| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 2012年第38期——双侧卵巢肿块(已点评)
53 y/f with bilateral adnexal masses and anterior abdominal wall nodule and peritoneal effusion. Regular CT examination showed bilateral ovarian masse measuring 10 and 8 cm, respectively; lung negative, pancrease, gastric negative findings also. Patient has no previous malignant history.
《永恒爱恋老师友情帮助翻译》:女,53岁,双附件巨大肿块,之前有腹部质硬结节伴腹膜渗出物;CT检查示双侧附件巨大肿块,大小分别约为10cm和8cm,肺、胰腺、胃均无异常发现,患者无恶性肿瘤病史。
Core biopsy was performed for anterior andominal wall nodule.
行腹部质硬结节细针穿刺活检
Three core biopsy specimen showed benign fibroadipose tissue. Only one core demonstrate focal epithelial lining.
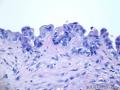
See the photos:
见图:
40x
100x
200x
400x
Please descript
请描述
1. Your analysis and impression for this core biopsy
1、您对此穿刺活检标本的分析和看法
2. If you want to order some stains, what stains will you order? Only three unstained slides are avaiable due to the scant tissue.
2、如果您觉得需要做免疫组织化学染色,会选择哪些标记,剩余的组织只可用来做三张染色。
本例点评:赵澄泉老师
(以下由:蔷薇老师友情帮助翻译!)53岁女性,双侧附件肿块,前腹壁结节,有腹水。常规CT检查显示双侧卵巢肿块分别为10cm及8cm;双肺、胰腺、胃未见特殊。患者无恶性肿瘤病史。
行前腹壁肿块粗针穿刺活检。
三条组织呈良性纤维脂肪组织。仅1条组织见局灶上皮被覆。
如图片所示:
请给出如下所述。
1 您对该活检的分析及诊断
2 如果需特殊染色,请列出那些特殊染色。由于组织有限,仅有3张白片。
点评专家:赵澄泉(113楼 链接:>>点击查看<< )
获奖名单:雅马哈(1楼 链接:>>点击查看<< )
-
本帖最后由 筷子 于 2013-05-09 18:28:41 编辑
Based on the requirement from the patient or clinician, the Tissue of Origin Test (from block) was performed by Pathwork Diagnostics (Redwood City, CA).
A. Most likely tissue of origin: PANCREAS (Degree of confidence: MODERATELY HIGH; Similarity Score-SS 41.6) (see note).
B. Tissues ruled out: Sarcoma, Breast, Non-Small Cell Lung, Bladder, Thyroid, Melanoma, Kidney, Hepatocellular, Hon-Hodgkin Lymphoma, Testicular Germ Cell, Prostate.
TISSUE OF ORIGIN TEST
TISSUE Similarity score:
Pancreas 41.6
Gastric 25.6
Colorectal 13.5
Ovarian 7.3
Sarcoma 3.8
Breast 1.8
Non-Small Cell Lung 1.0
Bladder 1.0
Thyroid 1.0
Melanoma 0.8
Kidney 0.8
Hepatocellular 0.7
Non-Hodgkin Lymphoma 0.6
Testicular Germ Cell 0.4
Prostate 0.4
NOTE:
An off-panel tumor type, such as cholangiocarcinoma and esophageal adenocarcinoma, CANNOT BE EXCLUDED by the Test.
Some one please help to translate the report about the tissue of origin test into chinese
The following introduction is from the original report.
The Tissue of Origin Test, developed by Pathwork Diagnostics, measures the expression pattern, comprising more than 1500 genes, in a tumor to compare it to expression patterns of a panel of 15 known tumor types, representing 58 morphologies and covering 90% of all solid tumors. It produces a report with an objective score for each potential tissue (1,2). The test uses a proprietary Pathchip microarray and runs on the proven Affymetrix GeneChip System. According to the Pathwork Diagnostics, this test demonstrated 89% positive percent agreement (akin to sensitivity) with available diagnoses, and greater than 99% negative percent agreement (akin to specificity) in specimens that had previously been identified with existing methods as being among the 15 tumor types on the panel (3).
1. Dumur CI, Lyons-Weiler M, Sciulli C, et al. Interlaboratory performance of a microarray-based gene expression test to determine
tissue of origin in poorly differentiated and undifferentiated cancers. J Mol Diagn. 2008;10:67-77.
