| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
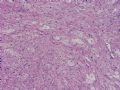
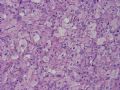
- NP (4) - WHO grade IV glioblastoma, granular cell variant
-
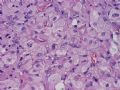
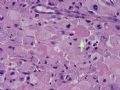
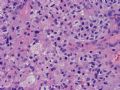
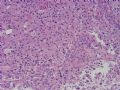
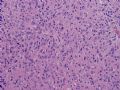
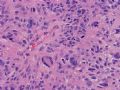
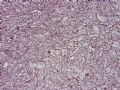
This is a resected supratentorial intra-axial focally enhancing brain tumor from a 50-year-old woman. Figures 1~5 are taken from the central portion of the resected tumor. Figures 6~12 are taken from the peripheral portion of the resected tumor. Figure 13 is taken from the interface between tumor and surrounding brain parenchyma. What is/are your diagnosis or your differential diagnoses? What stain(s) would help you?
标签:
-
本帖最后由 于 2006-11-08 11:16:00 编辑

聞道有先後,術業有專攻
×参考诊断
-
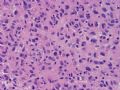
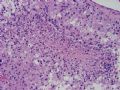
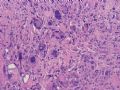
This is a rare case of WHO grade IV, granular cell variant of glioblastoma. The granular cells in this case are very prominent and occupy the central bulk of the resected tumor. They faithfully illustrate this variant of almost always high grade (WHO grade III~IV) astrocytoma. The granular cytoplasm is moderately positive on PAS stain (not shown), and there is very distinctive pericellular reticulin fibrils on silver stain. Intratumoral inflammatory infiltrates have been listed as a characteristic feature, but I have not seen enough of this variant to say this is true. There are many characteristic neoplastic astrocytes in the periphery of this resected tumor with features consistent with glioblastoma. This is usually the case, and astrocytomas consisting purely of granular cells are extremely rare. there is no quantitative criterion (?percentage of cells to be granular cells) for assigning an astrocytoma this particular variant. In general, I follow the 50% rule.
Differential diagnoses of this rare tumor include pleomorphic xanthoastrocytoma (PXA) with anaplastic features, giant cell variant of glioblastoma, benign granular cell tumor of dura/leptomeninges or of pituitary gland, macrophages or histiocytes (infarct, demyelinating lesion, Erdheim-Chester disease), and metastases (alveolar soft part sarcoma, renal cell carcinoma, adrenal cortical carcinoma). Perhaps the most critical key to rule these out is, as xiaohl pointed out earlier, is the anatomic location of the lesion. With resection specimens, these are not that difficult to distinguish. If, unfortunately, you do not have this important information and only have a small biopsy to examine, it can be very difficult to reach the correct diagnosis.
At first glance, the granular cells may appear histiocytic, but their malignant nature is evidenced by atypical nuclear features (size and shape variations with scattered very large and hyperchromatic nuclei, irregular nuclear shape, and occasional mitoses). Granular cell tumors (considered a special type of schwannomas) of dura/meninges are extremely rare. Granular cell tumor of pituitary gland and hypothalamus are also rare. These two tumors are benign and cells do not have malignant features. Like granular cell astrocytoma, PXA and giant cell glioblastoma show pericellular reticulin fibrils and, usually, prominent perivascular inflammation. The giant cells in these two tumors, however, are usually much larger in size with a much greater cellular size variation. PXA almost always occurs at a superficial cerebral cortical location. Giant cell glioblastomas usually contain very small neoplastic cells between giant cells. All these are helpful points.
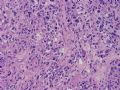
Nine month after gross tumor resection and post-surgical irradiation of tumor bed, the tumor was found to have recurred by MRI and a second resection was undertaken. The resected tissue shows a mitotically active and focally necrotic glioblastoma of the usual type (see Figures 1~4 below).

聞道有先後,術業有專攻
-
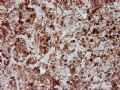
Figures 1~2 are taken from reticulin silver stain, with 1 from the center and 2 from the periphery of the tumor.
Figures 3~5 are taken from GFAP immunohistochemical stain, with 3 from the periphery, 4 from the interface, and 5 from the center of the tumor.
Figures 6~7 are taken from MIB-1 immunohistochemical stain, with 6 from the center and 7 from the periphery of the tumor.

聞道有先後,術業有專攻
| 以下是引用xiaohl 在2006-10-31 23:46:00的发言:The anatomic location of this tumor is very important for a accurate diagnosis. If this leision localized in the surfuce of cerebrum, PXA with anaplastic feature or a histocytic tumor is to be considered, but the intra-axial location, the relatively old age of the patient and the untypical histomorphology features don't support this diagnosis. If the leision localized intrasellarly and/or suprasellayly, I would prefer the diagnosis of granular cell tumor of the neurohypophysis. If the tumor arise from the parenchyma of the cerebrum, the diagnosis of giant cell glioblastoma must be considered. So, I think the exact location of this tumor is the utmost important for its correct diagnosis, then, some kinds of antibodies,such as GFAP,Ki67,NSE,SYN,S-100,CD68,α1-AT,and so on,will do some help for our diagnosis. |

聞道有先後,術業有專攻
| 以下是引用xiaohl 在2006-10-30 15:41:00的发言: I want to know the exact location of this tumor,Thanks a lot. |

聞道有先後,術業有專攻