| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
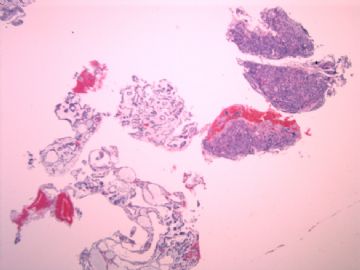
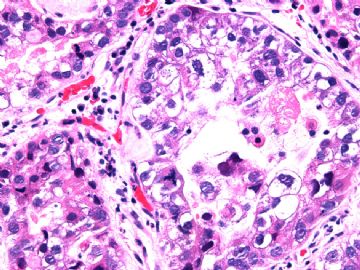
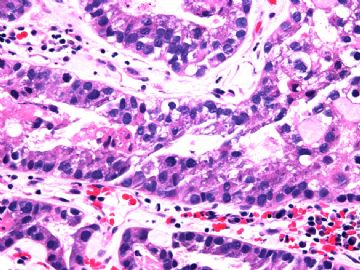
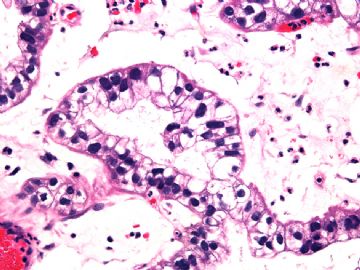
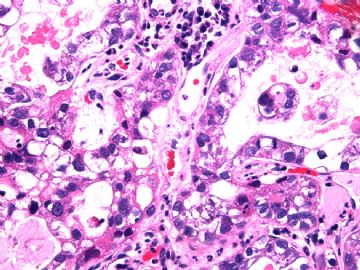
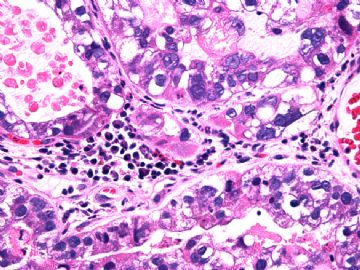
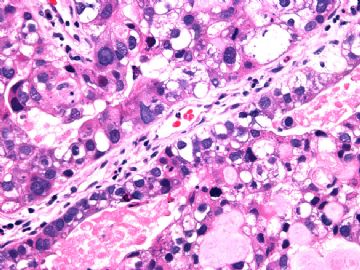
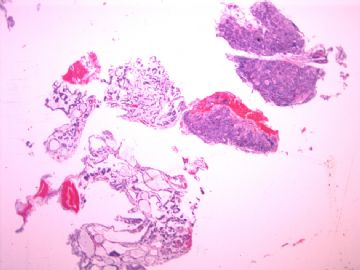
- 女/26岁 孕32周 宫颈肿块
-
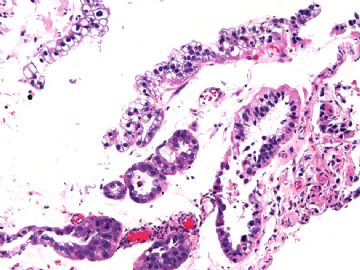
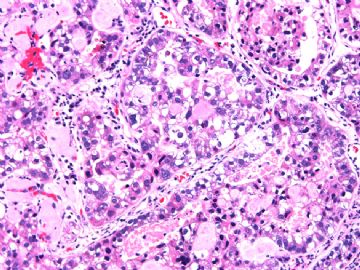
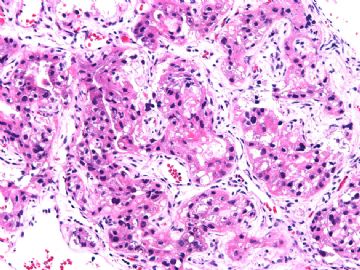
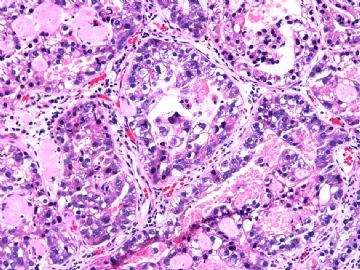
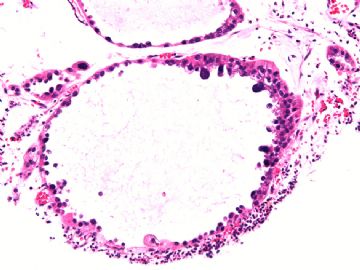
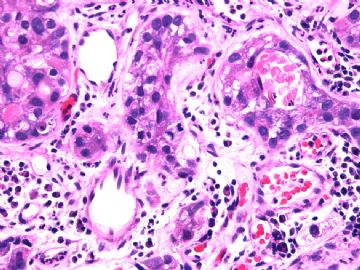
Just as architectural and cytologic similarities between clear cell carcinoma and the Arias-Stella reaction cause problems, so do some differences help resolve them. As is often the case when evaluating endocervical glandular lesions, low power evaluation is important. In cases of Arias-Stella reaction,
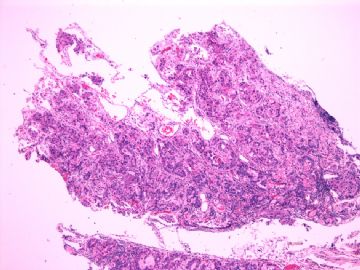
the glandular units have a spatial distribution that is consistent with normal. In contrast, clear cell carcinoma, even when small, often has an irregular distribution of glands in keeping with an invasive process. Although the Arias-Stella reaction may involve adjacent glands imparting a confluent growth pattern, the distribution parallels that of the normal cervical gland architecture. Interpretation of the Arias-Stella change in endocervical polyps is more challenging given that glands within endocervical polyps may be increased in number and have a more disorganized appearance; nevertheless, even