本帖最后由 于 2010-07-31 12:46:00 编辑
看到Dr.XLJin的详尽诊断思路和鉴别要点后,早上很幸运查到了Dr.Rodney T. Miller的一个较新的对所谓未分化肿瘤的详实讲解和记录,和大家分享。
里面提到很多较新而全面的形态学和免疫组化内容,真的是宝贝。对本例诊断思路和后续工作可能会有帮助。在Google里是一定可以查打这篇原文的,是免费的。
对于本例:在临床未提供相应转移瘤可能的前提下,可能还是要考虑胸腺上皮起源的恶性肿瘤,期待楼主的后续报道。
Immunohistochemical Approach
to “Undifferentiated” Tumors
Rodney T. Miller, M.D.
Director of Immunohistochemistry
ProPath Laboratory
1355 River Bend Drive
Dallas, TX 75247-4915
rodney.miller@propath.com
www.propath.com
American Academy of Oral and Maxillofacial Pathology
Annual Meeting – Tucson, AZ
Sunday, May 16, 2010
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 1
INTRODUCTION
As we all know, immunohistochemistry (IHC) is an extremely valuable adjunct to
standard morphologic diagnosis in diagnostic pathology. It has rapidly become the
standard of care, particularly when dealing with a number of common diagnostic
problems, including "undifferentiated malignant tumor", metastatic carcinoma of
unknown origin, lymphoma classification, and similar problems. In this portion of the
presentation, I will discuss an approach to the diagnosis of malignant tumors that appear
"undifferentiated" by light microscopy. I should say at this point that the approach
discussed includes my personal biases, and other pathologists may advocate a different
approach or employ different antibodies (Abs) in certain types of cases. However, the
approach I will discuss has served me well in the past, and I look forward to improving
these approaches as new and more specific markers become available. We also need to
keep in mind that there are exceptions to everything, and not all tumors will necessarily
react as they are "supposed" to (since "tumors don't read textbooks"). This underscores
the importance of a thorough background in standard morphologic diagnosis employing
the time-honored and venerable H&E section.
The topics that I will be covering today are very broad, so I will not be able to cover
everything in the degree of detail that I would like. However, I have tried to make the
handout materials as useful as possible, by condensing much of the information into lists
and tables. I have found these types of lists to be very helpful in jogging my memory, and
I hope the lists find themselves within easy reach of your microscope as you deal with
difficult cases.
IMPORTANCE OF A PANEL APPROACH TO DIAGNOSTIC PROBLEMS
The importance of a panel approach to diagnostic problems cannot be
overemphasized. Many of the most egregious errors that can occur will happen because
the pathologist has not ordered enough stains in his or her diagnostic battery to
appropriately address the differential diagnostic possibilities in a particular case. We use
IHC because the cases are by nature difficult, and skimping on stains may save the patient
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 2
a bit of money, but may also provide the patient with an incorrect or otherwise
suboptimal diagnosis.
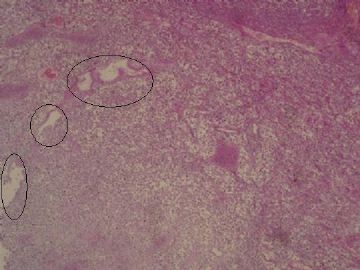
The Concept of “Undifferentiated Tumors
"Undifferentiated" typically refers to tumor that is composed of a proliferation of
“primitive cells” that do not show any recognizable line of cellular differentiation. It is
well known however, that most tumors that appear "undifferentiated" by light microscopy
do express evidence of a specific line of cellular differentiation when studied using other
techniques, commonly IHC. As such, in the particular context of our role as diagnostic
pathologists, the term "undifferentiated" is more accurately defined as "I don't know what
this tumor is based on the H&E appearance".
As diagnostic pathologists, our role is to precisely define the nature of the tumors that
we see, so that the clinicians who treat the patients can offer them the best and most
appropriate therapy. Most of the time that can be done on a standard H&E section, but
we are all too familiar with the fact that tumors of widely varying histogenesis can look
identical on an H&E stain. Fortunately, there are only a limited number of lines of
cellular differentiation that need to be considered, and if we are aware of the most useful
markers to screen for each of these pathways of cellular differentiation, a logical approach
to diagnosis can be formulated. The main lines cellular differentiation (histogenetic
categories) can be listed as follows:
1. Epithelial Tumors (carcinoma)
2. Germ cell – Sex Cord Stromal Tumors
3. Neuroendocrine Tumors
4. Melanocytic Tumors
5. Lymphohematopoetic Tumors (lymphoma, leukemia, histiocytic)
6. Mesenchymal Tumors (sarcoma)
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 3
When confronted by a tumor that appears undifferentiated by light microscopy, it can
be useful to try to place a tumor into a particular morphologic category of tumor, listed
below:
1. Pleomorphic Large Cell Tumors
2. Epithelioid Large Cell Tumors
3. Spindle Cell (Sarcomatoid) Tumors
4. Small Blue Cell Tumors (Round or Spindled)
In my day-to-day practice, I rely heavily on the use of sets of computerized notes to
assist my imperfect memory and to make certain that I do my best to consider all
reasonable possible diagnoses in my working differential diagnosis. These notes (which I
maintain in Excel spreadsheet format so that they are highly portable and readily
searchable), have enabled me to make a correct diagnosis in numerous difficult cases that
I otherwise would have missed. For those of you can, I encourage you to make use of
similar computerized notes and lists.
EPITHELIAL MARKERS
Cytokeratins: Cytokeratins (CK’s) are the most frequently used epithelial markers,
and I would estimate that 97% to 98% of carcinomas will stain with CK, provided an
appropriate CK Ab is employed.
What about “Pan-Cytokeratin”? Before discussing cytokeratins further, it is
worthwhile to discuss so called "pan-cytokeratin" or "pan-keratin" stains. To my
knowledge, there are no particular clones of antibodies that truly recognize all types of
cytokeratin, and for that reason, I have banished the term "pan-keratin" from my
consultation reports (and from my laboratory). Additionally, when I see the term "pankeratin"
on a pathology report, I do not really know what this means, particularly if the
clones used in this "pan-keratin" are not specified. Actually, I think the use of the term
"pan-keratin" can be misleading and sometimes dangerous, since some antibodies that are
frequently employed in this fashion (particularly AE1/AE3) are far from ideal "pankeratin"
reagents, and a number of pathologists who have employed "pan-keratin" stains
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 4
and have obtained negative results have erroneously concluded that the tumor they are
studying is not epithelial.
Cytokeratin AE1/AE3: This antibody cocktail if often referred to as a “pancytokeratin”,
but it is NOT a “pan-cytokeratin”, and anyone who uses this antibody in this
fashion is certainly doing some of their patients a disservice. The problem with
cytokeratin AE1/AE3 is that this cocktail does a poor job of detecting CK8, which is the
major CK in hepatocellular carcinoma (HCC) and many other carcinomas (ca’s),
particularly renal cell carcinoma (RCC), prostate carcinoma, and many other
adenocarcinomas. It is also not as good as high molecular weight CK antibody Ab (clone
34bE12) for recognizing squamous tumors. Below is a list of major problems that can
occur when CK AE1/AE3 is used as “pan-CK”:
1. The majority of HCC will be AE1/AE3 negative or very weak with AE1/AE3
2. A significant number of RCC and some prostate ca’s are negative with AE1/AE3
3. Some neuroendocrine ca’s are negative with AE1/AE3
4. A few squamous ca’s are negative with AE1/AE3
In my practice, the main utility of AE1/AE3 is in the diagnosis of HCC, since those
tumors are characteristically negative or weak with this antibody. I also use it in
situations where I want to highlight a population of cells that I know will stain positively
with it, but I NEVER USE AE1/AE3 AS A “PAN-CYTOKERATIN”!
I should say at this point that I do not have personal experience with some other socalled
“pan-CK” antibodies such as OSCAR, so I cannot address the strengths or
weaknesses of those reagents.
So-called “Pan-cytokeratin”: A better approach: In my experience, a far better
way to use CK’s to detect the greatest number of epithelial tumors is by doing 2 stains:
one stain that detects low molecular weight CK’s 8 and 18 (CK-LMW) (such as clones
CAM5.2, 5D3, Zym5.2), and a stain for high molecular weight CK (CK-HMW) using
clone 34bE12. This combination of CK-LMW and CK-HMW will enable you to
detect the broadest spectrum of epithelial tumors using CK Abs. Although these 2
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 5
reagents could be made into a cocktail, I prefer to see the results of the 2 stains separately,
as in many instances one can gain valuable information about the tumor based on the
relative intensity and pattern of staining with these 2 CK’s. Specifics of these 2 Abs
follow.
