| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
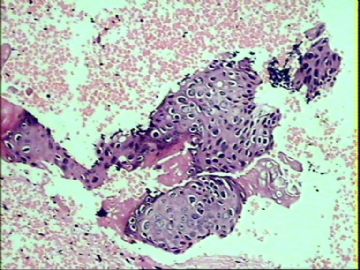
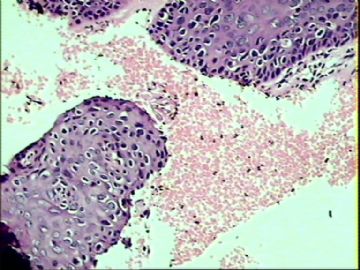
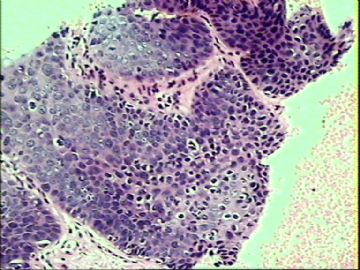
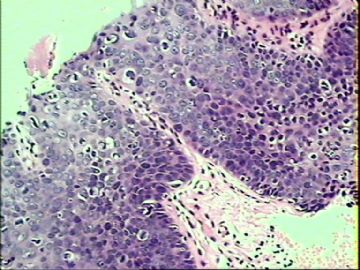
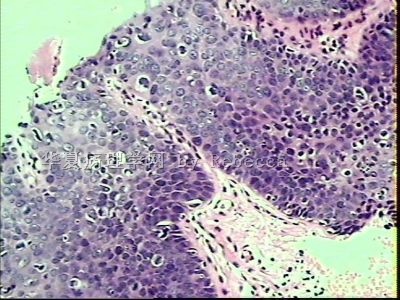
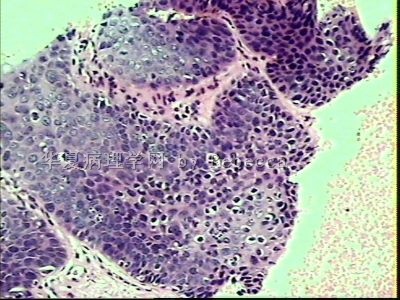
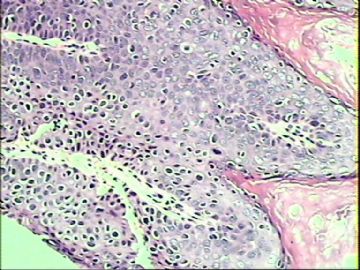
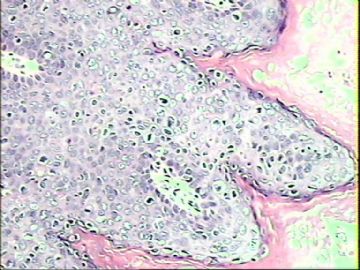
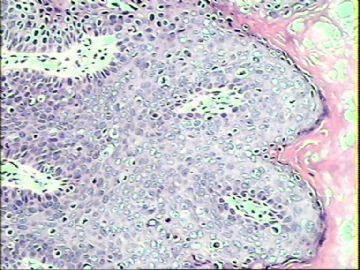
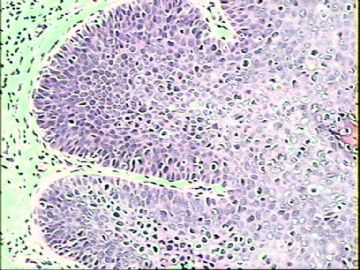
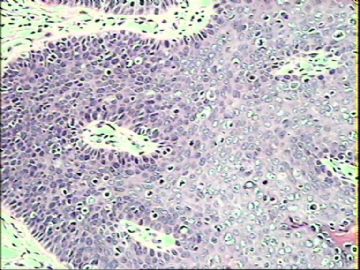
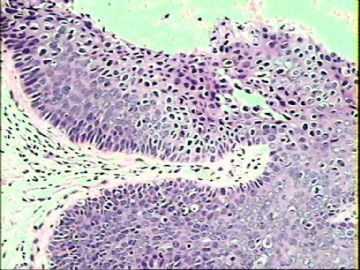
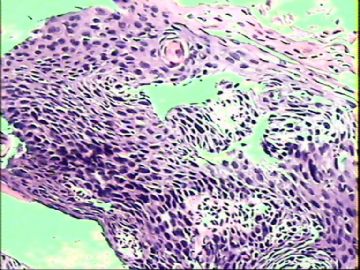
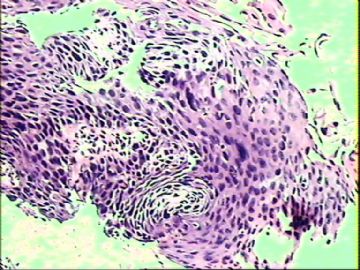
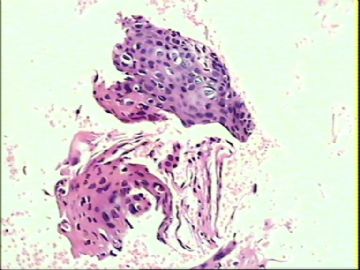
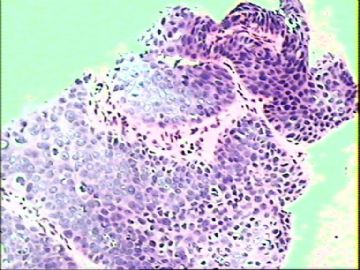
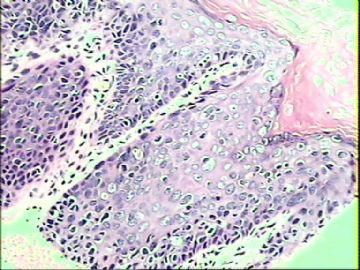
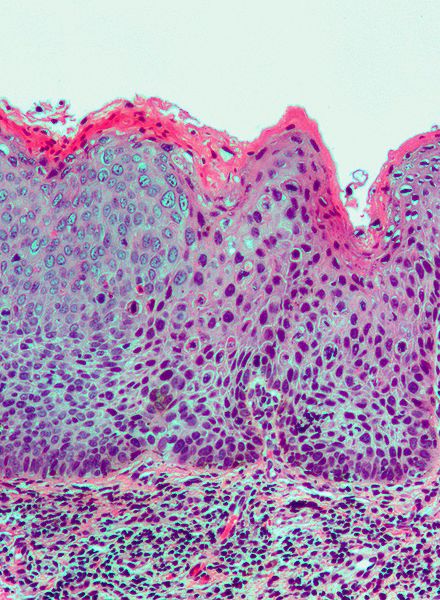
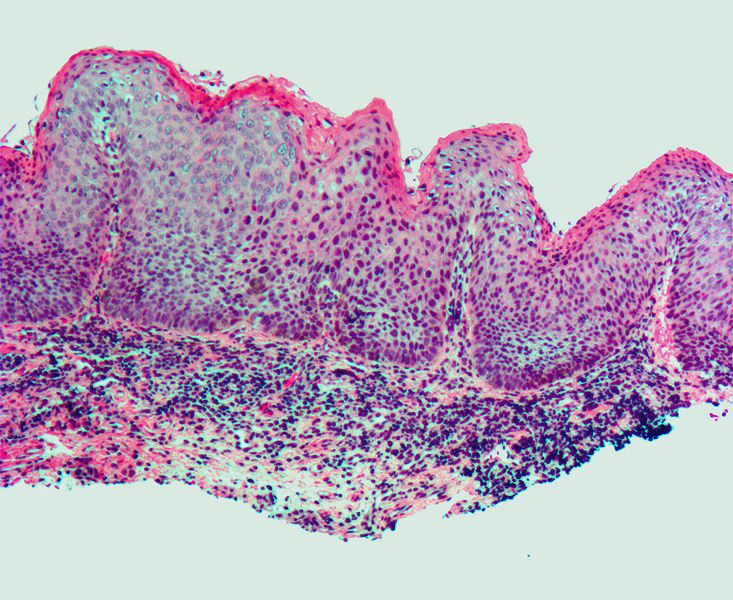