in polyps, the spatial distribution of the glands does not suggest invasion. Furthermore, a desmoplastic stromal reaction, often associated with invasive carcinoma, is not seen adjacent to glands exhibiting the Arias-Stella effect. A helpful feature is partial involvement of glands by the Arias-Stella effect, with
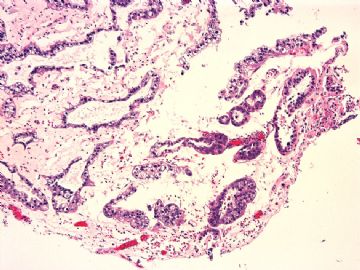
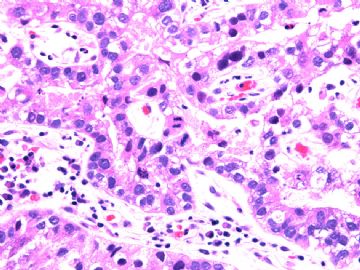
normal-appearing endocervical cells adjacent to and intermixed with cells exhibiting the Arias-Stella reaction . From the cytologic point of view, it is helpful that the hyperchromatic nuclei of the Arias-Stella reaction do not have as conspicuous nucleoli as those of clear cell carcinoma often do. Also, although Dr. Arias-Stella allows mitotic figures in the change that bears his name and others have reported them, they are rare in our experience with this entity, being present in only 1 case in this series in which only 1 mitotic
figure was identified after an exhaustive search of all the cases. Moreover, although described in the Arias-Stella reaction, in our experience atypical mitotic figures are usually not present, and their presence should strongly raise the possibility of a malignant process.
| 以下是引用Liu_Aijun在2010-7-6 22:20:00的发言: clear cell carcinoma |
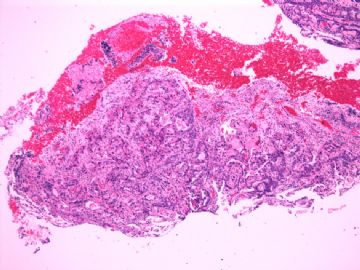
Yes. Classic cervical clear cell carcinoma. No immunostains are needed for this case.
Tubulocystic pattern with intraluminal pink materials, lined with maligant clear cells.
-A-S reaction will not show so diffused change.
-MGH will not show this kind of atypia.
