| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
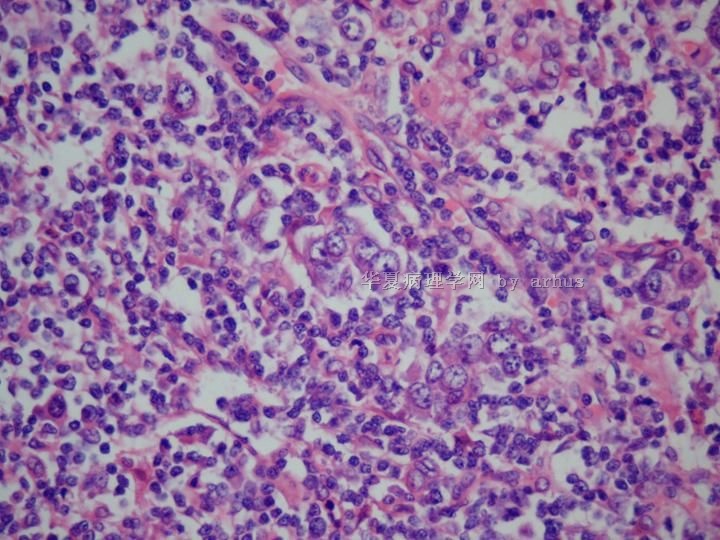
- 左锁骨上淋巴结活检-会4609
| 姓 名: | ××× | 性别: | 男 | 年龄: | 68 |
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
名称:图1
描述:图1
名称:图2
描述:图2
名称:图3
描述:图3
名称:图4
描述:图4
名称:图5
描述:图5
名称:图6
描述:图6
名称:图7
描述:图7
名称:图8
描述:图8
名称:图9
描述:图9
名称:图10
描述:图10
标签:
-
本帖最后由 于 2009-10-22 20:32:00 编辑
×参考诊断
淋巴结转移癌
-
chenliu0552 离线
- 帖子:502
- 粉蓝豆:22
- 经验:985
- 注册时间:2010-12-10
- 加关注 | 发消息
-
ZQH19811029 离线
- 帖子:458
- 粉蓝豆:1
- 经验:458
- 注册时间:2009-11-15
- 加关注 | 发消息
-
1)并不否定诊断转移性癌.
2)提供的病史似乎原发灶可能是胰腺,但"淋巴结癌细胞"并没有胰腺癌的形态学特点,
3)尽管形态学不象癌,IHC标记结果CK+诊断转移癌的正确率可能高达99.9%;
但是病理医师也应警惕0.1% 可能不是转移癌.我国是个人口大国,罕见病例的绝对
数应该高于国外,但是我国的报道却佷少,为什么?
4)DR.arhus很有经验,是否再深层次的讲解一下此例与"cytokeratin positive interstitial
reticulum cell tumor"鉴别诊断.因为CPIRCT非常罕见,我国仅南京周晓军教授在中华医学 (英文版)上发表一例.
5)参考文献:
1. Kwon JE, Yang WI, Kim HK,et al. Cytokeratin-positive interstitial reticulum cell sarcoma: a case report with cytological, immunohistochemical, and ultrastructural findings. Cytopathology. 2009;20:202-5.
2.Dong YC, Wu B, Sheng Z, et al. Cytokeratin-positive interstitial reticulum cell tumors of lymph nodes: a case report and review of literature. Chin Med J (Engl). 2008;121:658-63.
3.Schuerfeld K, Lazzi S, De Santi MM, et al.
Cytokeratin-positive interstitial cell neoplasm: a case report and classification
issues. Histopathology. 2003;43:491-4.
AIMS: Tumours of dendritic/accessory cell origin are rare neoplasms arising in
lymph nodes. Among these, tumours derived from cytokeratin-positive interstitial
reticulum cells (CIRCs), a subset of fibroblastic reticulum cells, are reported
even less frequently. The International Lymphoma Study Group (ILSG) has recently
proposed a classification for tumours of histiocytes and accessory dendritic
cells in which CIRC tumours are not included. We report a case of a CIRC tumour
arising in a submandibular lymph node of a 66-year-old male. METHODS AND RESULTS:
The neoplasm was composed of spindle cells with elongated or round nuclei,
prominent nucleoli and abundant cytoplasm. These cells were arranged in a diffuse
fascicular and vaguely whorled pattern. The tumour cells stained diffusely for
S100, vimentin, desmin, lysozyme, and focally for CD68 and cytokeratins 7, 8, 18,
CK-AE1 and CK-pool. Electron microscopy was performed for further evaluation on
samples taken from the paraffin block; this revealed cytoplasmic projections and
rudimentary cell junctions. CONCLUSIONS: Histopathologist should be aware of the
existence of tumours deriving from CIRCs, as these cases may be misdiagnosed as
metastatic carcinoma. Careful clinical and pathological evaluation is necessary
to exclude this possibility.
