| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- ‘外阴白斑’活检1例(VINIII第二次手术标本病理会诊报告 2010-09-29)
-
本帖最后由 于 2010-09-30 12:04:00 编辑
归纳与小结(P100282 )
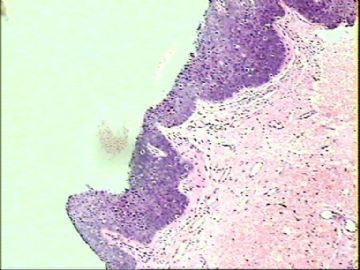
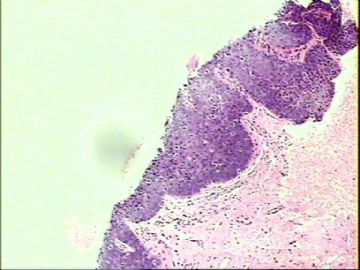
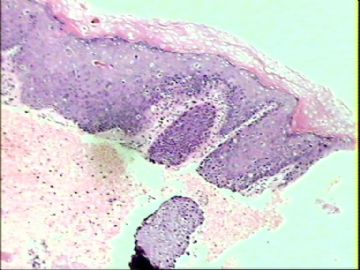
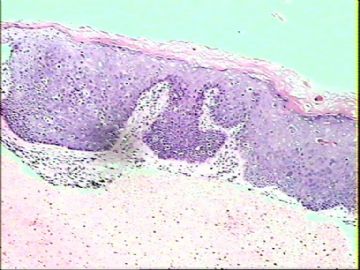
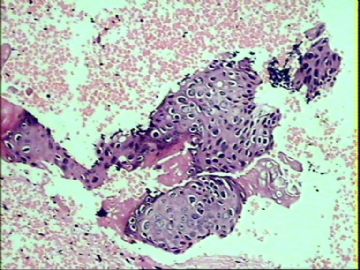
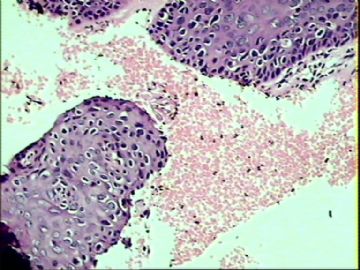
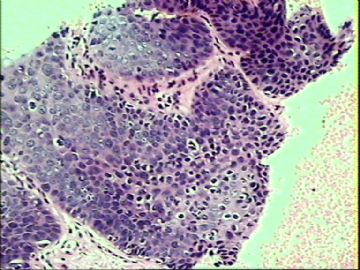
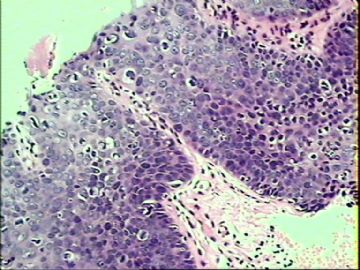
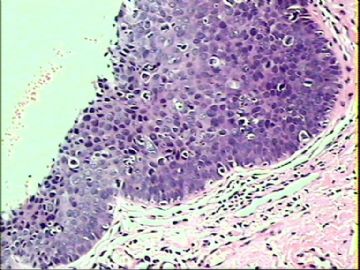
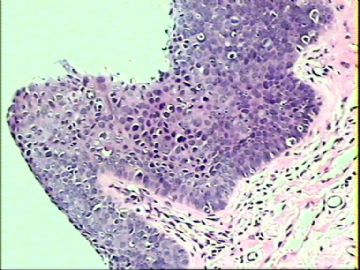
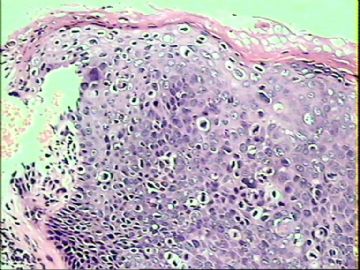
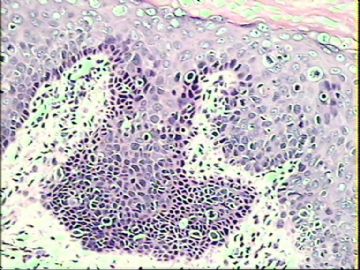
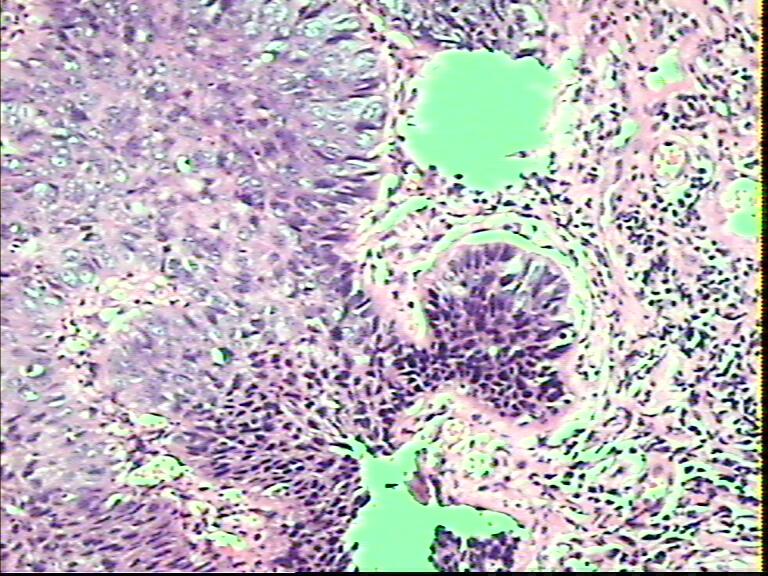
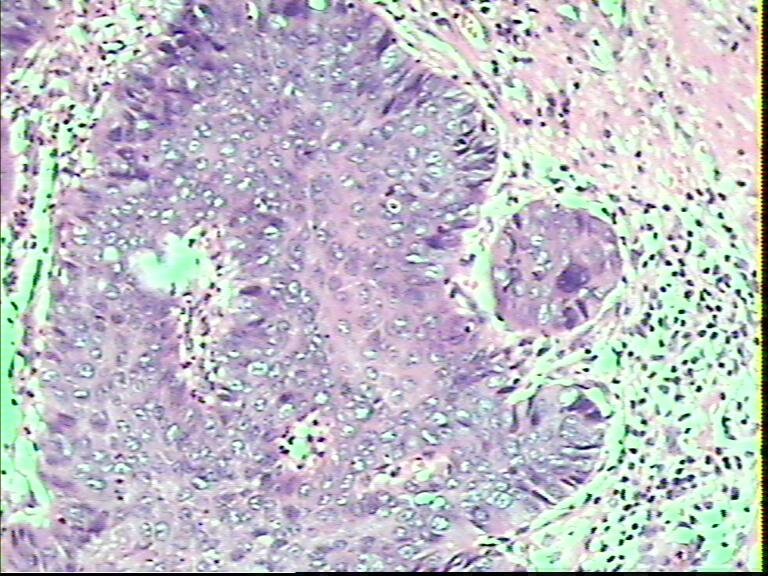
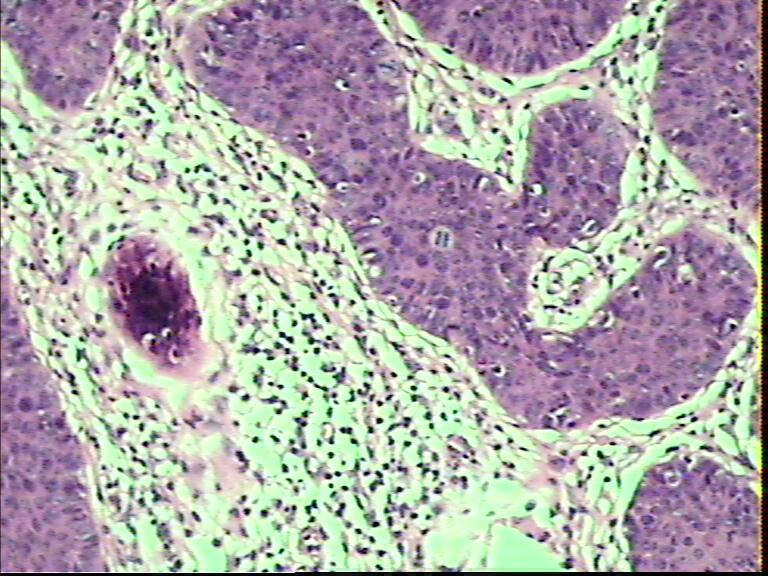
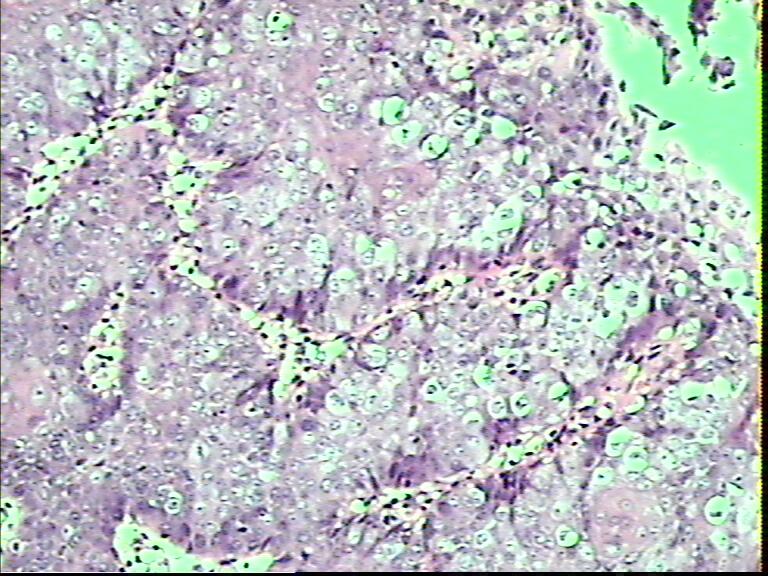
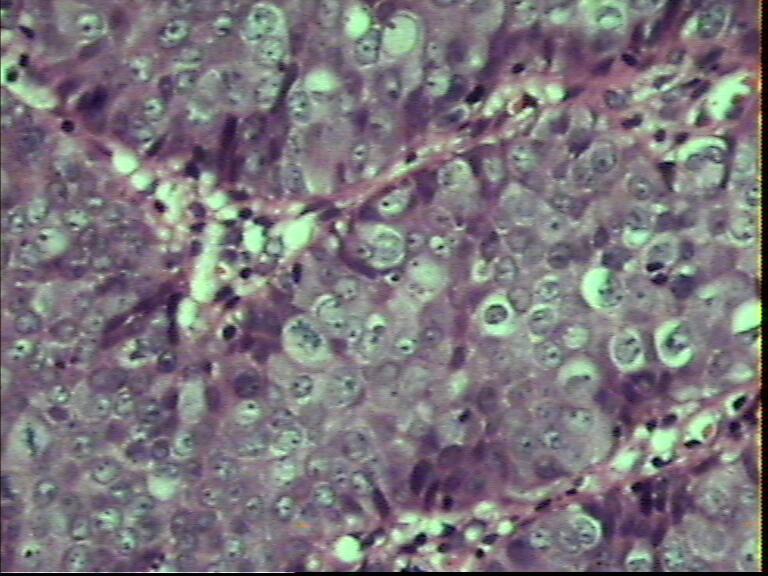
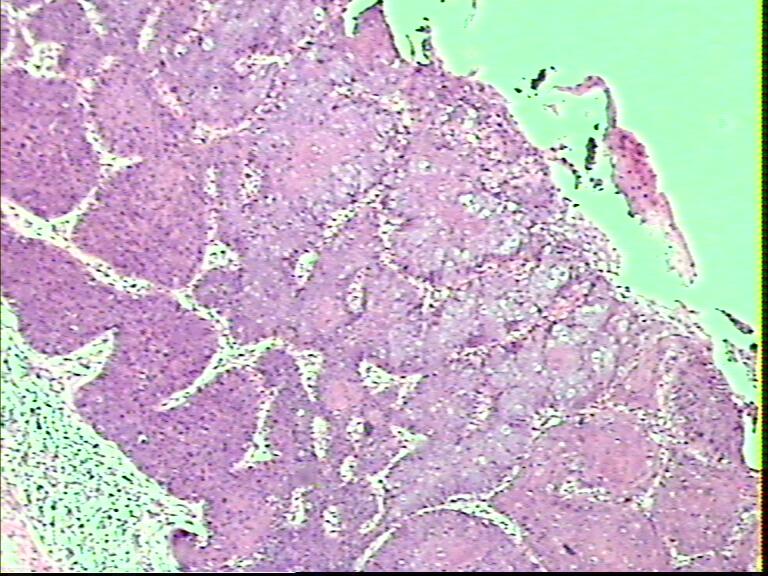
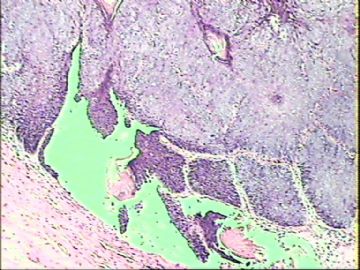
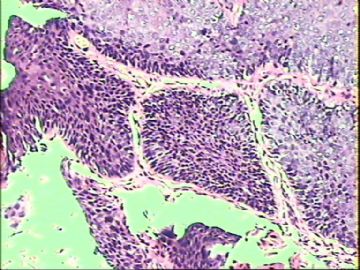
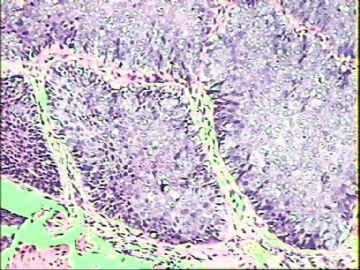
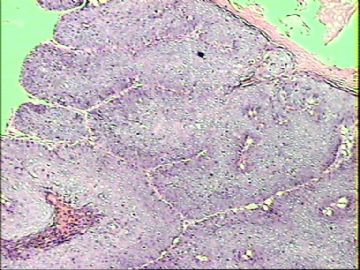
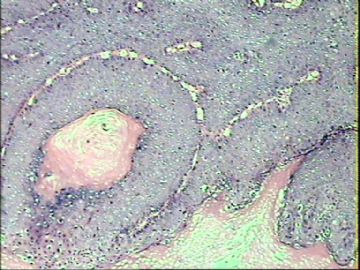
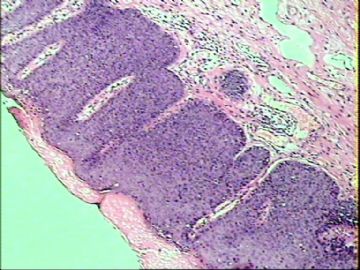
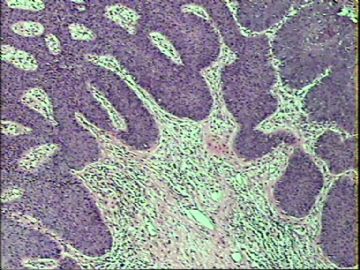
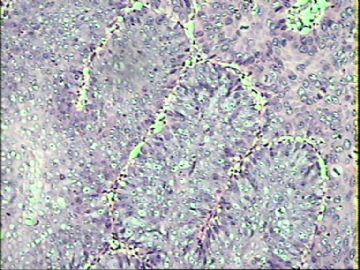
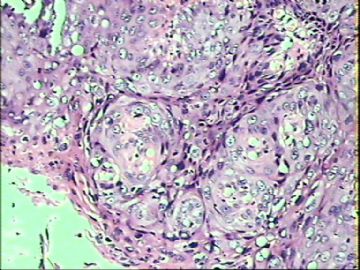
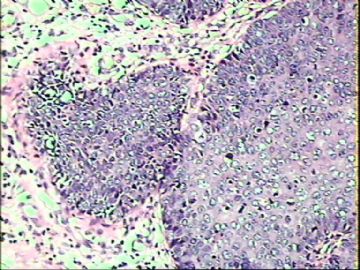
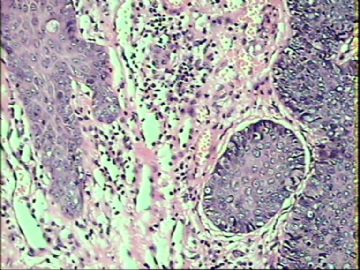
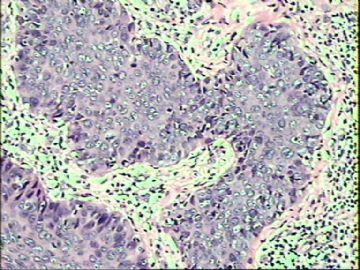
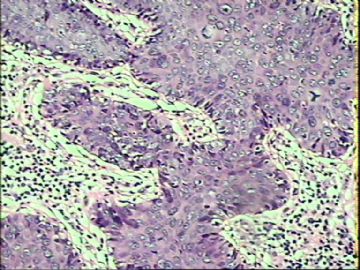
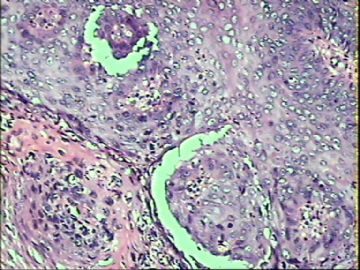
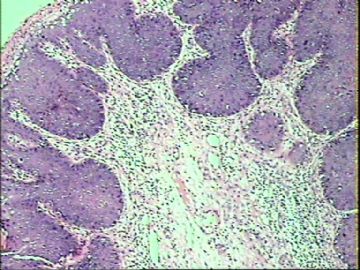
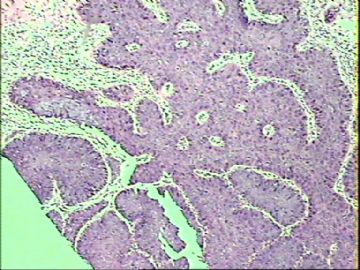
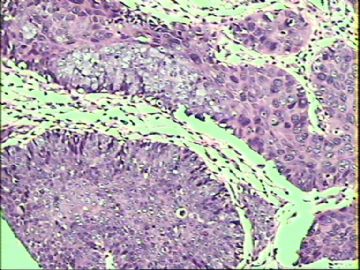
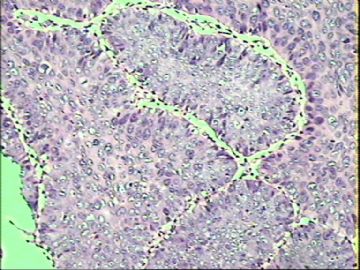
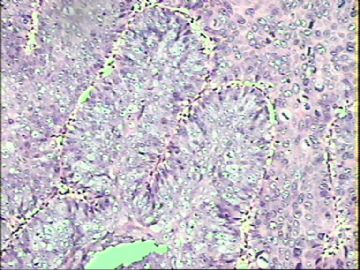
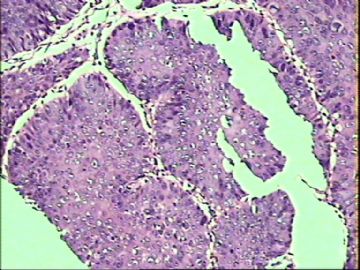
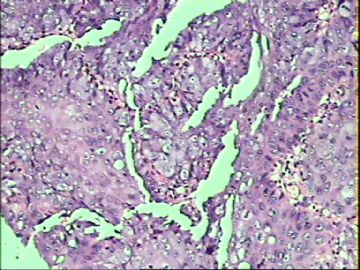
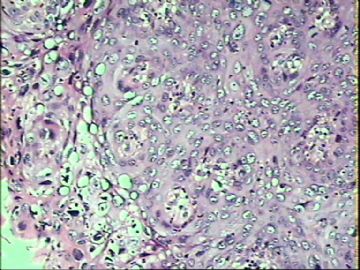
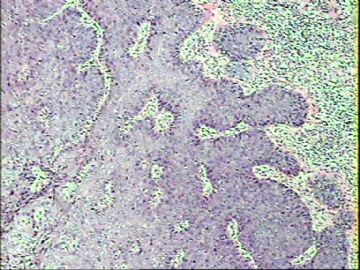
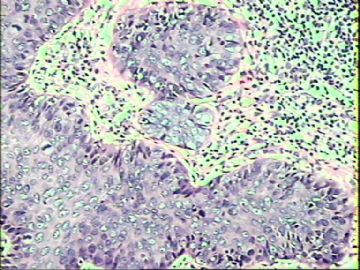
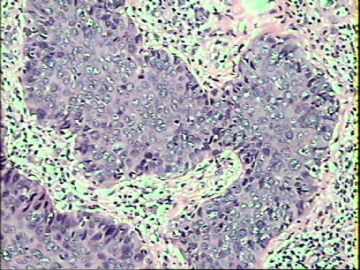
患者在9月17日病理活检诊断为VINIII(P100269),随后行白色病灶处全部切除送病检。镜下表现为CIS特征。癌变上皮呈乳头状增生,同时也有上皮乳头向下增生像棘皮瘤样排布,增生的上皮乳头横切。之间有纤细的间质分隔开来。细胞核分裂活跃,病理核分裂多见。细胞异型性明显,挖空细胞多见。
该例难点主要是判断有无浸润或早期浅表性浸润?事实上鉴别后者有时往往是比较困难的,正如czhao老师所指出:It is difficult to evalute the superficial invasion even though the true glass slides are reviwed.