-Cervical yolk sac tumor is one of the differential dx. But YST is much more rare, usually occurs in children and morphology is not support it.
|
尝试翻译,但是感觉有点困难,可能不是很通顺
以下是引用njwbhuang在2010-7-6 22:43:00的发言: Just as architectural and cytologic similarities between clear cell carcinoma and the Arias-Stella reaction cause problems, so do some differences help resolve them. As is often the case when evaluating endocervical glandular lesions, low power evaluation is important. In cases of Arias-Stella reaction, 正是结构和细胞学类似的的透明细胞癌和宫颈腺体A-S反应导致的问题,所以需要做一些鉴别来帮助解决。在评价宫颈内腺体病变时这是经常性的问题,低倍镜的观察是很重要的。在具有A-S反应的病例中,相关腺体具有一种与正常腺体一致的空间分布。相反地,透明细胞癌甚至病灶很小也经常会具有不规则的腺体分布以保持其浸润过程。尽管A-S反应可以包含临近腺体并赋予其一种融合性生长模式,但是其分布于正常宫颈腺体结构平行。宫颈息肉中A-S改变的判读是更具挑战性的,比如宫颈内息肉的腺体可能会有数量的增加和更加异常的组织像;但是,就算是在息肉中,腺体的空间分布并不提示浸润。还有,与浸润性癌密切相关的促结缔组织增生性间质反应,在具A-S反应腺体周围区域是看不到的。一个有帮助的特点是不完全的A-S反应腺体,表现为正常形态的宫颈内细胞临近或穿插于A-S反应的细胞。从细胞学特点来看,浓染核仁在A-S反应细胞中并没有透明细胞癌的显著。尽管Dr.Arias and Dr.Stella 认为分裂像在A-S反应中可见,还有其他的研究者也报道过,但是A-S反应腺体细胞的核分裂在我们一个研究表明很少见。还有,我们经验是A-S反应腺体细胞病理性核分裂像一般并不出现,如果出现将明显提升恶性的可能性。
解读:倾向于透明细胞癌。 猜想:妊娠期,高激素状态,腺癌细胞的so called Arias-Stella reaction.
|
-
本帖最后由 于 2010-07-09 05:09:00 编辑
|
感谢各位专家和网友的宝贵诊断意见。怀孕期宫颈透明细胞癌非常少见,根据最新报导,英文文献仅2例报导(下列参考文献-2)。本病例宫颈有5cm大小的菜花样肿块。HE倾向诊断宫颈透明细胞癌。IHC在进行中,会尽快将结果向大家汇报。 1.Vang R, Barner R, Wheeler DT, Strauss BL. Int J Gynecol Pathol. Immunohistochemical staining for Ki-67 and p53 helps distinguish endometrial Arias-Stella reaction from high-grade carcinoma, including clear cell carcinoma. 2004 Jul;23(3):223-33. Armed Forces Institute of Pathology, Department of Gynecologic and Breast Pathology, Washington, DC, USA. rvang1@yahoo.com The distinction of the Arias-Stella reaction from clear cell carcinoma of the endometrium is usually straightforward; however, this differential diagnosis can be difficult when the Arias-Stella reaction occurs outside the setting of pregnancy or in older patients. The differential diagnosis also is problematic when serous or clear cell carcinoma focally arises within an endometrial polyp, as part of "endometrial intra-epithelial carcinoma" (EIC), or in younger patients. The goal of this study was to determine whether immunohistochemical staining can distinguish the Arias-Stella reaction from endometrial high-grade carcinoma, particularly clear cell carcinoma. Cases of endometrial Arias-Stella reaction (n = 27), clear cell carcinoma (n = 11), serous carcinoma (n = 7), and EIC (n = 4) were assessed by IHC staining with antibodies for Ki-67, p53, estrogen receptor (ER), and progesterone receptor (PR). Composite immunohistochemical scores based on the percentage and intensity of stained cells were calculated, as was the overall positivity (percentage positive cases), using a cutoff value of >/=5% stained cells and at least weak intensity. Appropriate statistical tests were performed. Ki-67 and p53 immunostaining was significantly less in Arias-Stella reaction than in clear cell carcinoma (p < 0.0001 for both) or serous carcinoma/EIC (p < 0.0001 for both), measured by the composite immunohistochemical scores or overall positivity. ER showed a significant difference only between Arias-Stella reaction and clear cell carcinoma; PR showed a significant difference only between Arias-Stella reaction and serous carcinoma/EIC. When clinical or histologic features cannot facilitate the differential diagnosis, immunohistochemical staining for Ki-67 and p53 may help distinguish endometrial Arias-Stella reaction from clear cell carcinoma and other types of high-grade carcinoma.