2. Monzon FA, Lyons-Weiler M, Buturovic LJ, et al. Multicenter validation of a 1,550-gene expression profile for identification of
tumor tissue of origin. J Clin Oncol. 2009;27:2503-8.
3. Pillai R, Deeter R, Rigl CT, et al. Validation and reproducibility of a microarray-based gene expression test for tumor
identification in formalin-fixed, paraffin-embedded specimens. J Mol Diagn. 2011;13:48-56.
Based on the requirement from the patient or clinician, the Tissue of Origin Test (from block) was performed by Pathwork Diagnostics (Redwood City, CA).
A. Most likely tissue of origin: PANCREAS (Degree of confidence: MODERATELY HIGH; Similarity Score-SS 41.6) (see note).
B. Tissues ruled out: Sarcoma, Breast, Non-Small Cell Lung, Bladder, Thyroid, Melanoma, Kidney, Hepatocellular, Hon-Hodgkin Lymphoma, Testicular Germ Cell, Prostate.
TISSUE OF ORIGIN TEST
TISSUE Similarity score:
Pancreas 41.6
Gastric 25.6
Colorectal 13.5
Ovarian 7.3
Sarcoma 3.8
Breast 1.8
Non-Small Cell Lung 1.0
Bladder 1.0
Thyroid 1.0
Melanoma 0.8
Kidney 0.8
Hepatocellular 0.7
Non-Hodgkin Lymphoma 0.6
Testicular Germ Cell 0.4
Prostate 0.4
NOTE:
An off-panel tumor type, such as cholangiocarcinoma and esophageal adenocarcinoma, CANNOT BE EXCLUDED by the Test.
-
本帖最后由 abin 于 2012-11-24 00:51:30 编辑
Ovarian metastases of pancreaticobiliary tract adenocarcinomas: analysis of 35 cases, with emphasis on the ability of metastases to simulate primary ovarian mucinous tumors.
Source
Departments of Pathology, The Johns Hopkins University School of Medicine and Hospital, Baltimore, MD 21231, USA.
Abstract
Metastatic mucinous carcinomas in the ovary are readily recognized when they show characteristic features, including bilateral involvement, only moderate tumor size, surface and superficial cortical involvement, nodular growth, and an infiltrative pattern. However, it is well established that some metastatic mucinous carcinomas can simulate primary ovarian mucinous tumors grossly and microscopically. Metastatic pancreaticobiliary tract adenocarcinomas present a particular diagnostic challenge due to their ability to exhibit borderline-like and cystadenomatous growth patterns, which can be misinterpreted as underlying primary ovarian precursor tumors and can be erroneously used to support interpretation of the carcinomatous components as arising from these purported precursors within the ovary. Thirty-five cases of metastatic pancreaticobiliary tract adenocarcinomas were analyzed. The mean patient age was 58 years (median, 59 y; range, 33 to 78 y). In 15 cases (43%), the pancreaticobiliary tract and ovarian tumors presented synchronously and in 2 cases (6%) the ovarian tumors presented earlier as the first manifestation of the disease. Ovarian tumors were bilateral in 31 cases (89%). Mean and median tumor sizes were 10.6 and 9.5 cm, respectively (range, 2.5 to 21.0 cm). Nodularity was present in 22 cases (63%) and surface involvement was identified in 14 cases (40%). An infiltrative growth pattern was present at least focally in 28 cases (80%), accompanied by borderline-like and/or cystadenomatous areas in 17 (49%) cases and as the exclusive pattern in 11 cases (31%). Conversely, borderline-like and cystadenomatous patterns were identified in 24 cases (69%) and as the exclusive patterns (either pure or combined with one another) in 7 cases (20%). Dpc4 expression was lost in 20 of 33 tumors analyzed (61%). Of 25 patients with follow-up, 23 patients had died of disease (mean/median time, 9/6 mo; range, 1 to 39) and 2 patients were alive with disease (at 1 and 25 mo). Frequent bilateral ovarian involvement, moderate tumor size, nodularity, and infiltrative patterns are useful features for identifying these ovarian tumors as metastatic. However, many tumors exhibit borderline-like and cystadenomatous patterns that, when dominant and combined with synchronous presentation, make recognition as metastases an ongoing challenge. Loss of Dpc4 expression provides the most useful immunohistochemical evidence for establishing the pancreaticobiliary tract as the most likely source of these metastatic mucinous carcinomas in the ovary.(卵巢转移性粘液癌中确定胰胆管是最可能起源部位的最有用的免疫组化证据是Dpc4阴性)
-
本帖最后由 abin 于 2012-11-24 00:45:45 编辑
In addition I would like to thank all people who read or participated the discussion for this case, especially Abin who spent a lot of time to analyze the case and show many useful references.
(另外感谢所有浏览过或参加讨论的人,特别是abin花费了大量时间分析并提供了许多有用的参考资料)
-
本帖最后由 abin 于 2012-11-24 00:44:38 编辑
最终诊断:腹壁结节转移性管状腺癌,结合HE形态及免疫组化结果提示来源于胰腺可能,建议临床进一步检查。(虽然CT检查示双侧附件巨大肿块,大小分别约为10cm和8cm,肺、胰腺、胃均无异常发现,患者无恶性肿瘤病史。)
1.形态:在纤维组织增生性间质中,管状/导管样腺体浸润,这种形态常见来源:胃肠道、肺、乳腺、胰腺、胆管、及卵巢或宫颈腺癌等。
2.临床:双侧卵巢肿物(大小分别约为10cm和8cm)、粘液腺癌样首先考虑转移(非卵巢原发)。
3.IHC:CK7+,CK20-/+,ER-PR-,PAX8-,CDX2-,SMAD4—:
理由:在CK7+和CK20-/+的肿瘤谱中,TTF-1阴性排除肺,calretinin阴性排除间皮(实际上形态也不像),ER-PR-排除乳腺癌,CDX2进一步排除结直肠。SMAD4为抑癌基因,本例为阴性(注意腺腔内核阳性可能非上皮细胞),要知道其在55%胰腺癌中失活,在其他癌如胃肠道、乳腺等也可失活,而在卵巢粘液性腺癌一般会有表达,假设结节是卵巢来的,SMAD4-提示胰腺可能。PAX8表达于大多数苗勒肿瘤等(见赵老师提供的文献,不说了)。
一个悲催的现实:一些卵巢转移的粘液腺癌被诊断原发粘液癌。标准,方法该如何?
I would like to mention that 96298 was the first one to have reasonable and correct diagnosis and interpretation for this case.
(我也注意到96298是第一位得出合理、正确诊断和解释者)
-
本帖最后由 abin 于 2012-11-24 00:42:52 编辑
Before I signed out the case, I had a long discussion with the gynecologist. Two days late, the gynecologist sent me an email to show the thanks for my analysis for the case.
The patient had an intensive CT scan for the abdoman and a 2 cm mass was identified in the pancrease. So most likely the pancrease is the primary site of the tumor with extensive metastasis.
(在签发报告之前,我也妇科医生进行了长时间讨论。两天后,妇科医生发邮件给我表示感谢。
患者做了腹部增强CT,发现胰腺2cm肿块。因此很可能胰腺是原发部位,伴广泛转移)
-
本帖最后由 cqzhao 于 2012-12-21 11:22:22 编辑
Now I report you how I signed the case finally. My report is just for your reference.
(现在提供我是如何签发最终报告的,仅供参考。
Final diagnosis: 最终诊断:
Anterior abdominal wall, biopsy- 前腹壁活检-
Metastatic adenocarcinoma. 转移性腺癌。
Comment:评注:
This is a challenge case. The biopsy specimen shows malignant glands infiltrating the dense stroma with obvious desmoplastic reaction. The glands demonstrate irregular shape and the tumor cells with some mucinous features. Multiple immunostains were performed. The metastatic tumor cells are positive for CK7, BerEP4, and negative for CK20, CDX2, TTF-1, ER, PR, PAX8, SMAD4(DCP4), mammaglobin, GCDFP, and calretinin. Overall the stain results and cytomorphologic features of the tumor do not support the gyncological (negative for ER, PR, PAX8, SMAD4), colonic (negative for CK20, CDX2, positive for CK7), lung (negative for TTF-1), breast (negative for mammaglobin, GCDFP, ER, PR), mesothelial (positive for BerEP4, negative for calretinin) primaries. The most significant IHC finding is that the tumor cells are completely negative for SMAD4. The tumors in most organs are positive for SMAD4. One study indicated that 61% of the ovarian metastases from pancreaticobiliary tract show loss of SMAD4 expression (Merident, et al. Am J Surg Pathol 2011;35:276-288). Other studies showed that 20-30% colonic carcinomas are negative for SMAD4. Overall I favor that the tumor is a pancreaticobliary tract primary based on the IHC and morphological features, even though other primary cannot be completely excluded. Clinical correlation with imaging is suggested.