CK-LMW (CK’s 8 and 18): This CK Ab stains most adenocarcinomas, including
those that are often or may be negative with AE1/AE3, including HCC, RCC, prostate ca,
Hurthle cell ca of thyroid, and neuroendocrine ca’s. In the case of neuroendocrine ca’s,
perinuclear dots of CK-LMW may provide a clue that you are dealing with a
neuroendocrine tumor. Potential “traps” involve lack of staining of certain types of
epithelial tumors and staining of certain non-epithelial cells, as listed below:
1. CK-LMW may not stain translocation-associated RCC (TFE3+)
2. CK-LMW stains some non-epithelial cells and tumors, including the following:
- Interstitial reticulum cells in lymph nodes
- Submesothelial fibroblasts
- Epithelioid angiosarcoma (50-70%)
- Synovial sarcoma
- Epithelioid Sarcoma
- Alveolar rhabdomyosarcoma
- Some leiomyosarcomas, Ewing / PNET
- Few cases of gastrointestinal stromal tumors (GIST)
- Rare AML, myeloma, pheochromocytoma
CK-HMW, clone 34bE12 (CK’s 1, 5, 10, 14): This CK Ab has a number of useful
attributes:
1. Virtually all squamous ca’s show strong and diffuse reactivity with CK-HMW
2. If the CK-HMW stain is stronger than the CK-LMW stain, you are probably
dealing with a squamous tumor
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 6
3. CK-HMW is typically absent or weak and focal in HCC, RCC of conventional
type, and adrenocortical ca
4. Strong CK-HMW is uncommon in prostate ca
Phenotypic features of Squamous ca’s:
1. Strong diffuse expression of CK-HMW
2. Intensity of CK-HMW > CK-LMW
3. Strong diffuse co-expression of CK5 (or CK5/6) and nuclear p63
Traps: Cutaneous adnexal tumors show the above, and expression of CK5 is often
patchy in basaloid squamous ca’s
Limitations of Cytokeratins as a marker of epithelial tumors:
1. Expression of CK may be focal in poorly differentiated tumors (sampling issues)
2. A small percentage (<2%) of epithelial tumors are negative with CK’s (including
a high percentage of translocation-associated RCC’s, TFE3+)
3. Watch out for “bleeding artifacts”, which may make a non-epithelial tumors
appear to have CK
Epithelial Membrane Antigen (EMA): EMA is expressed in many epithelial
tumors, but is also expressed in many non-epithelial tumors, including certain lymphomas
and sarcomas. Therefore, in order for it to be used as a valid marker of epithelial
differentiation, mesenchymal and hematoplymphoid neoplasms must be excluded.
GERM CELL AND SEX-CORD STROMAL MARKERS
In the past several years, there have been great improvements in the markers available
for the recognition of germ cell tumors, relegating some of the previous markers (such as
placental alkaline phosphatase) obsolete. The most useful markers in my experience are
the following:
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 7
Germ Cell Tumor Markers:
SALL4: Nuclear marker of Yolk Sac Tumor, Embryonal ca, and Seminoma
OCT3/4: Nuclear marker of Embryonal ca and Seminoma
CD30 (Ki-1): Embryonal ca
D2-40 (podoplanin): Seminoma, in a diffuse strong membranous pattern
Glypican-3: Yolk Sac Tumor – stains many more cells than AFP
AFP: Stains a variable minority of cells in Yolk Sac Tumor
HLA-G: Excellent marker for the intermediate trophoblastic cells of choriocarcinoma
HCG: Syncytiotrophoblasts of choriocarcainoma and syncytiotrophoblastic giant cells
that may be present in other germ cell tumors
Other new markers (which I have not yet used):
NANOG: Nuclear marker of Embryonal ca and Seminoma, also some breast ca’s
SOX2: Embryonal ca, also gliomas, with 1 report of squamous ca’s of GI tract
GDF3: Strong in Seminoma, moderate to strong in Embryonal ca, weak or neg in Yolk
Sac
Traps: With SALL4 and OCT3/4, the reactivity should be diffuse and moderate to
strong in intensity. Some non-germ cell tumors show weak focal staining with these
markers. Additionally, I have seen a small number of high grade non-germ cell
carcinomas that have shown SALL4 expression similar to that seen in germ cell tumors.
However, germ cell tumor was excluded in these cases by other means. Obviously, it
must be kept in mind that CD30 stains some lymphomas, and I have also seen strong
staining of a few sarcomas with this marker, including dedifferentiated liposarcoma.
Glypican-3 also stains HCC, Wilms tumor, and occasionally some carcinomas. HLA-G
staining should be seen in >70% of the tumor cells in order to use it as a valid marker of
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 8
intermediate trophoblasts, as focal patchy staining may be seen in some non-trophoblastic
lesions. HCG is usually very strong in choriocarcinoma, and usually demonstrates
extensive bleeding artifact.
Sex-Cord Stromal Tumors:
Markers of Sex-Cord Stromal Tumors include Inhibin, Calretinin, and MART-1,
clone A103. In addition to staining sex-cord stromal tumors, the antibodies also stain the
following:
Inhibin: adrenocortical lesions, granular cell tumors, some neuroendocrine tumors,
and occasional carcinomas
Calretinin: adrenocortical lesions, mesothelioma, about 30-40% of squamous ca’s,
neural lesions, and occasionally other carcinomas
MART-1, clone A103: adrenocortical lesions and melanocytic lesions
NEUROENDOCRINE MARKERS
Chromogranin and Synaptophysin are an excellent screen for neuroendocrine
tumors. They should almost always be ordered together, as some neuroendocrine markers
will be positive for only 1 of these 2 markers. So-called “neuron-specific enolase” is not
neuron-specific, and is best avoided.
MELANOCYTIC MARKERS
S100 protein: Positive in 97-99% of melanomas, sensitive but not very specific
- also stains some carcinomas (especially breast ca), histiocytes (Langerhans cells),
sarcomas, myoepithelial and salivary gland tumors, neural tumors, sex-cord stromal
tumors, and rare lymphomas.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 9
Sox10: Nuclear marker, stains a higher percentage of melanomas and nevi than S100,
but does not stain breast carcinomas or histiocytes (useful for melanoma sentinel nodes).
- also stains neural lesions (schwannoma, neurofibroma, astrocytoma), granular cell
tumors, myoepithelial lesions (including salivary gland tumors). Cytoplasmic expression
may be seen in some T-cells, osteoclastic giant cells, and renal oncocytoma.
MART-1, HMB-45, and Tyrosinase: These markers have good specificity for
melanoma, and in my experience MART-1 is more sensitive than HMB-45. They also
stain perivascular epithelioid tumors (PEComas), and rare (<0.5%) of carcinomas may
show significant staining (including some cases of TFE3+ RCC). As mentioned above,
MART-1 clone A103 also stains adrenocortical tumors and sex-cord stromal tumors.
My current “melanoma screen” consists of immunostains for Sox10 and MART-1.
LYMPHOHEMATOPOETIC MARKERS
CD45 (Leukocyte Common Antigen, LCA): CD45 is highly sensitive and specific
for tumors of hematopoetic origin. A small minority of lymphohematopoetic tumors lack
CD45 (including Hodgkin lymphoma, CD30+ lymphomas, some T-cell lymphomas, and
some leukemias) so its absence does not rule out a hematolymphoid tumor. However, the
presence of CD45 virtually assures that you are dealing with a hematolymphoid process
of some type. CD45 shows a membranous pattern of immunoreactivity. I have also
observed that the antibody stains the luminal surface of proximal convoluted tubules in
the kidney, and also stains the cytoplasm of renal oncocytoma (even when using a
polymer detection complex, so the staining cannot be ascribed to endogenous biotin).