- ‘外阴白斑’活检1例(VINIII第二次手术标本病理会诊报告 2010-09-29)
归纳与小结
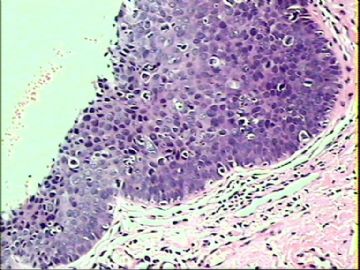
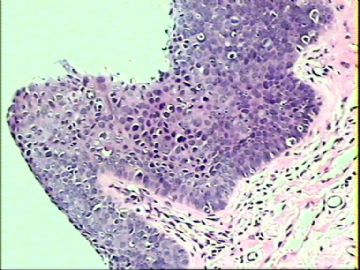
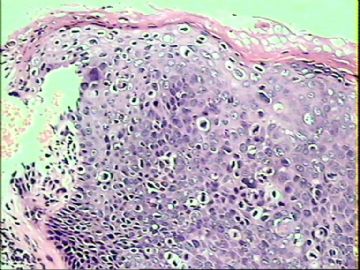
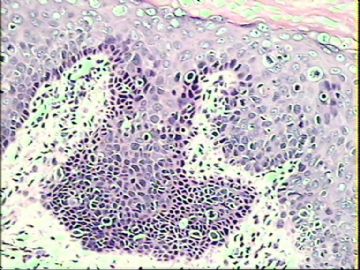
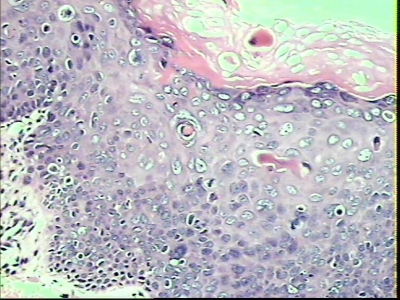
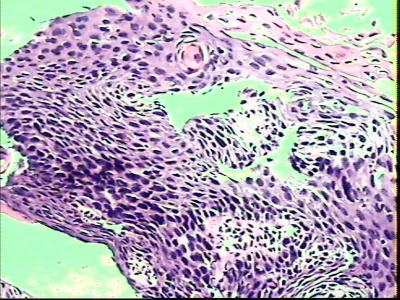
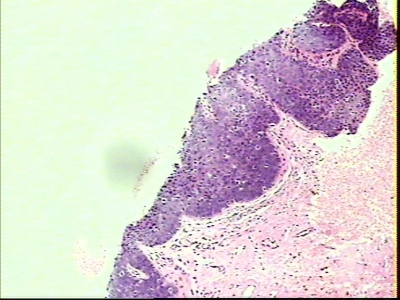
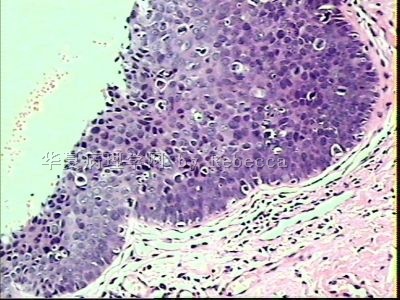
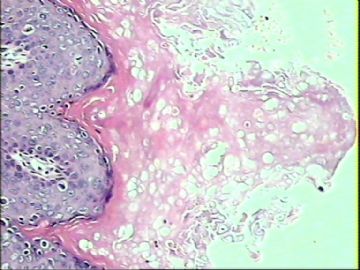
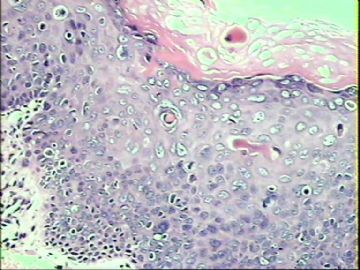
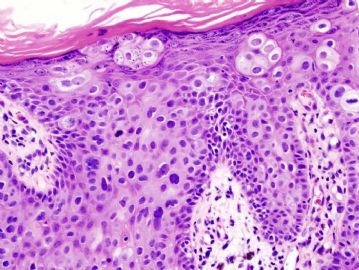
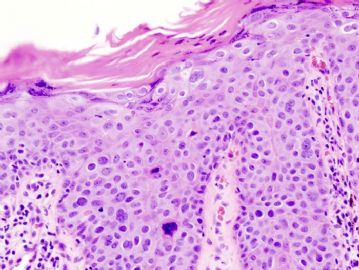
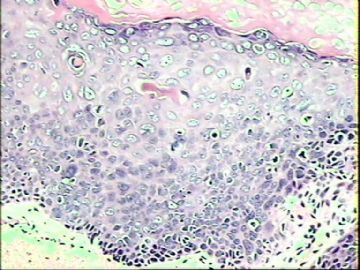
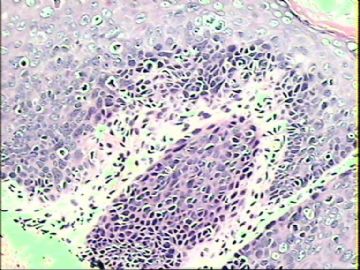
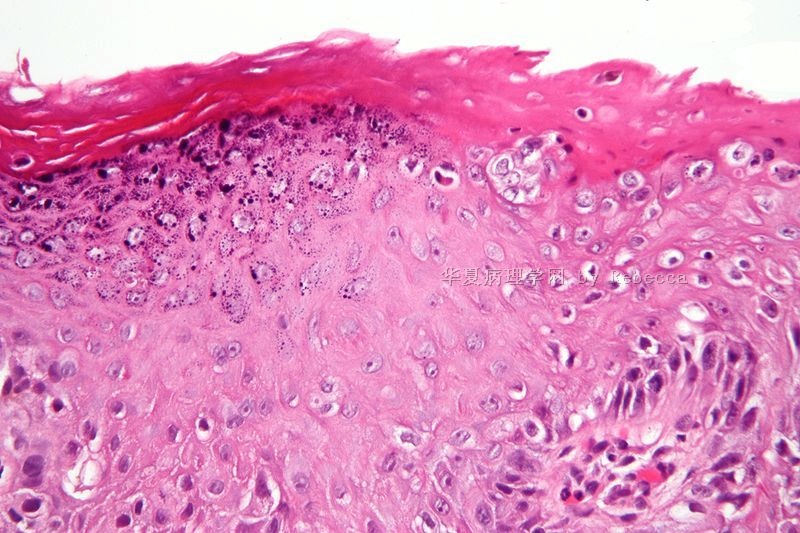
病理组织学主要表现为:鳞状上皮内高度瘤变、病理核分裂像活跃,角化过度、角化不良(上皮内细胞角化珠出现,又称鲍温氏细胞)、角化不全,真皮乳头增生增宽形成围裙样改变。
外阴上皮内瘤变(VIN)是外阴阴道疾病研究国际学会(ISSVD)于1989年拟定的外阴疾病系统分类其中一术语。它代替了过去外阴萎缩、鲍温氏病及kraurosis vulvae一系列这些传统术语。
VIN根据病理组织形态学又分为:
