于较年老者的胸膜和腹膜,有石棉暴露史。进一步更多病例研究,将有助于更全面地描述这一罕见间皮瘤亚型的临床和病理特征。
总之,我们报道这例41岁女性剖宫产后6周发生的MDM,最初误诊为假肿瘤样蜕膜病。此例强调病理学家需要了解恶性间皮瘤的这一亚型,以避免误诊为良性病变。我们提出一个观点,即MDM可能仍代表上皮样间皮瘤的一个独特亚型,伴特殊的临床和病理特征。

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
文献图片放大:
图1 大的多角形细胞有丰富的嗜酸性胞浆,细胞轮廓清晰,有一胞浆周围空白区。核多形性,空泡状染色质,单个显著核仁。罕见核分裂。(HE400X)
图2 肿瘤细胞侵犯真皮,隔以透明变性区。(HE100X)
图3 肿瘤细胞侵犯肠粘膜下层。(HE50X)
图4 肿瘤细胞CK(KL1)强阳性。(200X)
图5 仅散在肿瘤细胞呈CK5/6阳性。(200X)
图6仅散在肿瘤细胞呈calretinin阳性。(400X)

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
-
本帖最后由 于 2007-02-28 19:06:00 编辑
| 以下是引用hechn 在2007-1-18 8:06:00的发言: 腹膜间皮蜕模样变。 |
(根据常规组织学图像,这是一例恶性蜕膜样间皮瘤。它通常发生于较年轻女性的腹膜,常用的间皮标记物(如calretinin和CK5/6)仅呈局灶阳性。预后很差。网上有几篇可用的参考文献,最近一例报道如下:
http://arpa.allenpress.com/arpaonline/?request=get-document&doi=10.1043%2F1543-2165(2005)129%3C403:MDMADC%3E2.0.CO%3B2
abin译)

聞道有先後,術業有專攻