所以, 无论如何要看到间质内癌细胞(巢)的浸润,这是很关键的。我们看到的这些增生上皮乳头团横切面,周边的基底膜还是存在的,光滑的,完整的;尽管细胞学异型性很明显,部分视野细胞分化也比较差。但基底层细胞极像还是存在的,增生上皮团之间有同相、延续的关系。
诊断浸润性外阴癌要持重,因治疗方案完全不同。
在一些特殊或有疑问牵涉到后继术式、决定治疗原则问题的病例上,最好是申请本地上级(中心)医院病理诊断中心或本地病理学会主任委员托管所在医院,请多几位有经验的资深同道在多头显微镜下一起会诊读片,面对面的讨论切磋是很有必要的,这也是分摊或化解医疗责任风险、尽量避免执业失误的重要举措之一。在工作中掌握一个原则:那就是在自己的想法与上级医院、上级医师有偏差或意见相左时,原则上是以上级医院、上级医生签名负责制为准。
尽量稳打稳扎,步步为营。要学会悟出什么地方可能容易出问题,该怎么优化解决它们为好。

该例难点主要是判断有无浸润或早期浅表性浸润?事实上鉴别后者有时往往是比较困难的,正如czhao老师所指出:It is difficult to evalute the superficial invasion even though the true glass slides are reviwed.
所以, 无论如何要看到间质内癌细胞(巢)的浸润,这是很关键的。我们看到的这些增生上皮乳头团横切面,周边的基底膜还是存在的,光滑的,完整的;尽管细胞学异型性很明显,部分视野细胞分化也比较差。但基底层细胞极像还是存在的,增生上皮团之间有同相、延续的关系。
诊断浸润性外阴癌要持重,因治疗方案完全不同。
在一些特殊或有疑问牵涉到后继术式、决定治疗原则问题的病例上,最好是申请本地上级(中心)医院病理诊断中心或本地病理学会主任委员托管所在医院,请多几位有经验的资深同道在多头显微镜下一起会诊读片,面对面的讨论切磋是很有必要的,这也是分摊或化解医疗责任风险、尽量避免执业失误的重要举措之一。在工作中掌握一个原则:那就是在自己的想法与上级医院、上级医师有偏差或意见相左时,原则上是以上级医院、上级医生签名负责制为准。
尽量稳打稳扎,步步为营。要学会悟出什么地方可能容易出问题,该怎么优化解决它们为好。



- 三十功名尘与土,八千里路云与月。
| 以下是引用cqzhao在2010-9-29 1:52:00的发言:
|

 谢谢赵老师经典话语。
谢谢赵老师经典话语。

- 三十功名尘与土,八千里路云与月。
Review for Vulvar Cancer
Vulvar cancer, a malignant invasive growth in the vulva, accounts for about 4 % of all gynecological cancers and typically affects women in later life. It is estimated that in the United States in 2006 about 3,740 new cases will be diagnosed and about 880 women will die as a result of vulvar cancer.[1] Vulvar carcinoma is separated from vulvar intraepithelial neoplasia (VIN), a non-invasive lesion of the epithelium that can progress via carcinoma-in-situ to squamous cell cancer, and from Paget disease of the vulva.
Types
Squamous cell carcinoma
The vast majority of vulvar cancer (approximately 90%)[2] is caused by squamous cell carcinoma, which originates from the epidermis of the vulva tissue. Carcinoma-in-situ is a precursor stage of squamous cell cancer prior to invading through the basement membrane. Most lesions originate in the labia, primarily the labia majora. Other areas affected are the clitoris, and fourchette, and the local glands. While the lesion is more common with advancing age, younger women who have risk factors (v.i.) may also be affected. In the elderly treatment may be complicated by the interference of other medical conditions.