VIN I 轻度
VIN II 中度
VIN III 重度及包括外阴原位癌
我们在临床上不大见到VINI的情况,究其原因可能是VINI处于一种轻度病变状态,缺乏临床症状与表现,它容易被忽略,对应宫颈CINI来说。走笔到此深为细胞学之父——巴氏所创造发明的Pap Test仰止。
2004年,ISSVD对VIN进行了重新归类。以前用来描述上皮内轻度瘤变的VIN 1将不再使用,因这类变化被认为是由于刺激因或非癌前疣状病毒感染所致。目前VIN一词指的是高级别鳞状上皮内的不正常病变(即已知的VIN2、VIN3)。
鲍温氏病乃鳞状上皮内的原位癌(CIS)。VIN III涵盖了外阴原位癌。因而它们可以视为等同术语。所以该例诊断Bowen's Disease也是可以的。
ISSVD分类术语是比较经典,它能反应及体现外阴阴道疾病谱系。VIN一术语也能从病理组织学上阐述并对应临床。所以我们应接受它,无论文献查询及撰写论文都是必要的。
VIN治疗原则上是手术切除局部病灶,激光治疗,5-氟尿嘧啶软膏等。
该例将在活检创面愈合后,局部用5-氟尿嘧啶软膏治疗、随访。有可能将在3-6个月后进行第二次
手术切除残留的病灶;如是,我们将再次回到这里来继续。
D.D
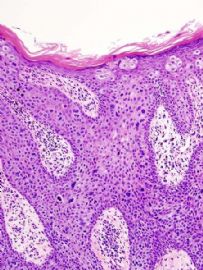
外阴的乳腺外Paget‘s病
它是非常罕见。病理基础表现在正常鳞状上皮内有迁徒移行来的孤立的腺癌导管上皮,有认为可能是来自巴氏腺。

- 三十功名尘与土,八千里路云与月。
-
(Squamous) vulval (or vulvar) intraepithelial neoplasia (VIN) is a pre-cancerous skin lesion of the vulva, and was previously known as Bowen's disease of the vulva.
