| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 系统学病理及英语病理学之一
1a Chronic Pancreatitis
Chronic pancreatitis is characterized by patchy fibrous replacement of whole lobules or parts of lobules, focal fat necrosis in different stages, and chronic inflammation. Grossly, depending on the etiology and degree of injury, the gland may be slightly firm but have a normal outline, lobular pattern, and color. Severe cases may be smaller than normal, bosselated, rock-hard, and display foci of fat necrosis, calcification, or fully developed calculi.
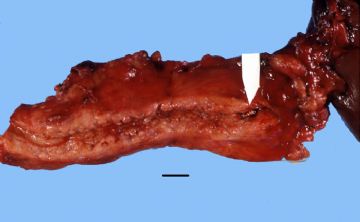
Gross: This chronically inflamed pancreas is small and scarred. The dilated pancreatic duct contains a stone (arrow). Chronic Pancreatitis with stone
onmouseover="showMenu(this.id, 0, 1)"> X-ray: This is an example of chronic pancreatitis with marked calcification of the pancreatic parenchyma. This calcification could be demonstrated by an x-ray of the abdomen.
onmouseover="showMenu(this.id, 0, 1)"> Gross: These are cross sections taken through the head of the pancreas in chronic pancreatitis. The sections of pancreas which you have in your class sets were taken in a similar fashion. Notice that the dense white fibrous scarring has almost totally obliterated the lobular architecture of the pancreas.
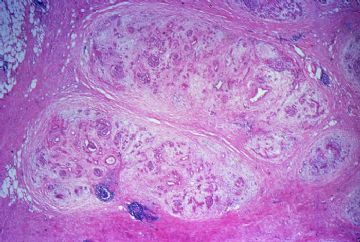
onmouseover="showMenu(this.id, 0, 1)"> This is a low magnification picture of the H&E slide of chronic pancreatitis in your class set. This particular patient had an obstructive type of pancreatitis due to carcinoma of the head of the pancreas. The lobular architecture of the pancreas is accentuated by broad bands of interstitial fibrosis.
onmouseover="showMenu(this.id, 0, 1)"> The fibrous scarring of the pancreas is highlighted with the Trichrome stain. The fibrous septa appear as blue bands surrounding the residual pancreatic lobules, which stain red.
The fibrous scarring of the pancreas is highlighted with the Trichrome stain. The fibrous septa appear as blue bands surrounding the residual pancreatic lobules, which stain red. Shows the dense interstitial fibrosis surrounding two pancreatic lobules. Note there is also an increase in intralobular fibrous tissue and there is chronic inflammation.
Shows the dense interstitial fibrosis surrounding two pancreatic lobules. Note there is also an increase in intralobular fibrous tissue and there is chronic inflammation.
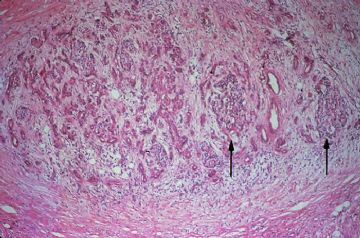
onmouseover="showMenu(this.id, 0, 1)"> The exocrine portion of the gland is most severely affected. There is almost total atrophy and fibrous replacement of pancreatic acini with relative preservation of the pancreatic ducts and islets of Langerhans (arrows). The intralobular pancreatic ductules are irregularly shaped and are embedded in chronically inflamed fibrous tissue. Several preserved islets are marked with arrows
The exocrine portion of the gland is most severely affected. There is almost total atrophy and fibrous replacement of pancreatic acini with relative preservation of the pancreatic ducts and islets of Langerhans (arrows). The intralobular pancreatic ductules are irregularly shaped and are embedded in chronically inflamed fibrous tissue. Several preserved islets are marked with arrows
Higher magnification shows preservation of the islets of Langerhans to better advantage (arrows).

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
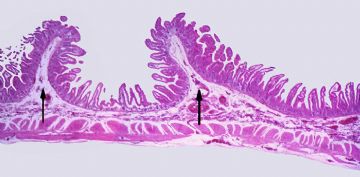
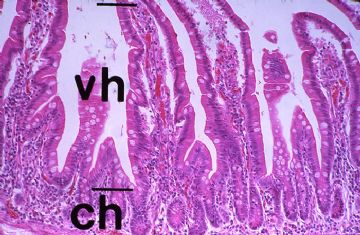
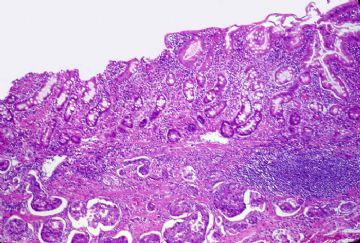
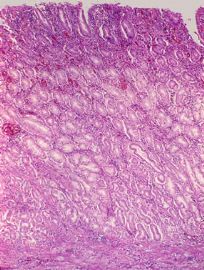
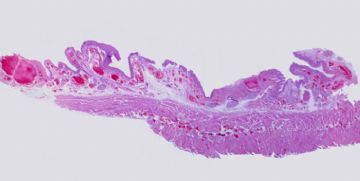
A low power view of the glass slide in your class set. The mucosa of the jejunum is thrown into plical folds (arrows) which are covered with the intestinal villi that measure 0.5 to 1.5 mm in length.
Regularly spaced in the valleys between the villi, and numbering some 2-3 per villus, are the straight, tubular intestinal glands or crypts of Lieberkuhn. Given individual variation, the average villus height (VH) to crypt height (CH) in the jejunum is about 6:1. This ratio should always be assessed when evaluating small bowel biopsies because many malabsorptive diseases are characterized by villus atrophy with subsequent decrease in the villus height to crypt height ratio.
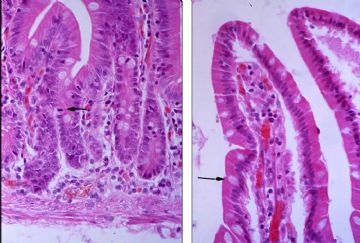
The left panel shows the intestinal crypts at high magnification. The lower half of the crypts contains mostly undifferentiated cells with a high mitotic rate. One mitotic figure is noted by the arrow. As the villus epithelium of the intestine is shed, there is upper displacement and differentiation of cells generated from the undifferentiated basal epithelium. The entire process of cell division, migration, and maturation takes about 2-6 days.The right panel shows the villous epithelium at high magnification. As the undifferentiated cells of the crypt migrate up into the villus, they differentiate into the absorptive cells covered by a microvillus brush border and into mucin-secreting goblet cells (arrow). Note the lacteal in the central core of the villus.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Gross: Linitis plastica carcinoma diffusely infiltrates the entire gastric wall without forming an intraluminal mass. The wall of the stomach is typically thickened to about 2-3 cm. and has a leathery, inelastic consistency.
A low power view of the slide in your class set. Poorly differentiated carcinoma arises from the mucosa and diffusely infiltrates all layers of the gastric wall.
This is a higher magnification showing effacement of the lamina propria of the gastric mucosa by adenocarcinoma.
A higher magnification showing the malignant epithelial cells extending through the muscularis propria.
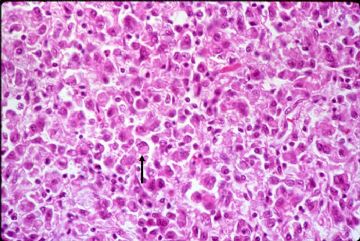
Higher magnification of the carcinoma shows it to be composed of diffuse sheets of loosely cohesive, slightly pleomorphic epithelial cells with large nuclear-to-cytoplasmic ratios. This is a poorly differentiated adenocarcinoma in that no glands are formed, but you will notice that some of the cells contain a mucin vacuole that displaces the nucleus to the periphery to form the so-called "signet cell" (arrow).

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
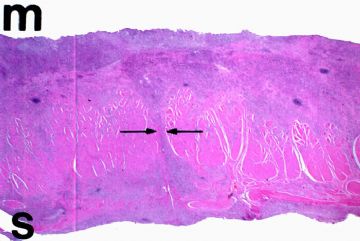
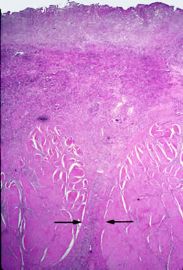
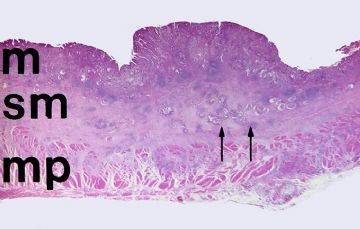
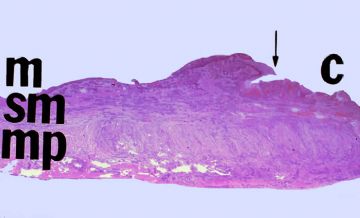
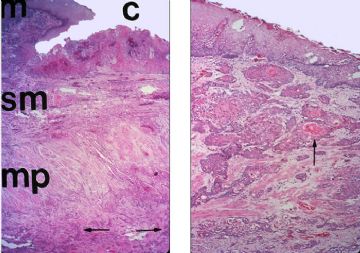
A low power photograph of the slide in your class set. The mucosa "M", submucosa (SM), muscularis propria (MP), and serosa are all readily apparent. At this magnification you can see an adenocarcinoma that extends into the submucosa (double arrows).
The left panel shows a moderately differentiated adenocarcinoma arising from the mucosa. The islands of malignant cells in the submucosa have invaded into lymphatic channels (arrows).
Higher magnification in the right panel shows that the gastric mucosa has been largely replaced by adenocarcinoma. The malignant gland that is marked by the double arrows is seen at higher magnification in Slide 3.
Note the complex pattern of this malignant gland. Whereas a benign gland is lined by a single layer of cells, the malignant gland is hypercellular. This results in the stratification of malignant cells with the formation of an irregular, thickened gland wall. Small, accessory glandular lumina form in the wall of the major gland to form the so-called "gland-within-gland" pattern. Also note the irregular size and shape ("pleomorphism") of the nuclei of the malignant cells and the increased mitoses.
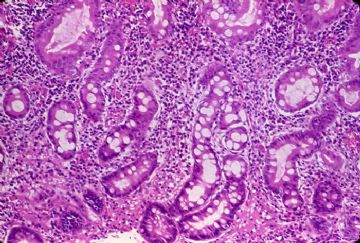
The gastric mucosa adjacent to the carcinoma shows chronic inflammation, glandular atrophy and distortion, and intestinal metaplasia. These findings are typical for chronic atrophic gastritis. As you know, atrophic forms of gastritis with intestinal metaplasia show an increased incidence of gastric cancer.
Shows the intestinal metaplasia of the gastric mucosa at higher power. Note that the foveolar epithelium of the gastric mucosa has been replaced by absorptive cells and mucin-secreting goblet cells typical of the intestinal mucosa. There is also intense chronic inflammation of the lamina propria

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Gross: Chronic peptic ulcers are typically small (less than 4 cm in diameter), round, sharply punched-out lesions with perpendicular walls and a clean base. Fibrous contracture of the base of the ulcer may cause puckering of the surrounding mucosal folds such that they radiate away from the ulcer in spoke-like fashion. A perpendicular histologic section taken through the plane of the yellow bar would appear like that show in the next.
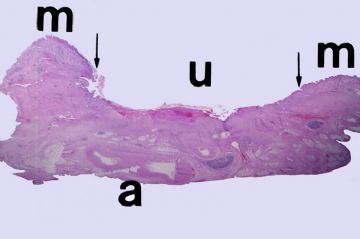
A low power view of the gastric ulcer in your class set. The ulcer (U) lies between the arrows. The intact, but chronically inflamed, gastric mucosa (M) is on both sides. Note that the base of the ulcer extends all the way to the serosa of the stomach. Large arteries (A) are present at the base of the ulcer. Erosion into one of these large arteries could result in massive hematemesis.
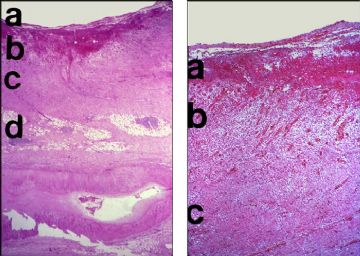
The left panel is a low power view of the full thickness of the gastric wall in the region of the ulcer. This ulcer shows ongoing necrosis, inflammation, and fibrous repair that can be divided into 3 layers. "A" represents the superficial layer of necrotic debris and acute inflammation. Just below this superficial layer is a zone of active granulation tissue (B), which in the deeper layers matures into a fibrous scar (C). The fibrotic subserosal adipose tissue is noted by the letter "D". Again, notice the large artery at the base of the ulcer.
The right panel shows the layers of the ulcer at higher magnification. "A" represents the superficial zone of necrosis and active inflammation, "B" the zone of active granulation tissue, and "C" the deep fibrous scar.
The mucosa adjacent to the ulcer shows chronic gastritis. Note the discrete band of chronic inflammation in the most superficial portion of the mucosa.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Gross: This is an example of an ulcerated squamous cell carcinoma of the esophagus. It differs from a benign peptic ulcer of the esophagus because it is much larger and it has irregular borders, rather than being sharply punched-out. Note the perforation in the center.
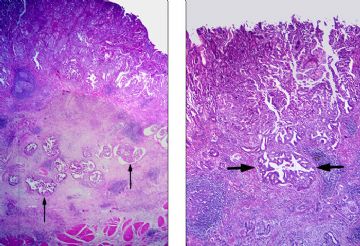
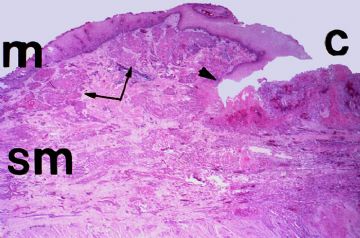
It is a low power view of the histologic section in your class set. (M = mucosa; Sm = submucosa; Mp = muscularis propria). The intact mucosa is to the left of the arrow; the ulcerated carcinoma (C) is to the right.
It is taken at the juncture (arrow head) of the normal mucosa (M) and the ulcerated carcinoma (C), and it shows another common feature of esophageal cancer. The gross margins of the cancer are often misleading because the tumor frequently spreads longitudinally within submucosal lymphatics (double arrows).
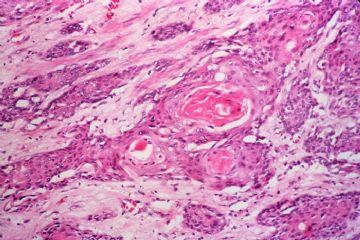
This left panel shows a histologic section taken through the full thickness of the esophageal wall. Carcinomas of the esophagus are typically deeply infiltrating lesions and this one has extended through the muscularis propria (arrows).
The right panel shows nests of malignant squamous cells within the submucosa. This is a moderately differentiated squamous cell carcinoma which shows keratin production. The malignant cells show a common feature of malignancy, namely altered polarity. The differentiating squamous cells within the submucosal nests cannot slough keratin to the luminal surface. Instead, the keratin accumulates in the center of the nests as spherical keratin "pearls" (arrow).
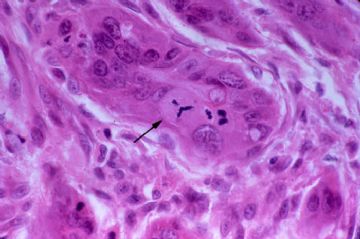
Shows the moderately differentiated squamous cell carcinoma with keratin pearls at higher power.
Mitotic figures are usually common in malignant tumors and often they are abnormal. This is a tripolar mitosis. If you look carefully, you can see 3 mitotic spindles.

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Esophageal Varices
onmouseover="showMenu(this.id, 0, 1)">

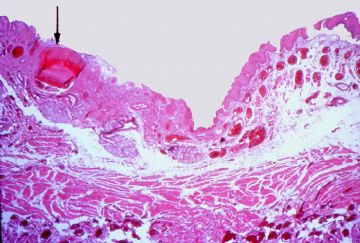
This is a photograph of the actual histologic slide in your class set. Note the markedly dilated veins in the submucosa and in the muscularis propria of the esophagus.
onmouseover="showMenu(this.id, 0, 1)">

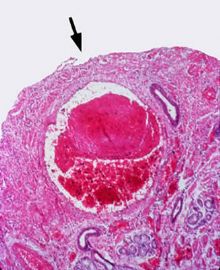
These dilated varices often cause pressure atrophy and ulceration of the overlying mucosa, as has happened in this case. The subsequent inflammation of the submucosa causes erosion of the thin wall of the varices with subsequent rupture. The large varix noted by the arrow communicates directly with the lumen and has probably ruptured in the past. It is now thrombosed.
onmouseover="showMenu(this.id, 0, 1)">

Shows thrombosis of a large submucosal varix. Note the ulceration of the overlying mucosa (arrow) and inflammation of the submucosal stroma.
onmouseover="showMenu(this.id, 0, 1)">


- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Adenocarcinoma of the Pancreas
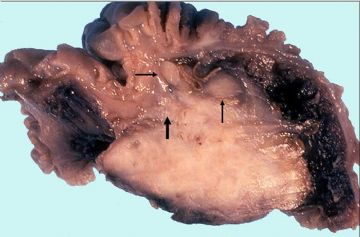
Gross: This section is taken through an adenocarcinoma of the head of the pancreas. The lesion is a firm, tan-white mass that effaces the normal lobular architecture of the pancreas. Although this carcinoma is only about 2.5 cm in diameter, it has already invaded into the wall of the duodenum (large arrow) and metastasized to regional lymph nodes (small arrows).
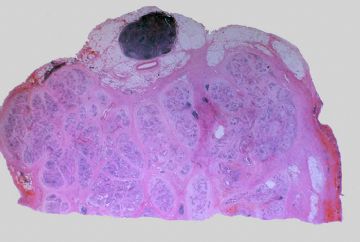
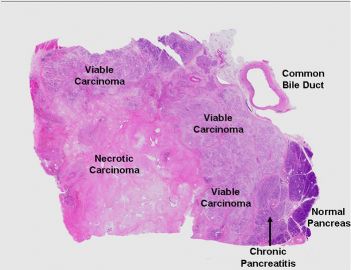
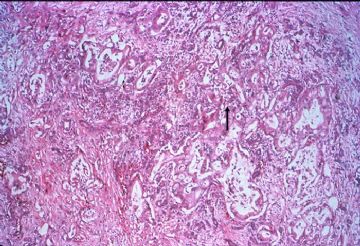
This is a low power view of the histologic slide in your class set. This is a section taken through the head of the pancreas from a patient with a ductal type of adenocarcinoma. The viable tumor is peripherally located around a central core of necrosis. Immediately adjacent to the tumor, the pancreas shows chronic pancreatitis (arrow). One normal pancreatic lobule is seen at the extreme right hand edge of the slide. The slide which you have contains a section taken through the extrapancreatic portion of the common bile duct (CD).
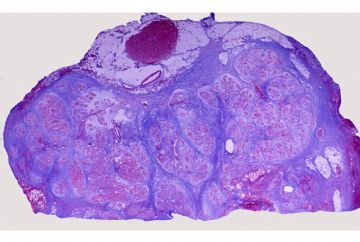
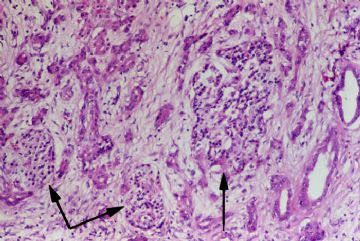
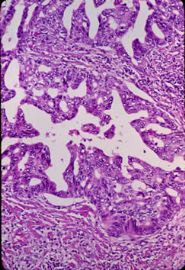
onmouseover="showMenu(this.id, 0, 1)"> This low power view shows a moderately differentiated adenocarcinoma. Irregularly shaped malignant glands are embedded in chronically inflamed fibrous tissue. Adenocarcinomas of the pancreas typically excite this type of fibrous reaction (“desmoplasia”) in the surrounding tissue. When palpated, the tumor may be extremely hard, making it virtually impossible to differentiate from chronic pancreatitis
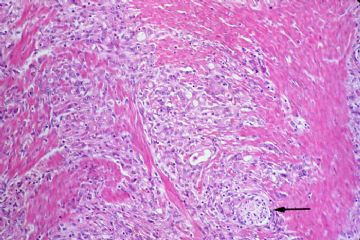
This low power view shows a moderately differentiated adenocarcinoma. Irregularly shaped malignant glands are embedded in chronically inflamed fibrous tissue. Adenocarcinomas of the pancreas typically excite this type of fibrous reaction (“desmoplasia”) in the surrounding tissue. When palpated, the tumor may be extremely hard, making it virtually impossible to differentiate from chronic pancreatitis
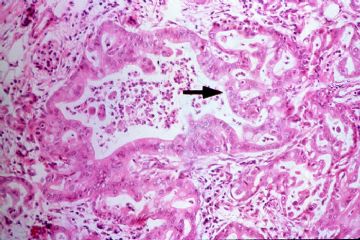
onmouseover="showMenu(this.id, 0, 1)"> This is a higher power view of a malignant gland. It is lined by pleomorphic cells which pile-up to form secondary lumina (gland-within-gland formation). Bridges of neoplastic epithelium grow across the major lumen of the gland (arrow).
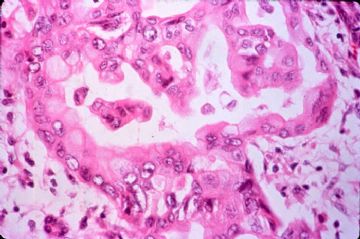
This is a higher power view of a malignant gland. It is lined by pleomorphic cells which pile-up to form secondary lumina (gland-within-gland formation). Bridges of neoplastic epithelium grow across the major lumen of the gland (arrow). At higher magnification, note the nuclear pleomorphism of the neoplastic cells lining the glands.
At higher magnification, note the nuclear pleomorphism of the neoplastic cells lining the glands.
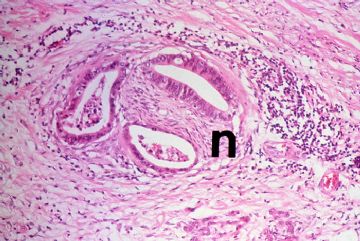
onmouseover="showMenu(this.id, 0, 1)"> Perineural invasion is extremely common in carcinoma of the pancreas. Unfortunately, infiltration into the peripancreatic fat, mesenteric vessels, duodenal wall, common bile duct, and other contiguous structures such as the stomach, spleen, portal vein, peritoneal cavity is also common. Regional lymph node metastases are almost always present at the time of diagnosis.
Perineural invasion is extremely common in carcinoma of the pancreas. Unfortunately, infiltration into the peripancreatic fat, mesenteric vessels, duodenal wall, common bile duct, and other contiguous structures such as the stomach, spleen, portal vein, peritoneal cavity is also common. Regional lymph node metastases are almost always present at the time of diagnosis. 
onmouseover="showMenu(this.id, 0, 1)">

- 赚点散碎银子养家,乐呵呵的穿衣吃饭