Squamous lesions tend to be unifocal, growing with local extension, and spreading via the local lymph system. The lymphatic drainage of the labia proceeds to the upper vulva and mons, then to the inguinal and femoral nodes with both superficial and deep lymph nodes. The last deep femoral node is called the Cloquet’s node; spread beyond this node affects the lymph nodes of the pelvis. The tumor may also invade adjacent organs such as the vagina, urethra, and rectum and spread via their lymphatics.
A verrucous carcinoma of the vulva is a subtype of the squamous cell cancer and tend to appear as a slowly growing wart.
Melanoma
About 5% of vulvar malignancy is caused by melanoma of the vulva. Such melanoma behaves like melanoma in other locations and may affect a much younger population. Contrary to squamous carcinoma, melanoma has a high risk of metastasis.
Basal cell carcinoma
Basal cell carcinoma affects about 1-2% of vulvar cancer is a slowly growing lesion and affects the elderly. Its behavior is similar to basal cell carcinoma in other locations that is it tends to grow locally with a low potential of deep invasion or metastasis.
Other lesions
Vulvar cancer can be caused by other lesions such as adenocarcinoma or sarcoma.
Types
Squamous cell carcinoma
The vast majority of vulvar cancer (approximately 90%)[2] is caused by squamous cell carcinoma, which originates from the epidermis of the vulva tissue. Carcinoma-in-situ is a precursor stage of squamous cell cancer prior to invading through the basement membrane. Most lesions originate in the labia, primarily the labia majora. Other areas affected are the clitoris, and fourchette, and the local glands. While the lesion is more common with advancing age, younger women who have risk factors (v.i.) may also be affected. In the elderly treatment may be complicated by the interference of other medical conditions.
Squamous lesions tend to be unifocal, growing with local extension, and spreading via the local lymph system. The lymphatic drainage of the labia proceeds to the upper vulva and mons, then to the inguinal and femoral nodes with both superficial and deep lymph nodes. The last deep femoral node is called the Cloquet’s node; spread beyond this node affects the lymph nodes of the pelvis. The tumor may also invade adjacent organs such as the vagina, urethra, and rectum and spread via their lymphatics.
A verrucous carcinoma of the vulva is a subtype of the squamous cell cancer and tend to appear as a slowly growing wart.
Melanoma
About 5% of vulvar malignancy is caused by melanoma of the vulva. Such melanoma behaves like melanoma in other locations and may affect a much younger population. Contrary to squamous carcinoma, melanoma has a high risk of metastasis.
Basal cell carcinoma
Basal cell carcinoma affects about 1-2% of vulvar cancer is a slowly growing lesion and affects the elderly. Its behavior is similar to basal cell carcinoma in other locations that is it tends to grow locally with a low potential of deep invasion or metastasis.
Other lesions
Vulvar cancer can be caused by other lesions such as adenocarcinoma or sarcoma.

- 三十功名尘与土,八千里路云与月。
-
本帖最后由 于 2010-09-23 12:02:00 编辑
| 以下是引用一棵小草在2010-9-20 22:59:00的发言: 是外阴粘膜白斑发展而来的原位癌? |
现在已不主张用外阴白斑(leukoplakia of vulva)这一术语,代之为外阴营养不良(vulvar dystrophies)或外阴白色病变(white lesions of the vulva)
.它可能是一组原因不明的非感染性炎性疾病或多种原因引起的局部营养代谢障碍疾病。根据病程可分类为1、非特异性外阴炎;2、萎缩性硬化性苔藓;3、神经性皮炎;4、白色角化病。
它们均可继发表皮的非典型性增生,甚至癌变。
VIN3这一类多为高危性HPV(H16、H18等)感染所致。我们在本例上述的组织图像中也可以看到有明显的HPV感染导致的上皮内细胞的改变。



- 三十功名尘与土,八千里路云与月。
| 以下是引用mingfuyu在2010-9-23 8:30:00的发言:
Agree with VIN 2-3. You can do mucin stain to exclude extramammary Paget's disease, and do melanoma markers to exclude melanoma in-situ. VIN is a little different from CIN: VIN occurs in skin, could be caused by HPV infection and non-HPV infection (for example p53 mutation), CIN is caused by HPV. Especially in older women, there is a type of high grade VIN (differentiated VIN) is not caused by HPV. |
Great!!


- 三十功名尘与土,八千里路云与月。