The presence of abnormal cells may occur anywhere on the vulvar skin. VIN is not invasive cancer but may eventually become invasive squamous cell cancer if left untreated.
In 2004, the International Society for the Study of Vulvovaginal Diseases (ISSVD) has reclassified VIN. The term VIN 1, previously used to describe a mild change in the lower epithelial lining, will no longer be used - these changes have been found to be due to irritation or non-precancerous viral wart infection. The term VIN now refers to high grade abnormal squamous lesions only (these were previously known as VIN 2 and VIN 3).
VIN (usual type) can be described by the pathologist as warty, basaloid or mixed. These types of VIN are due to infection with cancer-forming (oncogenic) types of human papillomavirus.
A less common ‘differentiated’ type of VIN is not caused by human papillomavirus and is associated with rapidly growing squamous cell carcinoma.
VIN, unclassified type, is rare and is of unknown origin.
很抱歉,没有太多的时间来翻译它们。不是很难懂的,让我们大家一起来学习或复习吧。


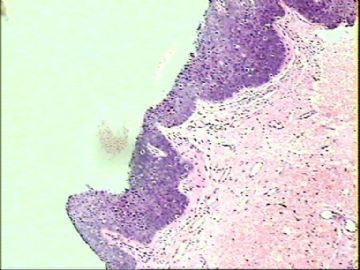
名称:图1
描述:图1

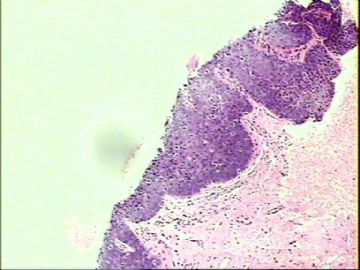
名称:图2
描述:图2

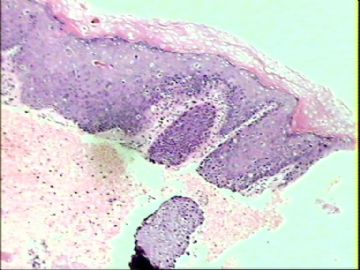
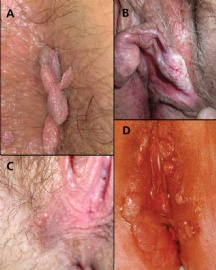
名称:图3
描述:图3

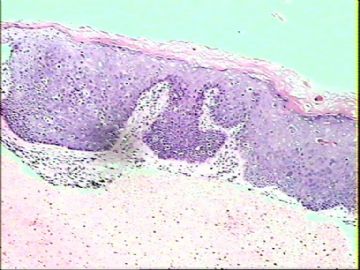
名称:图4
描述:图4

- 三十功名尘与土,八千里路云与月。
Rewiew for Vulvar Intraepithelial Neoplasia VIN
The term Vulvar intraepithelial neoplasia (VIN) refers to particular changes that can occur in the skin that covers the vulva. VIN is not cancer, and in some women it disappears without treatment. If the changes become more severe, there is a chance that cancer might develop after many years, and so it is referred to as a precancerous condition.