CD30 (Ki-1): CD30 is needed to recognize CD30-positive anaplastic large cell
lymphomas (which may be CD45 negative) and is also important in diagnosing Hodgkin's
disease. As mentioned above, CD30 can also be useful in subclassifying germ cell
tumors, since embryonal carcinomas are CD30 positive, whereas other types of germ cell
tumors are not. CD30 immunoreactivity can be both cytoplasmic and membranous. In
many cases a cytoplasmic "glob" of immunoreactivity is noted, corresponding to the
"golgi" area of the cell.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 10
B-cells markers: CD20, CD79a, and Pax5: These are all good markers of B-cells
tumors, although some important points to keep in mind are the following:
CD20 (L26) – Lost in patients who have received Rituximab therapy. Also negative
in some cases of B lymphoblastic leukemia / lymphoma. Staining limited to nucleoli is
nonspecific and should be ignored.
CD79a (mb1) – Also positive in acute promyelocytic leukemia (APL), plasma cells,
and some plasma cell myelomas.
Pax5 – stains nuclei of B-cells and Hodgkin cells, but also positive in some
neuroendocrine tumors (including Merkel cell tumor), mesonephric and mullerian
tumors, and alveolar rhabdomyosarcoma).
My current “screen” for B-cell lymphoma is CD20 and Pax5.
T-cell markers: CD2, CD3, CD5, CD7, TDT: It is a good idea to always employ >1
T-cell marker if T-cell lymphoma is a consideration, as T-cell lymphomas often
aberrantly lack one or more pan-T-cell markers. Some additional points to keep in mind
are as follows:
CD5 - coexpressed in some B-cells tumors (mantle cell lymphoma, CLL, and a small
percentage of diffuse large B-cell lymphoma).
CD7 - expressed in some myeloid leukemias. Ignore any artifactual nucleolar staining.
TDT - expressed in T-lymphoblastic leukemia / lymphoma, also in some myeloid
leukemias. It is also expressed in normal thymic T cells, and these cells typically show a
high Ki-67 proliferative fraction. Therefore, TDT(+) T cells with a high proliferative
fraction do not necessarily mean you are dealing with a neoplasm, since these findings
could be explained by sampling normal thymic T-cells. If you have a piece of tissue, you
can usually pick up cytokeratin-positive cells in the background, which can be a tip-off
that you are looking at thymic tissue.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 11
Natural killer (NK cell marker: CD56. Natural killer cell neoplasms show variable
expression of T-cell markers. CD56 is also expressed in some plasma cell myelomas,
leukemias, neuroendocrine tumors, certain sarcomas, and some carcinomas.
Myeloid Leukemia Markers: Myeloperoxidase, lysozyme, CD68, CD13, and CD33
are good markers of myeloid differentiation. There is some evidence that CD68 clone
PG-M1 has specificity for monocytic differentiation.
Histiocytic / Dendritic cell markers: Lysozyme and CD68 are good markers of
histiocytic origin. Follicular dendritic cell tumors express CD21 and Clusterin, and
Langerhans cell neoplasms express S100 protein and CD1a.
CD43: One could make an argument for including CD43 in a screening lymphoma
panel, since it stains tumors that may lack other lymphohematopoetic screening markers.
The only non-lymphohematopoetic tumor that I am aware of that expresses CD43 is
adenoid cystic carcinoma. Occasionally one will encounter a tumor where CD43 is the
only marker that stains the neoplastic cells, a situation that I refer to as the "CD43-only
syndrome”. The differential diagnosis of this condition is as follows:
CD43-only Syndrome:
1. Anaplastic large cell lymphoma
2. Leukemias (AML, AMML, erythroleukemia)
3. NK-cell tumors, including plasmacytoid dendritic
cell tumor, CD4+ hematodermic tumor
4. Plasma cell neoplasms
5. Langerhans cell histiocytosis
Traps with lymphohematopoetic markers:
1. Ordering too few markers. If the tumor is poorly differentiated or if you have little
tissue, it is wise to use >1 marker for each lineage (e.g., CD20 and Pax5 for B-cells, CD3
and CD5 for T cells, CD43 for leukemias and NK cells).
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 12
2. Pax5 expression in neuroendocrine tumors, Hodgkin lymphoma, and alveolar
rhabdomyosarcoma
3. CD79a in acute promyelocytic leukemia (APL) and myelomas
3. TDT in thymoma and in Merkel cell tumor
4. Focal CK expression in rare lymphohematopoetic tumors
MESENCHYMAL MARKERS
Rhabdomyosarcoma: Desmin is sensitive, Myogenin (nuclear) specific, although
regenerating skeletal muscle fibers may also express Myogenin. Pax5 can be expressed
in alveolar rhabdomyosarcoma.
Leiomyosarcoma: Smooth muscle myosin and Caldesmon are specific. Smooth
muscle actin is sensitive but also stains myofibroblastic lesions. Muscle specific actin
(MSA) is a bit more specific than SMA. All of these markers also will label
myoepithelial cells.
Angiosarcoma: CD31 and CD34 offer a reasonably good screen for vascular
neoplasms. Factor VIII has good specificity (although this marker also stains
megakaryocytes and megakaryocytic tumors). D2-40 (podoplanin) is a good marker of
lymphatic differentiation, but also stains a number of other tumors including seminoma
and mesothelioma. FLI-1 can be an endothelial marker but I have not been particularly
impressed with its performance in my laboratory. LMO2 is a relatively recently-described
endothelial marker.
Synovial sarcoma: TLE-1 often shows strong diffuse nuclear staining, and these
tumors also typically express focal cytokeratin and/or EMA. They are also CD56+ and
often CD99+. A substantial minority expresses S100. FISH for SYT translocation is
very helpful in rendering a definitive diagnosis of this tumor.
Alveolar soft part sarcoma: Strong nuclear staining with TFE3 is characteristic of
this tumor.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 13
Gastrointestinal Stromal Tumors (GIST): DOG1 is a sensitive and specific marker
for these tumors. CD117 (c-kit) stains most GIST, and many stain with CD34. They lack
Sox10, S100, and usually lack muscle markers.
Liposarcoma: Ki-67 clone K2 can be helpful in recognizing lipoblasts, as it stains
membranes of viable fat cells. MDM2 and CDK4 have been found to be useful in the
recognition of well differentiated liposarcoma and in dedifferentiated liposarcoma.
Epithelioid sarcoma: The tumors express cytokeratins and EMA, and often CD34.
Lack of nuclear staining with INI1 (BAF47) can be extremely helpful.
Malignant peripheral nerve sheath tumor (MPNST): Sox10 and S100 protein are
expressed in a subpopulation of tumors, and some also lack nuclear staining with INI1
(BAF47). Some authors state that the tumors are negative for microphthalmia
transcription factor (MiTF), which can be useful in their differential diagnosis with
melanoma, which expresses MITF (as noted above however, MiTF is not specific for
melanoma). These tumors are typically CD56+ and CD99-.
Traps with mesenchymal lesions:
1. Expression of cytokeratins and/or EMA by sarcomas
2. Spindle cell carcinoma can express SMA or MSA, and some can show occasional
desmin positive cells.
3. Misinterpretation of background cell reactivity as tumor cell reactivity
- CK reactivity in submesothelial fibroblasts
- Desmin reactivity by mesothelial cells.
- Expression of S100 by histiocytes
- Myogenin reactivity in regenerating skeletal muscle cells
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 14
IMMUNOHISTOCHEMICAL APPROACH TO
UNDIFFERENTIATED MALIGNANT TUMOR.
Initial considerations:
1. Value of looking at H&E first without looking at patient history first.
2. Clinical information can guide your differential diagnosis (age, history, location, etc.)
If prior pertinent pathology exists – try to look at that first.
3. How much tissue do we have to work with, and are clinicians in a big rush?
- If lots of tissue and no rush – sequential rounds of stains OK
- If minimal tissue or big rush – better to “blast away” up front
(cost of more stains is usually < cost of re-biopsy)
4. If minimal tissue – order stains in “order of importance”, and have 10 or more extra
sections cut and held, in case more stains are needed (rather than having to re-face the
paraffin block another time)
5. Use lists to help jog your memory
Useful Initial Panel (if you don’t have a clue what the tumor is):
CK-LMW Sox10 CD45 (LCA) CD43 SYN
CK-HMW MART-1 CD30 (Ki-1) SALL4 CHG
SUMMARY AND CONCLUSIONS
1. Appearances can be deceiving.
2. Importance of good clinical information and review of previous pathology.
3. Importance of panel approach – often need >1 marker per diagnostic category.
4. Be mindful of what you have to work with, and alter your approach accordingly.
5. Use lists so that you won’t forget things as easily.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 15
It must be kept in mind that there are exceptions to everything, and not all
tumors will necessarily react as I have indicated. This underscores the importance
of a carefully performed H&E examination by a skilled anatomic pathologist in
arriving at the correct diagnosis. If the immunostain findings don't make sense when
viewing the H&E, then the immunostain findings should be considered suspect
(especially if the immunostains were performed using so-called "Predilute Ready-To-
Use" antibodies).
