| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- Pap test with cervical bx result
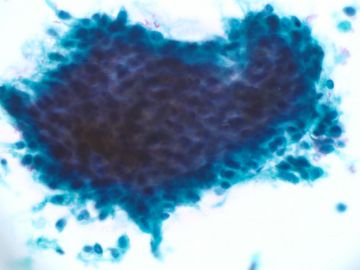
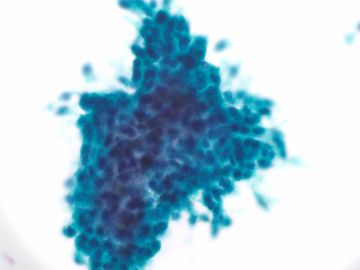
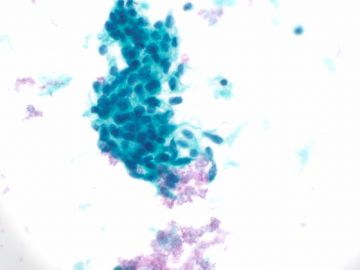
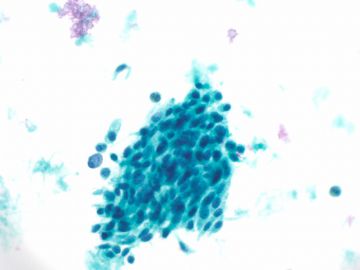
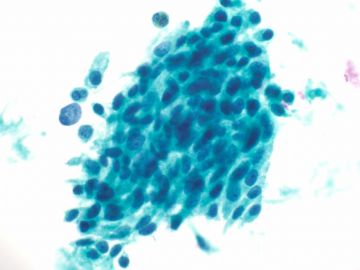
Last week I had a cervical bx case. I found the patient's recent Pap smear. I feel it is interesting case. Just take some photos and share with you here.
67 y women, Pap was negative in 2006, endometrial bx with endometrial polyp in 2007.The followings are the Pap last month. (上周有了这个病例的活检,并复习了这个病人最近的巴氏涂片。感觉这个病例很有意思,在这里贴些图片跟大家分享。病史:67岁女性,2006年涂片阴性,2007年子宫内膜活检为内膜息肉。这是上个月的巴氏随访涂片。)
Fig 1-4 400x
Fig 5 600x
-
本帖最后由 于 2009-12-02 09:46:00 编辑
| 以下是引用青青子矜在2009-12-20 21:39:00的发言:
很有意思的病例。 每次赵老师的病例都有陷阱,结果总是出人意料,所以大家都不敢轻易回答,下次我们来个逆向思维,反着答就对了,呵呵! 深染细胞群的鉴别在宫颈细胞是个难点,所以我一直很想有散在细胞的对照。赵老师连续三次发照片,可能有临床经验的已经可以猜测到组织学结果。但本例细胞学的确是有很多腺分化的特征,鳞病变的证据不足,更何况赵老师的经验也是——“AGC的组织学随访结果与年龄分布有相关性,40岁以下多数为鳞状上皮病变,40-50岁组别中鳞和宫颈腺病变相似,50岁以上者中子宫内膜肿瘤最常见。”(我从赵老师书上学来的,现学现卖) 有时腺鳞的鉴别的确非常困难,组织学上还有腺样鳞癌呢,更何况细胞学。私下认为这样的病例报鳞和腺都不是大问题,最主要不漏诊,不能放过,结合临床进一步检查即可。
|
说的很好!向青青子矜学习!
感谢赵老师!

- 王军臣
| 以下是引用青青子矜在2009-12-20 21:39:00的发言:
很有意思的病例。 每次赵老师的病例都有陷阱,结果总是出人意料,所以大家都不敢轻易回答,下次我们来个逆向思维,反着答就对了,呵呵! 深染细胞群的鉴别在宫颈细胞是个难点,所以我一直很想有散在细胞的对照。赵老师连续三次发照片,可能有临床经验的已经可以猜测到组织学结果。但本例细胞学的确是有很多腺分化的特征,鳞病变的证据不足,更何况赵老师的经验也是——“AGC的组织学随访结果与年龄分布有相关性,40岁以下多数为鳞状上皮病变,40-50岁组别中鳞和宫颈腺病变相似,50岁以上者中子宫内膜肿瘤最常见。”(我从赵老师书上学来的,现学现卖) 有时腺鳞的鉴别的确非常困难,组织学上还有腺样鳞癌呢,更何况细胞学。私下认为这样的病例报鳞和腺都不是大问题,最主要不漏诊,不能放过,结合临床进一步检查即可。
|

- 掌心0164
-
本帖最后由 于 2009-12-23 09:20:00 编辑
| 以下是引用掌心0164在2009-12-20 13:10:00的发言: 盼星星盼月亮终于盼来了赵老师最终的结果。回过头来总结我还是那句话:细胞学是组织学的片段。对我来说,有时需要解释病例的时候是痛苦的;因为没有组织学基础;单纯从细胞学看细胞学会时不时感觉到力不从心。现在我想请赵老师您从细胞学和组织学结合起来整个思路的分析给我们讲述一下。谢谢赵老师完整而精彩的病案。 |
-
本帖最后由 于 2010-01-07 22:44:00 编辑
Share several points (分享几点:)
1. Clinical hx is important: old women with vaginal bleeding(临床病史很重要:老年女性伴有阴道流血)
2. positive HR-HPV testing(高危HPV检测阳性)
2. Several clusters of hyperchromatic crowded groups (HCGs) of cells impliy the presence of a high-grade lesion(一些深染拥挤细胞团表明可能出现在高度病变中)
3. Very few normal squamous cells are not normal pap(非常少的正常鳞状上皮细胞是不正常的涂片)
4. Something-like tumor diathesis background (背景中的肿瘤样素质)
5. Cell, nuclear shape: more spindles than columnar(细胞、核形:比柱状上皮更多的呈纺锤形)
6. It is easy to appreciate nucleoli.(核仁明显)
7. It is true the case shows some features of glandular and squamous lesion. If you observed carefully, cytologic features of the case favor more squamous lesion then glandular lesion(实际病例中有一些鳞状病变和腺病变的特征。如果你自己观察,这例的细胞特征更倾向于鳞状病变而不是腺病变。)
8. If it is squmous lesion, it should be HSIL or invasive ca. Clearly it is not like a classic HSIL case. Tumor diathesis and nucleoli are two important features to distinguish invasion from HSIL or in situ ca.(如果是鳞状病变,应该是HSIL或浸润癌。显然这不是一个典型的HSIL病例。肿瘤素质和核仁是鉴别HSIL和浸润癌的两个重要特征。)
9. It is a difficult case for cytologic disgnosis. I think it is acceptable if we call this case as ASC-H, AGC, AGC-FN. Bottomline is that you need to contact with clinician to make sure the women had tissue biopsy. It is a bad call if you call asc-us or negative for this case. It is better to study more before you sign out Pap case independly(这是一个细胞学诊断疑难病例。如果我们叫这个病例为ASC-H、AGC或AGC-FN是可接受的。底线是你必须跟临床沟通让这个病例有组织学活检。如果叫ASCUS或阴性是比较糟糕了。在你独立签发巴士涂片报告之前需要更多的学习。)
10. Pap is a screening test. In your clinical practice, until you are 100% sure it is squamous carcinoma or adenocarcinoma, please do not use the term.(巴氏涂片是一个筛查。在您的临床实践中,除非您能100%肯定是鳞癌或腺癌,否则请不要用那么肯定的术语。)
11. It is not unusual that we meet the cases in clinic that patients with invasive squamous ca had true negative Pap within few years. It means that some invasive cases can develop very quickly, but not like the usual way, step by step: HPV-CIN1-CIN2/3-invasion.(我们在临床工作中遇到几年前巴氏确实是阴性而几年后是浸润性鳞癌的病例并不少见。这表明一些浸润病例可以进展很快,但是不像普通的进展模式,逐步进展:HPV-CIN1-CIN2/3-浸润。)
-
本帖最后由 于 2009-12-23 10:21:00 编辑
In our hospital (most hospitals in the US, cytotechnicians read Pap firstly, called primary screen, all abnormal Pap including reactive change et al will give pathologists to review and sign out. Cytotechnician input their interpretation in computer system, pathologists can make the final decision for the diagnosis. I can change whatever I like for final diagnosis. However, the primary interpretation of cytotechnicians can still be found in computer system. (在我们医院<美国的大多数医院>,细胞技术员先读巴氏涂片,也叫初筛;所有异常的涂片包括反应性改变都要给病理医生复核和签发报告。细胞技术员把他们自己的结果输入电脑系统中,病理医生做出最后诊断。我无论什么时候都可以更改最后诊断,但是技术员最初的结果仍然会在我们的系统中。)
For this case, the interpretaion of cytotech was invasive carcinoma and the case was singed out by our pathologist as AGC-FN. This pathologist called gynecologist to discuss the risk of cancer. Often cytotechnicians have more accurate diagosis. It is a pressure for pathologists to change cytotechnicans' interpretation. Of cause cytotech often over call. It is not a problem for cytotech to over call, but it is problem for them to low call or miss call.(这个病例,技术员的结果是浸润性癌但是我们病理医生最后签发的是AGC-FN。病理医生跟妇科医生讨论了叫癌的风险。通常细胞技术员会诊断得更准确,病理医生更改技术员的结果时面临很大的压力。当然技术员经常过诊,对技术员来说过诊没有关系,但是低诊或漏诊是大问题。)
-
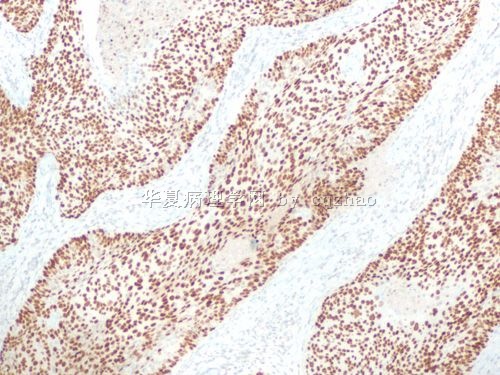
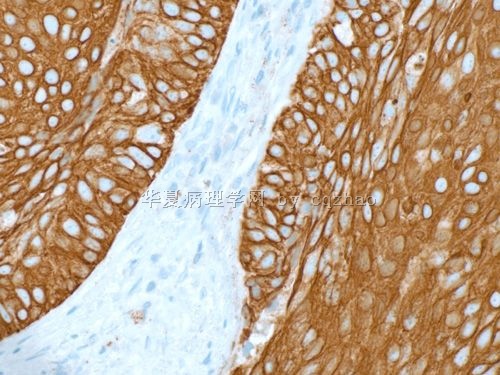
本帖最后由 于 2009-12-23 10:29:00 编辑
When I had biopsy I reviewed the Pap. Also I showed them to the pathologist who signed out the Pap. She still thought there are some glandular feature in biopsy. Please check the last histologic photo above. There are some nuclear palisading, feathering in the edges.(当我看活检片子的时候复阅了巴氏涂片。我也让签发巴氏报告的病理医生看了活检的片子。她仍然认为活检是腺的病变。请回顾前面的组织学照片。有一些核呈栅栏状、羽状边缘。)
For this reason I did squamous marker stains(因为这我做了鳞状标记)
-
本帖最后由 于 2009-12-23 10:41:00 编辑
I hope people know that Pap test is most difficult area for cytopathologists even though a lot of people think it is very easy to read Pap (like several hundred Pap/day, need only a few days or few weeks of training for reading Pap). We all need to gradually 积累our experience in practice. We always need to think patient's clinical presentaion and previous Pap test and related history.(即使很多人认为阅巴氏涂片很容易<像每天阅几百张巴氏涂片,阅巴氏片只需要几天或几周的培训>,我仍然希望大家知道巴氏涂片对细胞病理医生来说是最困难的领域。我们需要逐步的从实践中积累经验。我们需要考虑病人临床表现、过往的巴氏涂片和相关的病史)
We need to know what clinicans will do based on our Pap interpretation.".(我们要知道基于我们的巴氏结果,临床医生会做什么处理。)
In fact I spent several hours on this topic and hope our pathologists or technicians to know only one thing "Pap test is a screening test(我花几个小时在这个主题是希望我们病理医生或技术员明白一件事情“巴氏试验是一个筛查试验”。)
