| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B228135岁 乳腺肿物
-
shihong4699 离线
- 帖子:1024
- 粉蓝豆:43
- 经验:2917
- 注册时间:2009-01-20
- 加关注 | 发消息
For above case:
If it were my case I will definitely do
1. Make sure taqht metastatic tumor in one axillary lymph node is true.
2. stain myoepithelial markers to make sure if invasive component is present.
3. If no invasion is noted in the available slides, entire specimen should be submitted for microscopic examination. For a mass 5*4*2.5 cm, about 40 blocks may be enough.
请教楼主:
What is the size of the tumor in lymph node?
Is it lobular ca?
Generally people talk about DCIS with microinvasion. LCIS with microinvasion is more rare.
Positive axillary lymph node can be present in mcroinvasive ca, but the chance is much lower than macroinvasive ca.
The reasons that patients with carcinoma in situ have positive lymph nodes include 取材不够,or invasive componnet in patients' breasts.
We need to submit all exsional biopsy specimens to confirm the absence of invasion.
-
本帖最后由 于 2009-11-15 21:56:00 编辑
Definition:
1.
American Joint Committee on Cancer (AJCC) TNM staging system, microinvasive carcinoma of the breast (MICB) has been defined as follows: “the extension of cancer cells beyond the basement membrane into the adjacent tissue with no focus more than 0.1 cm in greatest dimension. In this system, the presence of multiple foci of MICB is to be noted, but the addition of sizes of individual foci of microinvasion is not allowed.
2 WHO pathology book consider that Tmic a single focus of invasive carcinoma < 2 mm or up to 3 foci < 1 mm in greatest dimensions. Tavassoli is main editor in WHO breast book. Her definition for Tmic was published in Cancer 1998, Silver and Tavassoli.
I think AJCC definition is better.
首先, 非常感谢Shihong医师为我提供了这样一例判断”小叶原位癌是否有早期浸润”的好教材, 能和大家一起学习、讨论、研究和提高。有以下思考, 供参考:
1) 腋下淋巴结1/22有癌转移(转移癌是否为小叶癌形态?), 表明原发灶内一定存在浸润性癌, 它要么是取材未取到或在石蜡组织块中切片未切到, 要么是我们”视而不识”, 癌细胞太”狡猾”。
2) 原发病灶5X4X2.5cm, 颗粒状? 一般认为: 小叶原位癌在临床上是难以触及到肿块的, 能否提供一张大体照片,显示一下癌灶的大小?
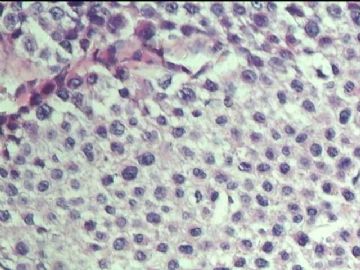
3) 就提供的9张镜下照片来分析:
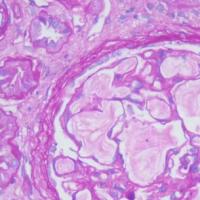
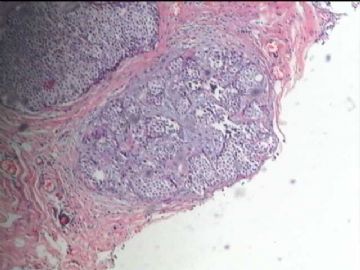
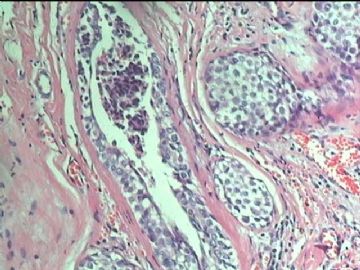
图1低倍示2个明显扩大的被癌细胞充实的末端导管-小叶单元;
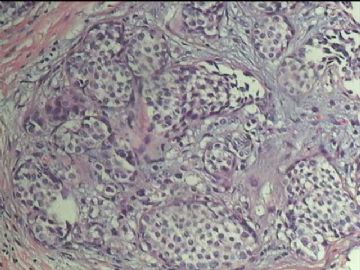
图2中倍可见小叶内部分癌巢外形不规则, 小叶内间质粘液变性和纤维增生, 细胞数量增多, 其间散在单个的异型细胞;
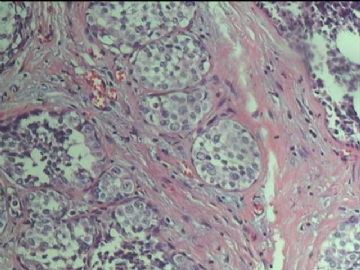
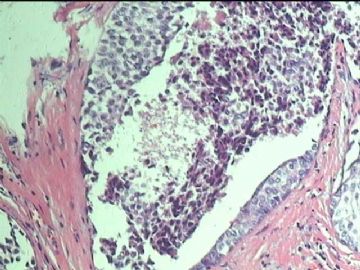
图3、4、5、6都有肿瘤细胞的坏死;
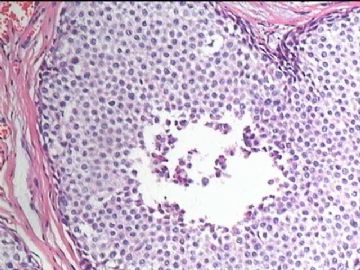
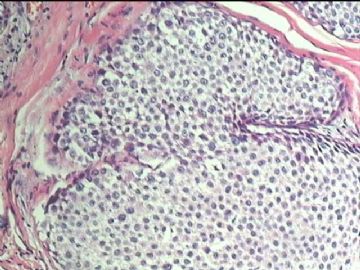
图7、9为癌细胞向外蘑菇形的突出,
图8血管淋巴管旁少量异型细胞。
4) 高度怀疑图2小叶间质内有微浸润, 图3图4小叶间间质有微浸润;
5) 因此, 建议IHC标记AE1/AE3和CK7来寻找浸润的癌细胞。因为小叶原位癌微浸润在常规HE切片中可很象”炎症细胞”和”间质细胞”, 靠光镜观察很难鉴别,非常容易漏诊; 有时“间质细胞的增多”是提示微浸润的唯一线索。
文献报导病理诊断为”导管原位癌/小叶原位癌”的病例, 腋窝淋巴结的转移率约为10%。因为病理医师不能常规的去检查整个肿瘤标本的全部切片, 很有可能漏掉微小的浸润灶。我们的工作越仔细, 漏诊的可能性就越小, 这就要挑战自己。
对于冰冻诊断中如何鉴别是否存在微浸润, 从技术上讲是非常困难或不可能, 与手术医师良好的沟通是关键。
如果观察到微浸润, 病理报告中应该表明最大直径(?1mm, ?2mm. ?5mm)和病灶数量(?);和鉴定微浸润的方法((HC标记?).
最后用我国一位最著名的软组织病理专家的一句格言与大家共勉”病理医师诊断不是靠眼睛看出来的, 而是靠鼻子嗅出来的”

- xljin8
-
mingmei_77 离线
- 帖子:37
- 粉蓝豆:11
- 经验:73
- 注册时间:2009-03-27
- 加关注 | 发消息
1)小叶原位癌(无浸润)- 小叶原位癌+微浸润(浸润灶小于1mm)-浸润性小叶癌(浸润灶大于1mm)是小叶癌进展的不同阶段。* 浸润灶大小1mm - 1cm 定义为微小浸润(minimal invasive)
2)微浸润是指很少量的癌细胞突破基底膜浸润间质(小叶内或小叶之间)。
3)提示微浸润可能的形态学表现:旺殖性增生的小叶原位癌伴有a)末端导管- 小叶结构的明显增大;b) 出现坏死和钙化; C)小叶癌巢的边缘不规则;d) 边缘有促结缔组织反应。
4)确定微浸润的方法是证明癌细胞已突破基底膜(Laminin和IV型胶原)进入到间质,这意味着癌细胞可以侵犯淋巴管和血管,已具备淋巴道转移的可能性。
5)明确基底膜不完整可用电镜和IHC(标记Laminin和IV型胶原); 肌上皮细胞消失也是可参照的指标之一(最好用同时用p63和SMM HC)。
6)证明间质中的癌细胞用CK标记,特别是CK7 和AE1/AE3。
7)本病例有哪些形态提示可能存在微浸润?
8)您能从提供的镜下照片中找到吗?

- xljin8
-
miracle008 离线
- 帖子:5
- 粉蓝豆:1
- 经验:5
- 注册时间:2009-11-11
- 加关注 | 发消息