Selected References
1. Stevenson AJ, Chatten J, Bertoni F et al: CD99 (p30/32MIC2)
neuroectodermal/Ewing's sarcoma antigen as an immunohistochemical marker.
Review of more than 600 tumors and the literature experience. Applied
Immunohistochemistry 2(4): 231-240, 1994.
2. Renshaw AA: O13 (CD99) in spindle cell tumors. Reactivity with
hemangiopericytoma, solitary fibrous tumor, synovial sarcoma, and meningioma, but
rarely with sarcomatoid mesothelioma. Applied Immunohistochemistry 3(4): 250-
256, 1995.
3. CD34: A review. van de Rijn M, Rouse RV: Applied Immunohistochemistry 2(2):
71-80, 1994.
4. Lumade JA, Askin FB, Perlman EJ: MIC2 analysis of small cell carcinoma.
American Journal of Clinical Pathology 102: 692-694, 1994.
5. Weiss LM, Arber DA, Chang KL: CD68: A review. Applied
Immunohistochemistry 2(1): 2-8, 1994.
6. DeYoung BR, Wick MR, Fitzgibbon JF et al: CD31: An immunospecific marker for
endothelial differentiation in human neoplasms. Applied Immunohistochemistry 1:
97-100, 1993.
7. Lloyd RV, Cano M, Rosa P et al: Distribution of chromogranin A and secretogranin I
(chromogranin B) in neuroendocrine cells and tumors. American Journal of
Pathology 130(2): 296-304, 1988.
8. Miettinen M: Synaptophysin and neurofilament proteins as markers for
neuroendocrine tumors. Archives of Pathology and Laboratory Medicine 111: 813-
818, 1987.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 16
9. Arber DA, Kandalaft PL, Mehta P et al: Vimentin-negative epithelioid sarcoma. The
value of an immunohistochemical panel that includes CD34. The American Journal
of Surgical Pathology 17(3): 302-307, 1993.
10. Shah IA, Netto D, Schlageter MO et al: Neurofilament immunoreactivity in Merkel
cell tumors: A differentiating feature from small cell carcinoma. Modern Pathology
6(1): 3-9, 1993.
11. 11: Dorfman DM, Pinkus GS: CD99 (p30/32MIC2) immunoreactivity in the
diagnosis of thymic neoplasms and mediastinal lymphoproliferative disorders. A
study of paraffin sections using monoclonal antibody O13. Applied
Immunohistochemistry 4(1): 34-42, 1996.
12. Pinkus GS, Kurtin PJ: Epithelial membrane antigen - A diagnostic discriminant in
surgical pathology. Immunohistochemical profile in epithelial, mesenchymal, and
hematopoetic neoplasms using paraffin sections and monoclonal antibodies. Human
Pathology 16: 929-940, 1985.
13. Sloane JP, Ormerod MG: Distribution of epithelial membrane antigen in normal and
neoplastic tissues and its value in diagnostic tumor pathology. Cancer 47: 1786-
1795, 1981.
14. Lloyd RV, Jin L, Zhang S: Proconvertases 2 and 3 are specific neuroendocrine
markers. Modern Pathology 9(1):173A (abstract #1016), 1996.
15. Folpe AL, Patterson K, Gown A: Antibodies to desmin identify the blastemal
component of nephroblastoma. . Modern Pathology 10(9):895-900, 1997.
16. Nonaka D, Chiriboga L, Rubin BP: Sox10: A Pan-Schwannian and Melanocytic
Marker. The American Journal of Surgical Pathology 32(9): 1291-1298, Sep 2008.
17. Cao D, Guo S, Allan RW et al: SALL4 is a novel sensitive and specific marker of
ovarian primitive germ cell tumors and is particularly useful in establishing yoke sac
tumor from clear cell carcinoma. The American Journal of Surgical Pathology
33(6): 894-904, Jun 2009 .
18. Cao D, Li J, Guo S et al: SALL4 is a novel diagnostic marker for testicular germ cell
tumors. The American Journal of Surgical Pathology 33(7): 1065-1077, Jul 2009 .
19. Liegl B, Hornick JL, Corless CL et al: Monoclonal antibody to DOG1.1 shows higher
sensitivity than KIT in the diagnosis of gastrointestinal stromal tumors, including
unusual subtypes. The American Journal of Surgical Pathology 33(3): 437-446,
Mar 2009.
20. Singer G, Kurman RJ, McMaster MT et al: HLA-G immunoreactivity is specific for
intermediate trophoblast in gestational trophoblastic disease and cancer of as a useful
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 17
marker in differential diagnosis. The American Journal of Surgical Pathology
26(7): 914-920, Jul 2002.
21. Hornick JL, Cin PD, Fletcher CDM: Loss of INI 1 expression is characteristic of both
conventional and proximal-type epithelioid sarcoma. The American Journal of
Surgical Pathology 33(4): 542-550, Apr 2009.
22. Binh MBN, Sastre-Garau X, de Pinieux G et al: MDM2 and CDK4 immunostainings
are useful adjuncts in diagnosing well-differentiated and dedifferentiated liposarcoma
subtypes. A comparative analysis of 559 soft tissue neoplasms with genetic data. The
American Journal of Surgical Pathology 29(10): 1340-1347, Oct 2005.
23. Terry J, Saito T, Subramanian S et al: TLE1 as a diagnostic immunohistochemical
marker for synovial sarcomas emerging from gene expression profile and studies. The
American Journal of Surgical Pathology 31(2): 240-246, Feb 2007.
24. Buresh CJ, Oliai BR, Miller RT: Reactivity with TDT in a Merkel cell carcinoma. A
potential diagnostic pitfall. The American Journal of Clinical Pathology 129 (6):
894-898. Jun 2008
25. Feldman AL, Dogan A: Diagnostic uses of Pax5 immunohistochemistry. Advances
in Anatomic Pathology 14(5):323-334, Sep 2007.
26. Zynger DL, Dimov ND, Luan C et al: Glypican-3: A novel marker in testicular germ
cell tumors. The American Journal of Surgical Pathology 30(12): 1570-1575, Dec
2006.
27. Santagat S, Ligon K, Hornick JL: Embryonic standard cell transcription factor
signatures in the diagnosis of primary and metastatic germ cell tumors (OCT3/4,
NANOG, and SOX2). The American Journal of Surgical Pathology 31(6): 836-845,
Jun 2007.
J Clin Pathol 2007;60:936-938 doi:10.1136/jcp.2006.044750
Leucocyte common antigen (CD45) and CD5 positivity in an “undifferentiated” carcinoma: a potential diagnostic pitfall
- Nyethane Ngo1,
- Kaushik Patel2,
- Peter G Isaacson3,
- Kikkeri N Naresh4
+ Author Affiliations
-
1Department of Histopathology, Hammersmith Hospital, Imperial College, London, UK
-
2Department of Histopathology, Kingston Hospital, London, UK
-
3Department of Histopathology, University College, London, UK
-
4Department of Histopathology, Hammersmith Hospital, Imperial College, London, UK
- Correspondence to:
 Professor K N Naresh
 Department of Histopathology, Hammersmith Hospital, Du Cane Road, London W12 0HS, UK; k.naresh@imperial.ac.uk
CD45 is a transmembrane protein tyrosine phosphatase located on most haematopoietic cells. It has several isoforms, and haematopoietic cells express one or more of the isoforms—CD45RO, CD45RA and CD45RB.1,2 CD45 immunoreactivity is recognised to be highly specific for non–Hodgkin’s lymphomas.3,4 CD45-expressing non-haemopoietic tumours are very rare. This was first noted by McDonnell et al5 in 1987, who reported a primitive sarcoma expressing CD45. Subsequently, Nandedkar et al6 reported three cases of undifferentiated large-cell, possibly neuroendocrine, carcinomas expressing CD45. Two of them were lymph node metastasis and one was a pulmonary tumour. All the three cases expressed both CD45 and cytokeratin. Two of the cases behaved in an aggressive manner.6
In contrast to CD45, CD5 is expressed in thymic carcinoma and malignant mesothelioma.7,8 To the best of our knowledge, this is the first reported case of a carcinoma expressing both CD45 and CD5.
看到Dr.XLJin的详尽诊断思路和鉴别要点后,早上很幸运查到了Dr.Rodney T. Miller的一个较新的对所谓未分化肿瘤的详实讲解和记录,和大家分享。
里面提到很多较新而全面的形态学和免疫组化内容,真的是宝贝。对本例诊断思路和后续工作可能会有帮助。在Google里是一定可以查打这篇原文的,是免费的。
对于本例:在临床未提供相应转移瘤可能的前提下,可能还是要考虑胸腺上皮起源的恶性肿瘤,期待楼主的后续报道。
Immunohistochemical Approach
to “Undifferentiated” Tumors
Rodney T. Miller, M.D.
Director of Immunohistochemistry
ProPath Laboratory
1355 River Bend Drive
Dallas, TX 75247-4915
rodney.miller@propath.com
www.propath.com
American Academy of Oral and Maxillofacial Pathology
Annual Meeting – Tucson, AZ
Sunday, May 16, 2010
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 1
INTRODUCTION
As we all know, immunohistochemistry (IHC) is an extremely valuable adjunct to
standard morphologic diagnosis in diagnostic pathology. It has rapidly become the
standard of care, particularly when dealing with a number of common diagnostic
problems, including "undifferentiated malignant tumor", metastatic carcinoma of
unknown origin, lymphoma classification, and similar problems. In this portion of the
presentation, I will discuss an approach to the diagnosis of malignant tumors that appear
"undifferentiated" by light microscopy. I should say at this point that the approach
discussed includes my personal biases, and other pathologists may advocate a different
approach or employ different antibodies (Abs) in certain types of cases. However, the
approach I will discuss has served me well in the past, and I look forward to improving
these approaches as new and more specific markers become available. We also need to
keep in mind that there are exceptions to everything, and not all tumors will necessarily
react as they are "supposed" to (since "tumors don't read textbooks"). This underscores
the importance of a thorough background in standard morphologic diagnosis employing
the time-honored and venerable H&E section.
The topics that I will be covering today are very broad, so I will not be able to cover
everything in the degree of detail that I would like. However, I have tried to make the
handout materials as useful as possible, by condensing much of the information into lists
and tables. I have found these types of lists to be very helpful in jogging my memory, and
I hope the lists find themselves within easy reach of your microscope as you deal with
difficult cases.
IMPORTANCE OF A PANEL APPROACH TO DIAGNOSTIC PROBLEMS
The importance of a panel approach to diagnostic problems cannot be
overemphasized. Many of the most egregious errors that can occur will happen because
the pathologist has not ordered enough stains in his or her diagnostic battery to
appropriately address the differential diagnostic possibilities in a particular case. We use
IHC because the cases are by nature difficult, and skimping on stains may save the patient
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 2
a bit of money, but may also provide the patient with an incorrect or otherwise
suboptimal diagnosis.
The Concept of “Undifferentiated Tumors
"Undifferentiated" typically refers to tumor that is composed of a proliferation of
“primitive cells” that do not show any recognizable line of cellular differentiation. It is
well known however, that most tumors that appear "undifferentiated" by light microscopy
do express evidence of a specific line of cellular differentiation when studied using other
techniques, commonly IHC. As such, in the particular context of our role as diagnostic
pathologists, the term "undifferentiated" is more accurately defined as "I don't know what
this tumor is based on the H&E appearance".
As diagnostic pathologists, our role is to precisely define the nature of the tumors that
we see, so that the clinicians who treat the patients can offer them the best and most
appropriate therapy. Most of the time that can be done on a standard H&E section, but
we are all too familiar with the fact that tumors of widely varying histogenesis can look
identical on an H&E stain. Fortunately, there are only a limited number of lines of
cellular differentiation that need to be considered, and if we are aware of the most useful
markers to screen for each of these pathways of cellular differentiation, a logical approach
to diagnosis can be formulated. The main lines cellular differentiation (histogenetic
categories) can be listed as follows:
1. Epithelial Tumors (carcinoma)
2. Germ cell – Sex Cord Stromal Tumors
3. Neuroendocrine Tumors
4. Melanocytic Tumors
5. Lymphohematopoetic Tumors (lymphoma, leukemia, histiocytic)
6. Mesenchymal Tumors (sarcoma)
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 3
When confronted by a tumor that appears undifferentiated by light microscopy, it can
be useful to try to place a tumor into a particular morphologic category of tumor, listed
below:
1. Pleomorphic Large Cell Tumors
2. Epithelioid Large Cell Tumors
3. Spindle Cell (Sarcomatoid) Tumors
4. Small Blue Cell Tumors (Round or Spindled)
In my day-to-day practice, I rely heavily on the use of sets of computerized notes to
assist my imperfect memory and to make certain that I do my best to consider all
reasonable possible diagnoses in my working differential diagnosis. These notes (which I
maintain in Excel spreadsheet format so that they are highly portable and readily
searchable), have enabled me to make a correct diagnosis in numerous difficult cases that
I otherwise would have missed. For those of you can, I encourage you to make use of
similar computerized notes and lists.
EPITHELIAL MARKERS
Cytokeratins: Cytokeratins (CK’s) are the most frequently used epithelial markers,
and I would estimate that 97% to 98% of carcinomas will stain with CK, provided an
appropriate CK Ab is employed.
What about “Pan-Cytokeratin”? Before discussing cytokeratins further, it is
worthwhile to discuss so called "pan-cytokeratin" or "pan-keratin" stains. To my
knowledge, there are no particular clones of antibodies that truly recognize all types of
cytokeratin, and for that reason, I have banished the term "pan-keratin" from my
consultation reports (and from my laboratory). Additionally, when I see the term "pankeratin"
on a pathology report, I do not really know what this means, particularly if the
clones used in this "pan-keratin" are not specified. Actually, I think the use of the term
"pan-keratin" can be misleading and sometimes dangerous, since some antibodies that are
frequently employed in this fashion (particularly AE1/AE3) are far from ideal "pankeratin"
reagents, and a number of pathologists who have employed "pan-keratin" stains
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 4
and have obtained negative results have erroneously concluded that the tumor they are
studying is not epithelial.
Cytokeratin AE1/AE3: This antibody cocktail if often referred to as a “pancytokeratin”,
but it is NOT a “pan-cytokeratin”, and anyone who uses this antibody in this
fashion is certainly doing some of their patients a disservice. The problem with
cytokeratin AE1/AE3 is that this cocktail does a poor job of detecting CK8, which is the
major CK in hepatocellular carcinoma (HCC) and many other carcinomas (ca’s),
particularly renal cell carcinoma (RCC), prostate carcinoma, and many other
adenocarcinomas. It is also not as good as high molecular weight CK antibody Ab (clone
34bE12) for recognizing squamous tumors. Below is a list of major problems that can
occur when CK AE1/AE3 is used as “pan-CK”:
1. The majority of HCC will be AE1/AE3 negative or very weak with AE1/AE3
2. A significant number of RCC and some prostate ca’s are negative with AE1/AE3
3. Some neuroendocrine ca’s are negative with AE1/AE3
4. A few squamous ca’s are negative with AE1/AE3
In my practice, the main utility of AE1/AE3 is in the diagnosis of HCC, since those
tumors are characteristically negative or weak with this antibody. I also use it in
situations where I want to highlight a population of cells that I know will stain positively
with it, but I NEVER USE AE1/AE3 AS A “PAN-CYTOKERATIN”!
I should say at this point that I do not have personal experience with some other socalled
“pan-CK” antibodies such as OSCAR, so I cannot address the strengths or
weaknesses of those reagents.
So-called “Pan-cytokeratin”: A better approach: In my experience, a far better
way to use CK’s to detect the greatest number of epithelial tumors is by doing 2 stains:
one stain that detects low molecular weight CK’s 8 and 18 (CK-LMW) (such as clones
CAM5.2, 5D3, Zym5.2), and a stain for high molecular weight CK (CK-HMW) using
clone 34bE12. This combination of CK-LMW and CK-HMW will enable you to
detect the broadest spectrum of epithelial tumors using CK Abs. Although these 2
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 5
reagents could be made into a cocktail, I prefer to see the results of the 2 stains separately,
as in many instances one can gain valuable information about the tumor based on the
relative intensity and pattern of staining with these 2 CK’s. Specifics of these 2 Abs
follow.