Ok, I think I finish my duty for this case. Thank 掌心0164 ,青青 and all others who attended discussion, translation and read this topic.(好了。我认为我已经完成了这个病例。感谢掌心0164 ,青青子矜和所有参与讨论、翻译和阅读这个主题的网友。)
cz
| 以下是引用青青子矜在2009-12-22 23:26:00的发言:
赵老师讲解得真好,非常感谢! 尤其是评论鳞分化多于腺分化的一句话: Cell, nuclear shape: more spindles than columnar,很有启发,多谢!我当时看有腺分化时只是看到了部分细胞群边缘的明显羽化。 还有关于细胞技术员与细胞病理医生关系的评论,很有意思,呵呵! 来不及翻译,但我想我们细胞栏的同仁们英文都不错,有需要翻译的朋友们找掌心同学吧 |

- 掌心0164
| 以下是引用掌心0164在2009-12-23 10:50:00的发言:
|
-
本帖最后由 于 2010-01-07 22:46:00 编辑
| 以下是引用cqzhao在2009-12-22 22:34:00的发言:
Share several points (分享几点:) 1. Clinical hx is important: old women with vaginal bleeding(临床病史很重要:老年女性伴有阴道流血) 2. positive HR-HPV testing(高危HPV检测阳性) 2. Several clusters of hyperchromatic crowded groups (HCGs) of cells impliy the presence of a high-grade lesion(一些深染拥挤细胞团表明可能出现在高度病变中) 3. Very few normal squamous cells are not normal pap(非常少的正常鳞状上皮细胞是不正常的涂片) 4. Something-like tumor diathesis background (背景中的肿瘤样素质) 5. Cell, nuclear shape: more spindles than columnar(细胞、核形:比柱状上皮更多的呈纺锤形) 6. It is easy to appreciate nucleoli.(核仁明显) 7. It is true the case shows some features of glandular and squamous lesion. If you observed carefully, cytologic features of the case favor more squamous lesion then glandular lesion(实际病例中有一些鳞状病变和腺病变的特征。如果你自己观察,这例的细胞特征更倾向于鳞状病变而不是腺病变。) 8. If it is squmous lesion, it should be HSIL or invasive ca. Clearly it is not like a classic HSIL case. Tumor diathesis and nucleoli are two important features to distinguish invasion from HSIL or in situ ca.(如果是鳞状病变,应该是HSIL或浸润癌。显然这不是一个典型的HSIL病例。肿瘤素质和核仁是鉴别HSIL和浸润癌的两个重要特征。) 9. It is a difficult case for cytologic disgnosis. I think it is acceptable if we call this case as ASC-H, AGC, AGC-FN. Bottomline is that you need to contact with clinician to make sure the women had tissue biopsy. It is a bad call if you call asc-us or negative for this case. It is better to study more before you sign out Pap case independly(这是一个细胞学诊断疑难病例。如果我们叫这个病例为ASC-H、AGC或AGC-FN是可接受的。底线是你必须跟临床沟通让这个病例有组织学活检。如果叫ASCUS或阴性是比较糟糕了。在你独立签发巴士涂片报告之前需要更多的学习。) 10. Pap is a screening test. In your clinical practice, until you are 100% sure it is squamous carcinoma or adenocarcinoma, please do not use the term.(巴氏涂片是一个筛查。在您的临床实践中,除非您能100%肯定是鳞癌或腺癌,否则请不要用那么肯定的术语。) 11. It is not unusual that we meet the cases in clinic that patients with invasive squamous ca had true negative Pap within few years. It means that some invasive cases can develop very quickly, but not like the usual way, step by step: HPV-CIN1-CIN2/3-invasion.(我们在临床工作中遇到几年前巴氏确实是阴性而几年后是浸润性鳞癌的病例并不少见。这表明一些浸润病例可以进展很快,但是不像普通的进展模式,逐步进展:HPV-CIN1-CIN2/3-浸润。) |
最好的病例!最好的讲解!最好的老师!





















受益匪浅啊!谢谢赵老师!