4.Lucioni M, Boveri E, Rosso R, et al. Lymph node reticulum cell neoplasm with progression into cytokeratin-positive interstitial reticulum cell (CIRC) sarcoma: a case study. Histopathology. 2003;43:583-91.
AIMS: To detail on sequential biopsies the morphological and immunohistochemical
features of a case of primary lymph nodal fibroblastic reticulum cell (FBRC)
tumour which progressed into a clinically aggressive cytokeratin-positive
interstitial reticulum cell (CIRC) sarcoma. METHODS AND RESULTS: A 70-year-old
female underwent surgical excision of an enlarged submandibular lymph node. The
nodal architecture was effaced by a neoplastic proliferation of medium to large
cells, round to oval to spindle in shape, growing in a storiform pattern. The
tumour stained for vimentin, CD68, factor XIIIa, alpha1-antitrypsin, fascin and
actin. Dendritic and endothelial cell markers were negative. A diagnosis of FBRC
tumour was made by combining pathological and clinical data. The patient received
no therapy but 5 months later the tumour relapsed, exhibiting a deceptively
pleomorphic cytology, phenotypic changes (strong cytokeratin positivity), intense
p53 expression and aggressive clinical course with fatal outcome. In-situ
hybridization for Epstein-Barr virus was negative. CONCLUSIONS: We speculate that
the morphological changes and p53 expression of the relapsing neoplasm might
reflect tumour cell dedifferentiation, in keeping with the aggressive clinical
course. The intense p53 expression suggests that this oncoprotein might also play
a role in reticulum cell tumorigenesis.
5. Chan AC, Serrano-Olmo J, Erlandson RA, Rosai J.
Cytokeratin-positive malignant tumors with reticulum cell morphology: a subtype
of fibroblastic reticulum cell neoplasm?
Am J Surg Pathol. 2000;24:107-16.
Cytokeratin-positive interstitial reticulum cells (CIRCs) have been described as
a subset of fibroblastic reticulum cells (FBRCs) normally found in lymph nodes,
the spleen, and tonsils. Although tumors derived form other reticulum (dendritic)
cells, specifically follicular dendritic cells, interdigitating dendritic cells,
and cytokeratin-negative FBRCs, have been well documented and are now accepted,
this is not the case for tumors of CIRCs. A possible reason for this failure is
the difficulty in distinguishing them from other tumors, particularly carcinoma.
We report three cases of cytokeratin-positive malignant tumors with a reticulum
cell morphology: two located in the mediastinum and one in the soft tissue in the
proximal forearm. All cases coexpressed vimentin, and one case coexpressed smooth
muscle actin and desmin, resulting in a phenotype similar to that of some normal
CIRCs. Although metastatic carcinoma from an occult or regressed primary tumor
cannot be excluded completely, we raise the possibility of a CIRC origin for
these cases.
6. Gould VE, Bloom KJ, Franke WW, et al.Increased numbers of cytokeratin-positive interstitial reticulum cells (CIRC) in reactive, inflammatory and neoplastic lymphadenopathies: hyperplasia or induced expression?
Virchows Arch. 1995;425:617-29.
A total of 291 enlarged lymph nodes showing a range of reactive-inflammatory
processes, primary and metastatic neoplasms were studied to determine the
distribution and immunoprofile of their cytokeratin-positive interstitial
reticulum cells (CIRC) in comparison with normal nodes. In 258/291 nodes (89%),
CIRC numbers were distinctly increased in the subcapsular, paracortical and,
occasionally, in the medullary zones; often, these increased CIRC formed networks
around follicles, sinuses and vessels. CIRC had comparatively small, irregularly
shaped bodies and dendritic processes; occasionally, giant forms were noted. CIRC
contained cytokeratins (CK) 8 and 18 but not 19, as shown by immunohistochemistry, and by gel electrophoresis with subsequent immunoblotting. They co-expressed vimentin consistently, alpha-smooth-muscle actin frequently,and desmin less frequently. They did not contain desmoplakins, Factor VIII,S-100, LCA, B and T lymphocyte- and macrophage-associated antigens, chromogranin A, synaptophysin or the A-80 glycoprotein. We found no clear correlation between the increased CIRC and given nodal disease processes. However, CIRC were most
abundant in nodes free of but draining malignant tumours; bizarre CIRC assemblies
were noted in HIV lymphadenopathy. CIRC appear to represent a subset of the
so-called "fibroblastic reticulum cells" of lymph nodes. Their function remains
undetermined; their increase in diverse lymphadenopathies suggests that they
partake in nodal reactions to injury. It remains unclear whether the increase in
CIRC relative number is due to proliferation or to CK gene induction processes
but their presence and potential capability to undergo hyperplasia with
dysplastic forms should alert pathologists to possible diagnostic pitfalls. In
addition, we discuss that CIRC may undergo transformation and represent the "cell
of origin" of certain CK-positive tumours restricted to lymph nodes.

- xljin8
-
lanyueliang 离线
- 帖子:679
- 粉蓝豆:11
- 经验:1424
- 注册时间:2008-11-12
- 加关注 | 发消息