ISSVD Classification
Medically speaking, the term denotes a squamous intraepithelial lesion of the vulva that shows dysplasia with varying degrees of atypia. The epithelial basement membrane is intact and the lesion is thus not invasive but has invasive potential.
The terminology of VIN evolved over several decades. In 1989[2] the Committee on Terminology, International Society for the Study of Vulvar Disease (ISSVD) replaced older terminology such as vulvar dystrophy, Bowen's disease, and Kraurosis vulvae by a new classification system for Epithelial Vulvar Disease:
Nonneoplastic epithelial disorders of vulva and mucosa:
Lichen sclerosus
Squamous hyperplasia
Other dermatoses
Mixed neoplastic and nonneoplastic disorders
Intraepithelial neoplasia
Squamous vulvar intraepithelial neoplasia (VIN)
VIN I, mildest form
VIN II, intermediate
VIN III, most severe form including carcinoma in situ of the vulva
Non-squamous intraepithelial neoplasia
Extramammary Paget's disease
Tumors of melanocytes, non invasive
Invasive disease (vulvar carcinoma)
Diagnosis
The patient may have no symptoms, or local symptomatology including itching, burning, and pain. The diagnosis is always based on a careful inspection and a targeted biopsy.
Treatment
The treatment of VIN is local to wide excision, in case of very extensive involvement or recurrency even a simple vulvectomy. Laser therapy has also been useful for VIN.
Additional images:
Micrograph of vulvar intraepithelial neoplasia III or Grade 3 (VIN 3). H&E stain.
名称:图1
描述:图1
名称:图2
描述:图2
名称:图3
描述:图3

- 三十功名尘与土,八千里路云与月。
-
本帖最后由 于 2010-09-28 21:30:00 编辑
| 以下是引用wfbjwt在2010-9-14 18:22:00的发言: 鲍温病、派杰病、浅表恶黑鉴别。 |

 wfbjwt
wfbjwt
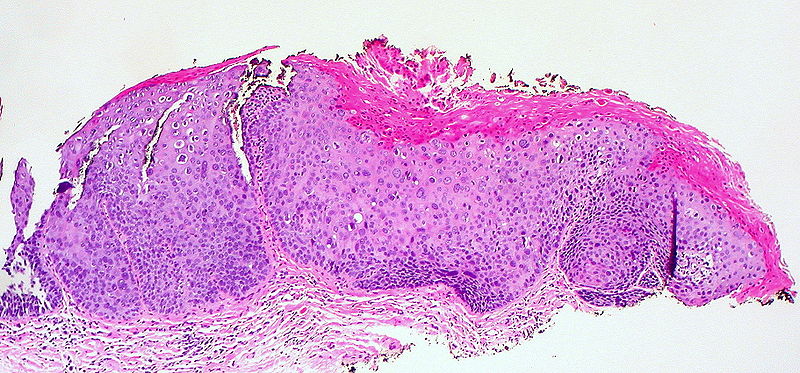
Review for Bowen's Disease
Bowen's disease (BD) (also known as "squamous cell carcinoma in situ"[1]:655) is a neoplastic skin disease, it can be considered as an early stage or intraepidermal form of squamous cell carcinoma. It was named after Dr John T. Bowen, the doctor who first described it in 1912. Erythroplasia of Queyrat is a form of squamous cell carcinoma in situ arising on the glans or prepuce, possibly induced by HPV.[2]
Causes
Causes of BD include solar damage, arsenic, immunosuppression (including AIDS), viral infection (human papillomavirus or HPV) and chronic skin injury and dermatoses.
