| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
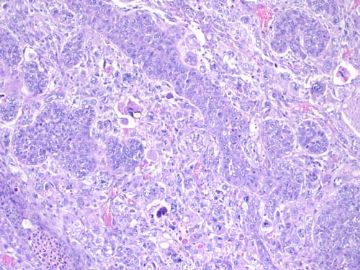
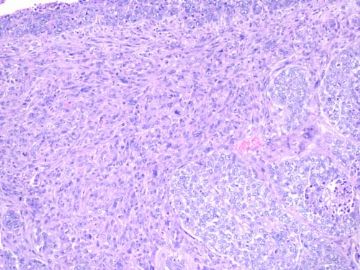
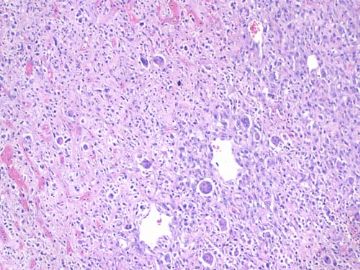
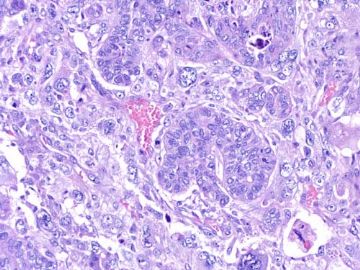
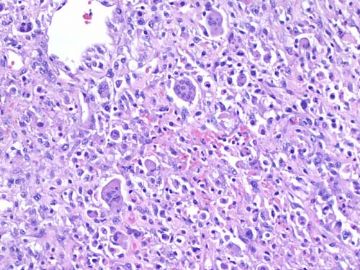
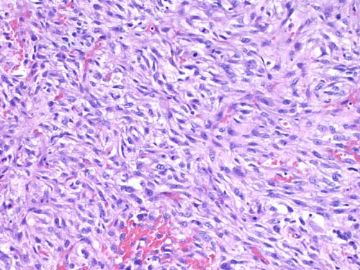
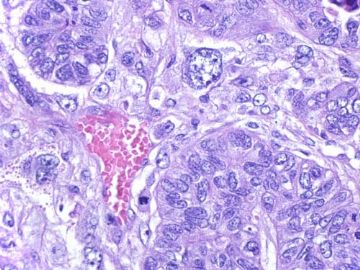
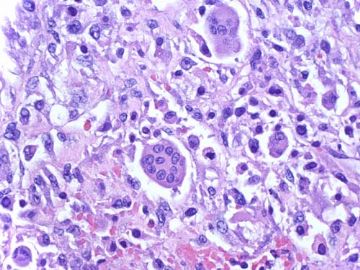
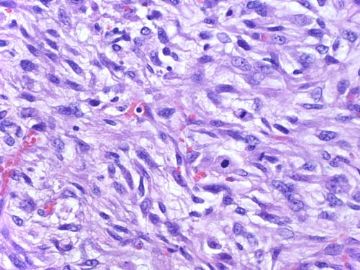
- B2188乳腺化生性癌 with 巨细胞and梭形细胞diffentiation (cqz-25)(8-12-2009)
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
40y/f, breast mass 12 cm.
Your diagnosis?
-
本帖最后由 于 2009-09-17 02:32:00 编辑
相关帖子
- • 左乳腺肿块
- • 乳腺肿物2---诊断?
- • 乳腺化生癌?
- • 06年的一例乳腺癌,什么类型?
- • 乳腺肿物
- • 化生性癌?
- • 女 60岁 乳腺6*7大小 切面半囊半实 红褐色
- • 可否诊断基底细胞样乳腺癌?
- • 右乳腺肿块
- • 右乳肿块,新加免疫组化结果
-
本帖最后由 于 2009-09-17 02:04:00 编辑
I think I can conclude this case. The purpose I pasted this case is to demonstrate the relation between basal-like ca and metaplastic ca.
1. They are two different diagnostic categories using different methods.
2. Based on the definiton of basal-like ca, most of metaplastic carcinomas will belong to the family of basal-like ca.
3. Basal-like carcinoma is a heterogenous group of ca including the classic basal-like ca, most metaplastic ca, most medullary ca and others.
4. Currently there is no special treatment for basal-like ca.
5. For classic metaplastic ca (even though they are triple negative and some basal-like marker positive), we still call metaplastic ca, but not basal-like ca.
6. For classic basal-like ca, currently we call invasive ductal ca with basal-like phenotype.
Above just for your reference.
Thank all of you.
-
The majority of triple-negative breast cancer may correspond to basal-like carcinoma, but triple-negative breast cancer is not identical to basal-like carcinoma.
Department of Diagnostic Pathology, Kochi Red Cross Hospital, 2-13-51 Shin-honmachi, Kochi, 780-8562, Japan. kurochankochi@yahoo.co.jp
Recently, the concept of basal-like carcinoma has been proposed. However, there are only a few reports about the relationship between triple-negative cancer and basal-like carcinoma. In this article, we report the study of the expression of basal cell markers in 11 triple-negative cancers. Eight tumors (4 metaplastic carcinomas, 2 invasive ductal carcinomas, 1 invasive papillary carcinoma, and 1 medullary carcinoma) were positive for more than three markers among cytokeratins 5, 14, and 17, and p63. Three tumors (2 invasive ductal carcinomas and 1 apocrine carcinoma) were completely negative for all markers. Among 8 tumors positive for basal markers, cytokeratins 5 and 17 were expressed in all 8 tumors, cytokeratin 14 in 6 tumors, and p63 in 7 tumors. