| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 2012年第38期——双侧卵巢肿块(已点评)
53 y/f with bilateral adnexal masses and anterior abdominal wall nodule and peritoneal effusion. Regular CT examination showed bilateral ovarian masse measuring 10 and 8 cm, respectively; lung negative, pancrease, gastric negative findings also. Patient has no previous malignant history.
《永恒爱恋老师友情帮助翻译》:女,53岁,双附件巨大肿块,之前有腹部质硬结节伴腹膜渗出物;CT检查示双侧附件巨大肿块,大小分别约为10cm和8cm,肺、胰腺、胃均无异常发现,患者无恶性肿瘤病史。
Core biopsy was performed for anterior andominal wall nodule.
行腹部质硬结节细针穿刺活检
Three core biopsy specimen showed benign fibroadipose tissue. Only one core demonstrate focal epithelial lining.
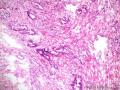
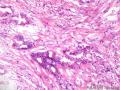
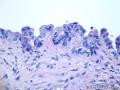
See the photos:
见图:
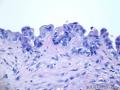
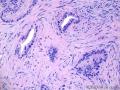
40x
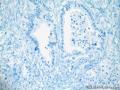
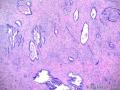
100x
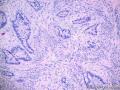
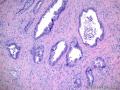
200x
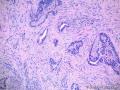
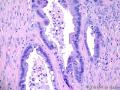
400x
Please descript
请描述
1. Your analysis and impression for this core biopsy
1、您对此穿刺活检标本的分析和看法
2. If you want to order some stains, what stains will you order? Only three unstained slides are avaiable due to the scant tissue.
2、如果您觉得需要做免疫组织化学染色,会选择哪些标记,剩余的组织只可用来做三张染色。
本例点评:赵澄泉老师
(以下由:蔷薇老师友情帮助翻译!)53岁女性,双侧附件肿块,前腹壁结节,有腹水。常规CT检查显示双侧卵巢肿块分别为10cm及8cm;双肺、胰腺、胃未见特殊。患者无恶性肿瘤病史。
行前腹壁肿块粗针穿刺活检。
三条组织呈良性纤维脂肪组织。仅1条组织见局灶上皮被覆。
如图片所示:
请给出如下所述。
1 您对该活检的分析及诊断
2 如果需特殊染色,请列出那些特殊染色。由于组织有限,仅有3张白片。
点评专家:赵澄泉(113楼 链接:>>点击查看<< )
获奖名单:雅马哈(1楼 链接:>>点击查看<< )
-
本帖最后由 筷子 于 2013-05-09 18:28:41 编辑
最终诊断:
转移性高分化粘液性腺癌。
IHC:CK7+,CK20-/+,ER-PR-,PAX8-,CDX2-,SMAD4少数核着色,结果符合转移性卵巢高分化粘液性腺癌。
理由:TTF-1阴性排除肺和甲状腺原发,calretinin阴性排除间皮瘤(实际上形态也不像)。在CK7+和CK20-/+的肿瘤谱中,ER-PR-排除乳腺癌,CDX2排除大多数消化道癌。SMAD4阳性定位于胞质,故本例判读为阴性,排除胰腺癌。PAX8表达于大多数苗勒肿瘤,但考虑到本例双侧卵巢有大肿块,CK7+和CK20-/+仍符合卵巢粘液癌。
SMAD4没有使用经验。
IHC:CK7+,CK20-/+,ER-PR-,PAX8-,CDX2-,SMAD4少数核着色,结果符合转移性卵巢高分化粘液性腺癌。
Why did you get this conclusion
-
本帖最后由 abin 于 2012-10-13 21:54:07 编辑
Now you have all information for this case.
Please give your final diagnosis for the abdominal nodule second biopsy.
Also you need to mention the reasons to support your diagnosis
(现在提供了本例的所有信息。
请给出腹壁结节第二次活检的最终诊断。
也需要写下诊断的理由。
abin译)
-
本帖最后由 abin 于 2012-10-13 19:30:45 编辑
Why is malignant?
The biopsy was from abdominal wall nodule. The glands are irregular shaped with mildly to moderately atypical cells. Clearly they are not like endometriosis. Many atypical glands in this location should be metastatic adenocarcinoma. The location is very important. If this is an ovarian biopsy, it would be difficult to determine the nature of the lesion.