CK-LMW (CK’s 8 and 18): This CK Ab stains most adenocarcinomas, including
those that are often or may be negative with AE1/AE3, including HCC, RCC, prostate ca,
Hurthle cell ca of thyroid, and neuroendocrine ca’s. In the case of neuroendocrine ca’s,
perinuclear dots of CK-LMW may provide a clue that you are dealing with a
neuroendocrine tumor. Potential “traps” involve lack of staining of certain types of
epithelial tumors and staining of certain non-epithelial cells, as listed below:
1. CK-LMW may not stain translocation-associated RCC (TFE3+)
2. CK-LMW stains some non-epithelial cells and tumors, including the following:
- Interstitial reticulum cells in lymph nodes
- Submesothelial fibroblasts
- Epithelioid angiosarcoma (50-70%)
- Synovial sarcoma
- Epithelioid Sarcoma
- Alveolar rhabdomyosarcoma
- Some leiomyosarcomas, Ewing / PNET
- Few cases of gastrointestinal stromal tumors (GIST)
- Rare AML, myeloma, pheochromocytoma
CK-HMW, clone 34bE12 (CK’s 1, 5, 10, 14): This CK Ab has a number of useful
attributes:
1. Virtually all squamous ca’s show strong and diffuse reactivity with CK-HMW
2. If the CK-HMW stain is stronger than the CK-LMW stain, you are probably
dealing with a squamous tumor
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 6
3. CK-HMW is typically absent or weak and focal in HCC, RCC of conventional
type, and adrenocortical ca
4. Strong CK-HMW is uncommon in prostate ca
Phenotypic features of Squamous ca’s:
1. Strong diffuse expression of CK-HMW
2. Intensity of CK-HMW > CK-LMW
3. Strong diffuse co-expression of CK5 (or CK5/6) and nuclear p63
Traps: Cutaneous adnexal tumors show the above, and expression of CK5 is often
patchy in basaloid squamous ca’s
Limitations of Cytokeratins as a marker of epithelial tumors:
1. Expression of CK may be focal in poorly differentiated tumors (sampling issues)
2. A small percentage (<2%) of epithelial tumors are negative with CK’s (including
a high percentage of translocation-associated RCC’s, TFE3+)
3. Watch out for “bleeding artifacts”, which may make a non-epithelial tumors
appear to have CK
Epithelial Membrane Antigen (EMA): EMA is expressed in many epithelial
tumors, but is also expressed in many non-epithelial tumors, including certain lymphomas
and sarcomas. Therefore, in order for it to be used as a valid marker of epithelial
differentiation, mesenchymal and hematoplymphoid neoplasms must be excluded.
GERM CELL AND SEX-CORD STROMAL MARKERS
In the past several years, there have been great improvements in the markers available
for the recognition of germ cell tumors, relegating some of the previous markers (such as
placental alkaline phosphatase) obsolete. The most useful markers in my experience are
the following:
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 7
Germ Cell Tumor Markers:
SALL4: Nuclear marker of Yolk Sac Tumor, Embryonal ca, and Seminoma
OCT3/4: Nuclear marker of Embryonal ca and Seminoma
CD30 (Ki-1): Embryonal ca
D2-40 (podoplanin): Seminoma, in a diffuse strong membranous pattern
Glypican-3: Yolk Sac Tumor – stains many more cells than AFP
AFP: Stains a variable minority of cells in Yolk Sac Tumor
HLA-G: Excellent marker for the intermediate trophoblastic cells of choriocarcinoma
HCG: Syncytiotrophoblasts of choriocarcainoma and syncytiotrophoblastic giant cells
that may be present in other germ cell tumors
Other new markers (which I have not yet used):
NANOG: Nuclear marker of Embryonal ca and Seminoma, also some breast ca’s
SOX2: Embryonal ca, also gliomas, with 1 report of squamous ca’s of GI tract
GDF3: Strong in Seminoma, moderate to strong in Embryonal ca, weak or neg in Yolk
Sac
Traps: With SALL4 and OCT3/4, the reactivity should be diffuse and moderate to
strong in intensity. Some non-germ cell tumors show weak focal staining with these
markers. Additionally, I have seen a small number of high grade non-germ cell
carcinomas that have shown SALL4 expression similar to that seen in germ cell tumors.
However, germ cell tumor was excluded in these cases by other means. Obviously, it
must be kept in mind that CD30 stains some lymphomas, and I have also seen strong
staining of a few sarcomas with this marker, including dedifferentiated liposarcoma.
Glypican-3 also stains HCC, Wilms tumor, and occasionally some carcinomas. HLA-G
staining should be seen in >70% of the tumor cells in order to use it as a valid marker of
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 8
intermediate trophoblasts, as focal patchy staining may be seen in some non-trophoblastic
lesions. HCG is usually very strong in choriocarcinoma, and usually demonstrates
extensive bleeding artifact.
Sex-Cord Stromal Tumors:
Markers of Sex-Cord Stromal Tumors include Inhibin, Calretinin, and MART-1,
clone A103. In addition to staining sex-cord stromal tumors, the antibodies also stain the
following:
Inhibin: adrenocortical lesions, granular cell tumors, some neuroendocrine tumors,
and occasional carcinomas
Calretinin: adrenocortical lesions, mesothelioma, about 30-40% of squamous ca’s,
neural lesions, and occasionally other carcinomas
MART-1, clone A103: adrenocortical lesions and melanocytic lesions
NEUROENDOCRINE MARKERS
Chromogranin and Synaptophysin are an excellent screen for neuroendocrine
tumors. They should almost always be ordered together, as some neuroendocrine markers
will be positive for only 1 of these 2 markers. So-called “neuron-specific enolase” is not
neuron-specific, and is best avoided.
MELANOCYTIC MARKERS
S100 protein: Positive in 97-99% of melanomas, sensitive but not very specific
- also stains some carcinomas (especially breast ca), histiocytes (Langerhans cells),
sarcomas, myoepithelial and salivary gland tumors, neural tumors, sex-cord stromal
tumors, and rare lymphomas.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 9
Sox10: Nuclear marker, stains a higher percentage of melanomas and nevi than S100,
but does not stain breast carcinomas or histiocytes (useful for melanoma sentinel nodes).
- also stains neural lesions (schwannoma, neurofibroma, astrocytoma), granular cell
tumors, myoepithelial lesions (including salivary gland tumors). Cytoplasmic expression
may be seen in some T-cells, osteoclastic giant cells, and renal oncocytoma.
MART-1, HMB-45, and Tyrosinase: These markers have good specificity for
melanoma, and in my experience MART-1 is more sensitive than HMB-45. They also
stain perivascular epithelioid tumors (PEComas), and rare (<0.5%) of carcinomas may
show significant staining (including some cases of TFE3+ RCC). As mentioned above,
MART-1 clone A103 also stains adrenocortical tumors and sex-cord stromal tumors.
My current “melanoma screen” consists of immunostains for Sox10 and MART-1.
LYMPHOHEMATOPOETIC MARKERS
CD45 (Leukocyte Common Antigen, LCA): CD45 is highly sensitive and specific
for tumors of hematopoetic origin. A small minority of lymphohematopoetic tumors lack
CD45 (including Hodgkin lymphoma, CD30+ lymphomas, some T-cell lymphomas, and
some leukemias) so its absence does not rule out a hematolymphoid tumor. However, the
presence of CD45 virtually assures that you are dealing with a hematolymphoid process
of some type. CD45 shows a membranous pattern of immunoreactivity. I have also
observed that the antibody stains the luminal surface of proximal convoluted tubules in
the kidney, and also stains the cytoplasm of renal oncocytoma (even when using a
polymer detection complex, so the staining cannot be ascribed to endogenous biotin).
CD30 (Ki-1): CD30 is needed to recognize CD30-positive anaplastic large cell
lymphomas (which may be CD45 negative) and is also important in diagnosing Hodgkin's
disease. As mentioned above, CD30 can also be useful in subclassifying germ cell
tumors, since embryonal carcinomas are CD30 positive, whereas other types of germ cell
tumors are not. CD30 immunoreactivity can be both cytoplasmic and membranous. In
many cases a cytoplasmic "glob" of immunoreactivity is noted, corresponding to the
"golgi" area of the cell.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 10
B-cells markers: CD20, CD79a, and Pax5: These are all good markers of B-cells
tumors, although some important points to keep in mind are the following:
CD20 (L26) – Lost in patients who have received Rituximab therapy. Also negative
in some cases of B lymphoblastic leukemia / lymphoma. Staining limited to nucleoli is
nonspecific and should be ignored.