2.Terada T.Clear cell adenocarcinoma of the uterine cervix in a young pregnant woman: a case report with immunohistochemical study. Med Oncol. 2010 Jan 7. [Epub ahead of print] The patient was a 30-year-old-pregnant woman (para 1, gradiva 1) without in utero exposure to diethylstilbestrol. A papillary and flat lesion was found by colposcopy in the uterine cervix in the routine examination at 10 pregnancy weeks. Biopsies showed papillary and tubular proliferation of malignant cells with clear glycogen-rich cytoplasm and malignant hobnail cells and were diagnosed as clear cell adenocarcinoma. The patient was treated by radical hysterectomy. The lesion of the cervix (10 x 15 x 5 mm) was clear cell adenocarcinoma with mild invasion into shallow myometrium (pTIb). An immunohistochemical study showed that the tumor cells were positive for pancytokeratins (AE1/3, CAM5.2, KL-1, and polyclonal wide), cytokeratin (CK) 7, CK8, CK18, CK19, epithelial membrane antigen, CA 125, p53 protein, and Ki-67 antigen (labeling = 95%). The tumor cells were negative for high-molecular weight CK (34betaE12), CK5/6, CK14, CK20, vimentin, AFP, CEA, desmin, S100 protein, alpha-smooth muscle antigen, CD34, estrogen receptor, progesterone receptor, chromogranin, synaptophysin, euron-specific enolase, and CD56. The patient is now of free of tumor. In the English literature, the present case is the second case of cervical clear cell adenocarcinoma during pregnancy, and the first case of cervical clear cell carcinoma investigating a wide range of immunoreactive antigens.
3.Ahrens WA, Barrón-Rodriguez LP, McKee M, Rivkees S, Reyes-Múgica M. Clear cell adenocarcinoma of the cervix in a child without in utero exposure to diethylstilbestrol: a case report and review of the literature. Pediatr Dev Pathol. 2005 Nov-Dec;8(6):690-5.
4. Nucci MR, Young RH. Arias-Stella reaction of the endocervix: a report of 18 cases with emphasis on its varied histology and differential diagnosis.Am J Surg Pathol. 2004 May;28(5):608-12 We report 18 cases of Arias-Stella reaction involving the endocervix with an emphasis on histologic features that can be encountered and result in the misdiagnosis of carcinoma. The patients ranged in age from 19 to 44 years. Two patients had a history of oral contraceptive use and 15 were pregnant; clinical information was not available in one case. Ten lesions presented as cervical polyps, and six were incidental findings in specimens obtained because of cervical dysplasia, dysfunctional uterine bleeding, fibroids, and a missed abortion. One patient was found to have a cervical "lesion" on a routine gynecologic examination. In the remaining patient, a cervical biopsy was obtained, for unknown reasons, at the time of termination of pregnancy. Microscopic examination showed a varied histologic appearance including vacuolated clear cytoplasm (18 cases), intraglandular tufts (16 cases), hobnail cells (14 cases), oxyphilic cytoplasm (13 cases), delicate filiform papillae (12 cases), intranuclear pseudoinclusions (10 cases), cribriform intraglandular growth (3 cases), and a single mitotic figure in 1 case. The histologic changes involved the superficial glands (6 cases), deep glands (4 cases), or both (8 cases); confluent or extensive gland involvement was seen in 8 cases. Follow-up information, available in four cases (4, 2, 1, 1 years), was unremarkable. The principal consideration in the differential diagnosis was clear cell carcinoma. The features most helpful in this distinction were 1)the usual lack of a mass suspicious for cancer, 2)absence of a desmoplastic response, 3)lack of an infiltrative pattern, 4)spectrum of cytologic atypia, 5)low nuclear-cytoplasmic ratio, and 6)usual lack of mitotic activity.
5. Ordi J, Romagosa C, Tavassoli FA, Nogales F, Palacin A, Condom E, Torné A, Cardesa A. CD10 expression in epithelial tissues and tumors of the gynecologic tract: a useful marker in the diagnosis of mesonephric, trophoblastic, and clear cell tumors.
Am J Surg Pathol. 2003 Feb;27(2):178-86. 6. Miller DM, Schouls JJ, Ehlen TG. Clear cell carcinoma arising in extragonadal endometriosis in a caesarean section scar during pregnancy. Gynecol Oncol. 1998 Jul;70(1):127-30.
7.Hanselaar A, van Loosbroek M, Schuurbiers O, Helmerhorst T, Bulten J, Bernhelm J. Clear cell adenocarcinoma of the vagina and cervix. An update of the central Netherlands registry showing twin age incidence peaks. Cancer. 1997 Jun 1;79(11):2229-36. 8.Sugiyama T, Nishida T, Kataoka A, Okura N, Iwanaga S, Yakushiji . A pregnant woman with clear cell adenocarcinoma of the ovary arising from endometriosis and with benign and borderline adenofibroma of the clear cell and endometrioid types. Eur J Obstet Gynecol Reprod Biol. 1997 Mar;72(1):47-50. 9. Gynecol Oncol. 1996 Mar;60(3):339-44. p53 protein expression and gene analysis in clear cell adenocarcinoma of the vagina and cervix. Waggoner SE, Anderson SM, Luce MC, Takahashi H, Boyd J. 10. Waggoner SE, Anderson SM, Van Eyck S, Fuller J, Luce MC, Herbst AL.Human papillomavirus detection and p53 expression in clear-cell adenocarcinoma of the vagina and cervix. Obstet Gynecol. 1994 Sep;84(3):404-8.
|

- xljin8
-
xingrongge 离线
- 帖子:42
- 粉蓝豆:11
- 经验:425
- 注册时间:2010-04-18
- 加关注 | 发消息
-
本帖最后由 于 2010-07-09 05:54:00 编辑
宫颈Arias-Stella反应鉴别诊断(主要参考19楼文献-4)
*虽然在分娩后子宫的宫颈内口ASR发生率仅为10%,但始终存在鉴别诊断问题。在Nucci 和Young最大组研究中(18例),病人年龄为19-44岁,除二例口服避孕药外,其他均为孕期妇女。
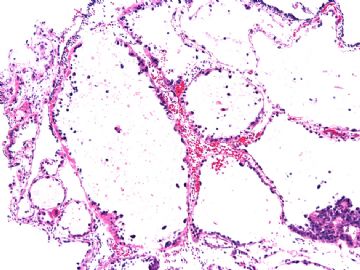
*ASR几乎总是显微镜下偶然发现,常发生在宫颈内口息肉中。一般ASR累及一个或几个腺体,但偶尔ASR的范围非常广泛。可累及浅表和/或深部腺体。
*显微镜下表现与内膜ASR类似。Nucci和Young注意到下列特点,依降序为:空泡化透明细胞质、腺体内上皮细胞簇、靴钉样细胞、嗜酸性胞质、纤细的丝状乳头、核内假包涵体、筛状结构、18例中仅一例有一个核分裂象。
*病理医生如果不知道患者怀孕,可能与宫颈原位腺癌(AIS)或透明细胞癌(CCC)混淆,特别是活检小标本和刮宫破碎标本。
*ASR 与AIS鉴别:ASR表现为透明细胞和靴钉细胞、无普遍的核不典型性、极少或无核分裂象。
*ASR与CCC鉴别:ASR临床病理特点为年轻孕妇、临床缺乏症状或肿块、组织学无浸润、无管囊状和实体结构、无透明轴心乳头、无间质反应、无明显异形性和核分裂象。

- xljin8