About the origin, we cannot make sure the carcinoma is from ovary or others. If the malignant glands are like high grade serous carcinoma, we can say mostly it is a gynecological high grade serous carcinoma. However, no one can be sure the orgin based on the one frozen section in this case.
Now we know that focal area of atypicl epithelial cells in one of the three cores (first core biopsy specimen) was part of the malignant glands.
Should the patient have BSO procedure based on the abdominal nodulebiopsy frozen result? It is better to wait for the final result from the biopsy specimen. If it is a non-gynecological tumor with extensive metastases, the BSO procedure may not be necessary.
Our gynecology oncologist will wait for the final report, then determine the next step.
(为什么是恶性?
活检标本部位来自腹壁结节。腺体形状不规则伴轻-中度非典型细胞。很明显,它们不像子宫内膜异位症。这个部位出现许多非典型腺体应该是转移性腺癌。部位非常重要。如果这是卵巢活检,就很难确定病变性质。
现在我们知道,三个粗针穿刺活检部位中有一处发现小灶区域有非典型上皮细胞(第一次粗针穿刺活检标本),它是恶性腺体的一部分。
患者是否需要根据腹腔结节活检标本的冰冻报告进行双侧卵巢和输卵管切除术?最好等待活检标本的最终报告。如果它是非妇科肿瘤伴有广泛转移,可能不需要双侧卵巢和输卵管切除术。
我们的妇科肿瘤医师会等待最终的病理报告,然后决定下一步处理。
abin译)
-
本帖最后由 abin 于 2012-10-13 19:19:21 编辑
Our frozen report:
Malignant.
Metastatic adenocarcinoma
The origin cannot be determined in frozen. It can be from ovary or others. Immunostains will be performed in the permanent sections for the origin
(我们的冰冻报告:
恶性肿瘤。
转移性腺癌。
冰冻切片不能确定原发部位。它可能来自卵巢或其他部位。将对石蜡切片做免疫染色协助判断原发部位。
abin译)
-
本帖最后由 abin 于 2012-10-07 20:29:44 编辑
In the third day, the gynecologist did another biopsy from the abdominal nodule:
Grossly the specimen consisted of a 2.2x2.0x0.6 cm portion of tan-pink soft tissue. The specimen was bisected and on half was submitted for intraoperative interpretation--frozen.
Above are three photos from frozen sections.
第三天,妇科医生对腹部结节再次活检:
大体:标本为2.2x2.0x0.6 cm褐红色软组织。标本对剖,一半做冰冻切片。
以上三图是冰冻切片。(abin译)
-
本帖最后由 abin 于 2012-10-07 20:25:10 编辑
The purposes of the biopsy:
1. Nature of the lesion: benign or malignant
2. origin: ovary or other organ
Clinicians hope to know above information to determine the next procedure. If the lesion is not from the ovary, but metastatic from other organ, the BSO prodedure may not be needed.
Based on the morphologic and staining feature, I felt most likely it is malignant tumor. However, I cannot be 100% sure. Also I cannot determine if it is ovarin primary or not. So I cannot make a definitive diagnosis.
Above is my thought. It does not mean it is a standard diagnosis
译文:
活检目的:
1、判断病变的性质:良性或恶性
2、判断病变的起源部位:卵巢或其他器官
临床医生希望知道上述信息,以确定后续处理。如果病变不是起源于卵巢,而是起源于其他器官,可能不需要BSO手术(双侧输卵管、卵巢切除术)
根据形态学和免疫染色,我觉得它很可能是恶性肿瘤。然而,我没有100%把握。我也不能确定它是否卵巢原发。因此我不能作出明确诊断。
以上是我的考虑,并不表示它是标准诊断。(abin译)
-
本帖最后由 abin 于 2012-10-07 20:20:22 编辑
I signed out the case as the following
Abdominal nodule, right lower quadrant, needle core biopsy:
Fibroadipose tissue with focal mucinous-like epithelial lining showing cytological atypia.
Comment:
Three needle core biopsy specimen shows fibroadipose tissue. Only focal lining with mucinous-like epithelium in present (1mm) in one slide. The glandular epithelial cells show nuclear atypia. Immunostains were performed. The glandular cells demonstrate increased proliferative index and are negative for PAX8, CDx2. No more staining results can be obtained becuase the glandular epithelialc cells are absence in the deep-cut levels. No conclusive diagnosis can be made due to the scant tissue. More tissue is needed for further evaluation.