CD79a (mb1) – Also positive in acute promyelocytic leukemia (APL), plasma cells,
and some plasma cell myelomas.
Pax5 – stains nuclei of B-cells and Hodgkin cells, but also positive in some
neuroendocrine tumors (including Merkel cell tumor), mesonephric and mullerian
tumors, and alveolar rhabdomyosarcoma).
My current “screen” for B-cell lymphoma is CD20 and Pax5.
T-cell markers: CD2, CD3, CD5, CD7, TDT: It is a good idea to always employ >1
T-cell marker if T-cell lymphoma is a consideration, as T-cell lymphomas often
aberrantly lack one or more pan-T-cell markers. Some additional points to keep in mind
are as follows:
CD5 - coexpressed in some B-cells tumors (mantle cell lymphoma, CLL, and a small
percentage of diffuse large B-cell lymphoma).
CD7 - expressed in some myeloid leukemias. Ignore any artifactual nucleolar staining.
TDT - expressed in T-lymphoblastic leukemia / lymphoma, also in some myeloid
leukemias. It is also expressed in normal thymic T cells, and these cells typically show a
high Ki-67 proliferative fraction. Therefore, TDT(+) T cells with a high proliferative
fraction do not necessarily mean you are dealing with a neoplasm, since these findings
could be explained by sampling normal thymic T-cells. If you have a piece of tissue, you
can usually pick up cytokeratin-positive cells in the background, which can be a tip-off
that you are looking at thymic tissue.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 11
Natural killer (NK cell marker: CD56. Natural killer cell neoplasms show variable
expression of T-cell markers. CD56 is also expressed in some plasma cell myelomas,
leukemias, neuroendocrine tumors, certain sarcomas, and some carcinomas.
Myeloid Leukemia Markers: Myeloperoxidase, lysozyme, CD68, CD13, and CD33
are good markers of myeloid differentiation. There is some evidence that CD68 clone
PG-M1 has specificity for monocytic differentiation.
Histiocytic / Dendritic cell markers: Lysozyme and CD68 are good markers of
histiocytic origin. Follicular dendritic cell tumors express CD21 and Clusterin, and
Langerhans cell neoplasms express S100 protein and CD1a.
CD43: One could make an argument for including CD43 in a screening lymphoma
panel, since it stains tumors that may lack other lymphohematopoetic screening markers.
The only non-lymphohematopoetic tumor that I am aware of that expresses CD43 is
adenoid cystic carcinoma. Occasionally one will encounter a tumor where CD43 is the
only marker that stains the neoplastic cells, a situation that I refer to as the "CD43-only
syndrome”. The differential diagnosis of this condition is as follows:
CD43-only Syndrome:
1. Anaplastic large cell lymphoma
2. Leukemias (AML, AMML, erythroleukemia)
3. NK-cell tumors, including plasmacytoid dendritic
cell tumor, CD4+ hematodermic tumor
4. Plasma cell neoplasms
5. Langerhans cell histiocytosis
Traps with lymphohematopoetic markers:
1. Ordering too few markers. If the tumor is poorly differentiated or if you have little
tissue, it is wise to use >1 marker for each lineage (e.g., CD20 and Pax5 for B-cells, CD3
and CD5 for T cells, CD43 for leukemias and NK cells).
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 12
2. Pax5 expression in neuroendocrine tumors, Hodgkin lymphoma, and alveolar
rhabdomyosarcoma
3. CD79a in acute promyelocytic leukemia (APL) and myelomas
3. TDT in thymoma and in Merkel cell tumor
4. Focal CK expression in rare lymphohematopoetic tumors
MESENCHYMAL MARKERS
Rhabdomyosarcoma: Desmin is sensitive, Myogenin (nuclear) specific, although
regenerating skeletal muscle fibers may also express Myogenin. Pax5 can be expressed
in alveolar rhabdomyosarcoma.
Leiomyosarcoma: Smooth muscle myosin and Caldesmon are specific. Smooth
muscle actin is sensitive but also stains myofibroblastic lesions. Muscle specific actin
(MSA) is a bit more specific than SMA. All of these markers also will label
myoepithelial cells.
Angiosarcoma: CD31 and CD34 offer a reasonably good screen for vascular
neoplasms. Factor VIII has good specificity (although this marker also stains
megakaryocytes and megakaryocytic tumors). D2-40 (podoplanin) is a good marker of
lymphatic differentiation, but also stains a number of other tumors including seminoma
and mesothelioma. FLI-1 can be an endothelial marker but I have not been particularly
impressed with its performance in my laboratory. LMO2 is a relatively recently-described
endothelial marker.
Synovial sarcoma: TLE-1 often shows strong diffuse nuclear staining, and these
tumors also typically express focal cytokeratin and/or EMA. They are also CD56+ and
often CD99+. A substantial minority expresses S100. FISH for SYT translocation is
very helpful in rendering a definitive diagnosis of this tumor.
Alveolar soft part sarcoma: Strong nuclear staining with TFE3 is characteristic of
this tumor.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 13
Gastrointestinal Stromal Tumors (GIST): DOG1 is a sensitive and specific marker
for these tumors. CD117 (c-kit) stains most GIST, and many stain with CD34. They lack
Sox10, S100, and usually lack muscle markers.
Liposarcoma: Ki-67 clone K2 can be helpful in recognizing lipoblasts, as it stains
membranes of viable fat cells. MDM2 and CDK4 have been found to be useful in the
recognition of well differentiated liposarcoma and in dedifferentiated liposarcoma.
Epithelioid sarcoma: The tumors express cytokeratins and EMA, and often CD34.
Lack of nuclear staining with INI1 (BAF47) can be extremely helpful.
Malignant peripheral nerve sheath tumor (MPNST): Sox10 and S100 protein are
expressed in a subpopulation of tumors, and some also lack nuclear staining with INI1
(BAF47). Some authors state that the tumors are negative for microphthalmia
transcription factor (MiTF), which can be useful in their differential diagnosis with
melanoma, which expresses MITF (as noted above however, MiTF is not specific for
melanoma). These tumors are typically CD56+ and CD99-.
Traps with mesenchymal lesions:
1. Expression of cytokeratins and/or EMA by sarcomas
2. Spindle cell carcinoma can express SMA or MSA, and some can show occasional
desmin positive cells.
3. Misinterpretation of background cell reactivity as tumor cell reactivity
- CK reactivity in submesothelial fibroblasts
- Desmin reactivity by mesothelial cells.
- Expression of S100 by histiocytes
- Myogenin reactivity in regenerating skeletal muscle cells
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 14
IMMUNOHISTOCHEMICAL APPROACH TO
UNDIFFERENTIATED MALIGNANT TUMOR.
Initial considerations:
1. Value of looking at H&E first without looking at patient history first.
2. Clinical information can guide your differential diagnosis (age, history, location, etc.)
If prior pertinent pathology exists – try to look at that first.
3. How much tissue do we have to work with, and are clinicians in a big rush?
- If lots of tissue and no rush – sequential rounds of stains OK
- If minimal tissue or big rush – better to “blast away” up front
(cost of more stains is usually < cost of re-biopsy)
4. If minimal tissue – order stains in “order of importance”, and have 10 or more extra
sections cut and held, in case more stains are needed (rather than having to re-face the
paraffin block another time)
5. Use lists to help jog your memory
Useful Initial Panel (if you don’t have a clue what the tumor is):
CK-LMW Sox10 CD45 (LCA) CD43 SYN
CK-HMW MART-1 CD30 (Ki-1) SALL4 CHG
SUMMARY AND CONCLUSIONS
1. Appearances can be deceiving.
2. Importance of good clinical information and review of previous pathology.
3. Importance of panel approach – often need >1 marker per diagnostic category.
4. Be mindful of what you have to work with, and alter your approach accordingly.
5. Use lists so that you won’t forget things as easily.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 15
It must be kept in mind that there are exceptions to everything, and not all
tumors will necessarily react as I have indicated. This underscores the importance
of a carefully performed H&E examination by a skilled anatomic pathologist in
arriving at the correct diagnosis. If the immunostain findings don't make sense when
viewing the H&E, then the immunostain findings should be considered suspect
(especially if the immunostains were performed using so-called "Predilute Ready-To-
Use" antibodies).