I discussed the case with Dr. xxxx xx at 4:00 PM, September 10, 2012
(本例具有挑战性。活检标本显示恶性腺体浸润致密间质伴明显的促纤维性间质反应。腺体呈不规则形状,肿瘤细胞具有部分粘液特征。检测了多种免疫染色。转移性肿瘤呈CK7和BerEP4阳性,而CK20, CDX2, TTF-1, ER, PR, PAX8, SMAD4(DCP4), mammaglobin, GCDFP和calretinin均阴性。总体上,免疫染色结果和细胞形态学特征不支持的原发部位包括妇科(ER, PR, PAX8, SMAD4均阴性)、结肠( CK20和 CDX2阴性而CK7阳性)、肺(TTF-1阴性)、乳腺(mammaglobin, GCDFP, ER, PR均阴性)或间皮(BerEP4阳性而calretinin阴性)。最有意义的发现是SMAD4完全阴性。大多数器官肿瘤呈SMAD4阳性。一项研究中提出61%来自胰胆管的卵巢转移癌为SMAD4阴性。其他研究显示20-30%结肠癌呈SMAD4阴性。根据免疫组化和形态学特征,我总体上倾向于肿瘤是胰胆管原发,但其他原发部位不能完全排除。建议结合临床和影像学考虑。
我与XXX医生在某个时间讨论了本例。)
-
本帖最后由 abin 于 2012-11-24 00:27:38 编辑
Sorry to delay for so long time.
A lot of pepole above have excellent explanation and discussion for this case. Thanks.
I have mentioned and discussed our diagnosis for the first core biopsy and frozen result of second biopsy before.
(抱歉延期。
很多人对本例提供了很好的分析和讨论,谢谢。
我在前面已经提到并讨论过第一次粗针穿刺活检和冰冻诊断。)
-
本帖最后由 abin 于 2012-10-22 19:58:35 编辑
I will be in China for three weeks and will put here my diagnosis here when i come back the usa. You have time to consider the case if you like to.
Since i put the photos from second biopsy and staining, there are very few people who writing your dx or comment here. Is it too easy for most of you?
我将在北京三个星期,回到美国时提供诊断。如果愿意,你们有时间考虑。
自从上传了第二次活检和染色的照片,很少人写了诊断或评论。是不是大多数人觉得太简单?
最终诊断:腹壁结节转移性管状腺癌,结合HE形态及免疫组化结果符合来源于胰腺转移,建议临床再查查。--怎么会有这个结论?(虽然CT检查示双侧附件巨大肿块,大小分别约为10cm和8cm,肺、胰腺、胃均无异常发现,患者无恶性肿瘤病史。)
1.形态:在纤维组织增生性间质中,管状/导管样腺体浸润,这种形态常见来源:胃肠道、肺、乳腺、胰腺、胆管、及卵巢或宫颈腺癌等。
2.临床:双侧卵巢肿物(大小分别约为10cm和8cm)、粘液腺癌样首先考虑转移(非卵巢原发)。
3.IHC:CK7+,CK20-/+,ER-PR-,PAX8-,CDX2-,SMAD4—:
理由:在CK7+和CK20-/+的肿瘤谱中,TTF-1阴性排除肺,calretinin阴性排除间皮(实际上形态也不像),ER-PR-排除乳腺癌,CDX2进一步排除结直肠。SMAD4为抑癌基因,本例为阴性(注意腺腔内核阳性可能非上皮细胞),要知道其在55%胰腺癌中失活,在其他癌如胃肠道、乳腺等也可失活,而在卵巢粘液性腺癌一般会有表达,假设结节是卵巢来的,SMAD4-提示胰腺可能。PAX8表达于大多数苗勒肿瘤等(见赵老师提供的文献,不说了)。
一个悲催的现实:一些卵巢转移的粘液腺癌被诊断原发粘液癌。标准,方法该如何?
What percentage of colonic cancer cases are SMAD4 negative?