译文:
我签发的这例报告如下:
腹部结节,右下方,粗针穿刺活检:纤维脂肪组织伴粘液样上皮被覆显示细胞学非典型性。
评注:
三条粗针穿刺活检组织显示纤维脂肪组织。仅有局灶被覆粘液样上皮(1张切片上1mm)。腺样上皮细胞显示核非典型性。免疫染色,腺细胞增殖指数增高,PAX8和CDX2均阴性。因其余切片中无腺上皮细胞故未做更多免疫染色。由于有效组织少,不能明确诊断。需要更多组织进一步评估。(abin译)
-
本帖最后由 abin 于 2012-10-07 21:35:33 编辑
In primary neoplasms, PAX 8 was expressed by 194 of 240 (89%) renal cell neoplasms, by 238 of 267 (89%) Müllerian-type neoplasms, by 65 of 65 (100%) thyroid follicular cell neoplasms, by 8 of 8 (100%) nephrogenic adenomas, and by 17 of 17 (100%) lymphomas.
In fact no any stain has 100% senstivity snd specificity
译文:
PAX8在原发肿瘤的表达率:肾细胞肿瘤194/240 (89%),苗勒型肿瘤238/267 (89%) ,甲状腺滤泡上皮肿瘤65 /65 (100%),肾腺瘤8 /8 (100%),淋巴瘤17 / 17 (100%)
实际上没有任何抗体的敏感性和特异性达到100%
PAX 8 expression in non-neoplastic tissues, primary tumors, and metastatic tumors: a comprehensive immunohistochemical study.
Source
Departments of Pathology, The Methodist Hospital, Houston, TX 77030, USA.
Abstract
PAX 8 is a transcription factor that is essential for embryonic development of the kidney, Müllerian organs, and thyroid. It may also have a role in tumor development in these organs. The diagnostic utility of PAX 8 has not been comprehensively studied. Formalin-fixed, paraffin-embedded tissue samples for non-neoplastic tissues (n=1601), primary neoplasms (n=933), and metastatic neoplasms (n=496) were subjected to PAX 8 immunostain. In non-neoplastic tissues, PAX 8 was consistently noted in glomerular parietal epithelial cells, renal collecting ductal cells, atrophic renal tubular epithelial cells regardless of nephronic segments, and epithelial cells of the endocervix, endometrium, fallopian tube, seminal vesicle, epidydimis, thyroid, pancreatic islet cells, and lymphoid cells. PAX 8 was not seen in the rest of the tissue samples. In primary neoplasms, PAX 8 was expressed by 194 of 240 (89%) renal cell neoplasms, by 238 of 267 (89%) Müllerian-type neoplasms, by 65 of 65 (100%) thyroid follicular cell neoplasms, by 8 of 8 (100%) nephrogenic adenomas, and by 17 of 17 (100%) lymphomas. Weak focal staining was noted in 5 of 12 (42%) cases of parathyroid hyperplasia/adenoma and in 6 of 17 (35%) well-differentiated neuroendocrine tumors of the pancreas. PAX 8 was not seen in other neoplasms. In metastatic neoplasms, PAX 8 was expressed by 90 of 102 (88%) metastatic renal cell carcinomas, by 57 of 63 metastatic Müllerian tumors (90%), and by 6 of 6 metastatic papillary thyroid carcinomas (100%). There was also weak focal staining for 1 of 15 metastatic small cell carcinomas and for 1 of 9 metastatic well-differentiated neuroendocrine carcinomas. PAX 8 was not seen in other metastatic neoplasms. It can be successfully identified in routinely processed tissue samples, and its expression is mostly nuclear. PAX 8 expression in non-neoplastic mature tissues is limited to the organs, the embryonic development of which depends on this transcription factor. This tissue/cell-specific expression is maintained during both neoplastic transformation and metastasis. PAX 8 is a sensitive and specific marker for tumors of renal, Müllerian, or thyroid origin in both primary and metastatic sites.
PAX8是用于鉴别卵巢浆液性肿瘤和恶性间皮瘤可信赖的标致记物,其在卵巢将夜性肿瘤中一般强阳性表达,而在间皮性肿瘤中一般不表达。结合CDX2阴性,几乎可以肯定本例为卵巢原发的浆液性上皮-间质肿瘤。HE形态示肿瘤性上皮虽层次不多,也无明确浸润,但细胞异型性大,Ki-67增值指数高,提示其至少为为高级别性上皮内肿瘤。由于是穿刺活检小标本,而双附件肿瘤巨大,故不能排除高级别浸润性浆液性癌可能,应该建议临床行肿瘤扩大切除术,待术中快速或术后病理进一步明确分级及分期。
Do you think PAX8 positive or negative?