Selected References
1. Stevenson AJ, Chatten J, Bertoni F et al: CD99 (p30/32MIC2)
neuroectodermal/Ewing's sarcoma antigen as an immunohistochemical marker.
Review of more than 600 tumors and the literature experience. Applied
Immunohistochemistry 2(4): 231-240, 1994.
2. Renshaw AA: O13 (CD99) in spindle cell tumors. Reactivity with
hemangiopericytoma, solitary fibrous tumor, synovial sarcoma, and meningioma, but
rarely with sarcomatoid mesothelioma. Applied Immunohistochemistry 3(4): 250-
256, 1995.
3. CD34: A review. van de Rijn M, Rouse RV: Applied Immunohistochemistry 2(2):
71-80, 1994.
4. Lumade JA, Askin FB, Perlman EJ: MIC2 analysis of small cell carcinoma.
American Journal of Clinical Pathology 102: 692-694, 1994.
5. Weiss LM, Arber DA, Chang KL: CD68: A review. Applied
Immunohistochemistry 2(1): 2-8, 1994.
6. DeYoung BR, Wick MR, Fitzgibbon JF et al: CD31: An immunospecific marker for
endothelial differentiation in human neoplasms. Applied Immunohistochemistry 1:
97-100, 1993.
7. Lloyd RV, Cano M, Rosa P et al: Distribution of chromogranin A and secretogranin I
(chromogranin B) in neuroendocrine cells and tumors. American Journal of
Pathology 130(2): 296-304, 1988.
8. Miettinen M: Synaptophysin and neurofilament proteins as markers for
neuroendocrine tumors. Archives of Pathology and Laboratory Medicine 111: 813-
818, 1987.
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 16
9. Arber DA, Kandalaft PL, Mehta P et al: Vimentin-negative epithelioid sarcoma. The
value of an immunohistochemical panel that includes CD34. The American Journal
of Surgical Pathology 17(3): 302-307, 1993.
10. Shah IA, Netto D, Schlageter MO et al: Neurofilament immunoreactivity in Merkel
cell tumors: A differentiating feature from small cell carcinoma. Modern Pathology
6(1): 3-9, 1993.
11. 11: Dorfman DM, Pinkus GS: CD99 (p30/32MIC2) immunoreactivity in the
diagnosis of thymic neoplasms and mediastinal lymphoproliferative disorders. A
study of paraffin sections using monoclonal antibody O13. Applied
Immunohistochemistry 4(1): 34-42, 1996.
12. Pinkus GS, Kurtin PJ: Epithelial membrane antigen - A diagnostic discriminant in
surgical pathology. Immunohistochemical profile in epithelial, mesenchymal, and
hematopoetic neoplasms using paraffin sections and monoclonal antibodies. Human
Pathology 16: 929-940, 1985.
13. Sloane JP, Ormerod MG: Distribution of epithelial membrane antigen in normal and
neoplastic tissues and its value in diagnostic tumor pathology. Cancer 47: 1786-
1795, 1981.
14. Lloyd RV, Jin L, Zhang S: Proconvertases 2 and 3 are specific neuroendocrine
markers. Modern Pathology 9(1):173A (abstract #1016), 1996.
15. Folpe AL, Patterson K, Gown A: Antibodies to desmin identify the blastemal
component of nephroblastoma. . Modern Pathology 10(9):895-900, 1997.
16. Nonaka D, Chiriboga L, Rubin BP: Sox10: A Pan-Schwannian and Melanocytic
Marker. The American Journal of Surgical Pathology 32(9): 1291-1298, Sep 2008.
17. Cao D, Guo S, Allan RW et al: SALL4 is a novel sensitive and specific marker of
ovarian primitive germ cell tumors and is particularly useful in establishing yoke sac
tumor from clear cell carcinoma. The American Journal of Surgical Pathology
33(6): 894-904, Jun 2009 .
18. Cao D, Li J, Guo S et al: SALL4 is a novel diagnostic marker for testicular germ cell
tumors. The American Journal of Surgical Pathology 33(7): 1065-1077, Jul 2009 .
19. Liegl B, Hornick JL, Corless CL et al: Monoclonal antibody to DOG1.1 shows higher
sensitivity than KIT in the diagnosis of gastrointestinal stromal tumors, including
unusual subtypes. The American Journal of Surgical Pathology 33(3): 437-446,
Mar 2009.
20. Singer G, Kurman RJ, McMaster MT et al: HLA-G immunoreactivity is specific for
intermediate trophoblast in gestational trophoblastic disease and cancer of as a useful
R.T. Miller, M.D. Diagnostic Immunohistochemistry Page 17
marker in differential diagnosis. The American Journal of Surgical Pathology
26(7): 914-920, Jul 2002.
21. Hornick JL, Cin PD, Fletcher CDM: Loss of INI 1 expression is characteristic of both
conventional and proximal-type epithelioid sarcoma. The American Journal of
Surgical Pathology 33(4): 542-550, Apr 2009.
22. Binh MBN, Sastre-Garau X, de Pinieux G et al: MDM2 and CDK4 immunostainings
are useful adjuncts in diagnosing well-differentiated and dedifferentiated liposarcoma
subtypes. A comparative analysis of 559 soft tissue neoplasms with genetic data. The
American Journal of Surgical Pathology 29(10): 1340-1347, Oct 2005.
23. Terry J, Saito T, Subramanian S et al: TLE1 as a diagnostic immunohistochemical
marker for synovial sarcomas emerging from gene expression profile and studies. The
American Journal of Surgical Pathology 31(2): 240-246, Feb 2007.
24. Buresh CJ, Oliai BR, Miller RT: Reactivity with TDT in a Merkel cell carcinoma. A
potential diagnostic pitfall. The American Journal of Clinical Pathology 129 (6):
894-898. Jun 2008
25. Feldman AL, Dogan A: Diagnostic uses of Pax5 immunohistochemistry. Advances
in Anatomic Pathology 14(5):323-334, Sep 2007.
26. Zynger DL, Dimov ND, Luan C et al: Glypican-3: A novel marker in testicular germ
cell tumors. The American Journal of Surgical Pathology 30(12): 1570-1575, Dec
2006.
27. Santagat S, Ligon K, Hornick JL: Embryonic standard cell transcription factor
signatures in the diagnosis of primary and metastatic germ cell tumors (OCT3/4,
NANOG, and SOX2). The American Journal of Surgical Pathology 31(6): 836-845,
Jun 2007.
J Clin Pathol 2007;60:936-938 doi:10.1136/jcp.2006.044750
Leucocyte common antigen (CD45) and CD5 positivity in an “undifferentiated” carcinoma: a potential diagnostic pitfall
- Nyethane Ngo1,
- Kaushik Patel2,
- Peter G Isaacson3,
- Kikkeri N Naresh4
+ Author Affiliations
-
1Department of Histopathology, Hammersmith Hospital, Imperial College, London, UK
-
2Department of Histopathology, Kingston Hospital, London, UK
-
3Department of Histopathology, University College, London, UK
-
4Department of Histopathology, Hammersmith Hospital, Imperial College, London, UK
- Correspondence to:
 Professor K N Naresh
 Department of Histopathology, Hammersmith Hospital, Du Cane Road, London W12 0HS, UK; k.naresh@imperial.ac.uk
CD45 is a transmembrane protein tyrosine phosphatase located on most haematopoietic cells. It has several isoforms, and haematopoietic cells express one or more of the isoforms—CD45RO, CD45RA and CD45RB.1,2 CD45 immunoreactivity is recognised to be highly specific for non–Hodgkin’s lymphomas.3,4 CD45-expressing non-haemopoietic tumours are very rare. This was first noted by McDonnell et al5 in 1987, who reported a primitive sarcoma expressing CD45. Subsequently, Nandedkar et al6 reported three cases of undifferentiated large-cell, possibly neuroendocrine, carcinomas expressing CD45. Two of them were lymph node metastasis and one was a pulmonary tumour. All the three cases expressed both CD45 and cytokeratin. Two of the cases behaved in an aggressive manner.6
In contrast to CD45, CD5 is expressed in thymic carcinoma and malignant mesothelioma.7,8 To the best of our knowledge, this is the first reported case of a carcinoma expressing both CD45 and CD5.