Signs and symptoms
Bowen's disease typically presents as a gradually enlarging, well demarcated erythematous plaque with an irregular border and surface crusting or scaling. BD may occur at any age in adults but is rare before the age of 30 years - most patients are aged over 60. Any site may be affected, although involvement of palms or soles is uncommon. BD occurs predominantly in women (70-85% of cases). About 60-85% of patients have lesions on the lower leg, usually in previously or presently sun exposed areas of skin.
This is a persistent progressive non-elevated red scaly or crusted plaque which is due to an intraepidermal carcinoma and is potentially malignant. The lesions may occur anywhere on the skin surface or on mucosal surfaces. Freezing, cauterization or diathermy coagulation is often effective treatment.
Histology
Bowen's disease is essentially equivalent to squamous cell carcinoma in situ. Atypical squamous cells proliferate through the whole thickness of the epidermis. The entire tumor is confined to the epidermis and does not invade into the dermis. The cells in Bowen's are often highly atypical under the microscope, and may in fact look more unusual than the cells of some invasive squamous cell carcinomas.
Additional images
onmouseover="showMenu(this.id, 0, 1)">

- 三十功名尘与土,八千里路云与月。
-
本帖最后由 于 2010-09-14 20:00:00 编辑
| 以下是引用wy1992在2010-9-13 23:43:00的发言: PAGED'S disease |
谢谢wy1992老师提供的思路。 

Review for Extramammary Paget's Disease
Extramammary Paget’s disease (EMPD), also Extramammary Paget disease, is a rare, slow-growing, usually non-invasive intraepithelial (in the skin) adenocarcinoma outside of the mammary gland and includes Paget's disease of the vulva and the extremely rare Paget's disease of the penis.
Extramammary Paget’s disease involves primarily the epidermis but occasionally extends into the underlying dermis.It has a predilection for apocrine gland bearing areas, mostly the perineum, vulva, axilla, scrotum, and penis.
Prognosis and comorbity
Extramammary Paget's disease is usually seen in isolation and is not usually associated with an underlying invasive malignancy. This is unlike Paget's disease of the breast, which is almost always associated with an underlying invasive malignancy, i.e. breast cancer (e.g. mammary ductal carcinoma).
Signs and symptoms
Signs and symptoms are a skin lesion often mistaken as eczema that may be itchy or painful. A biopsy will establish the diagnosis. The histology of the lesion is the same as for Paget's disease of the breast.
Types
Paget's disease of the vulva, a rare disease, may be a primary lesion or associated with adenocarcinoma originating from local organs such as the Bartholin gland, the urethra, or the rectum and thus be secondary. Patients tend to be postmenopausal.
Paget's disease of the penis may also be primary or secondary and is even rarer than genital Paget’s disease in women. At least one case has been misdiagnosed as Bowen's disease.Isolated Paget's disease of the penis is extremely rare.
Primary disease
It is important to exclude that the lesion is associated with another cancer. Primary disease is usually treated by surgical excision.
History
James Paget described Paget's disease of the nipple in 1874. Radcliffe Crocker reported the first case of EMPD in 1889 when he described a patient with a skin lesion affecting the penis and scrotum, the findings of which were identical to those described by Paget.
Micrograph of extramammary Paget's disease. H&E stain.
名称:图1
描述:图1

- 三十功名尘与土,八千里路云与月。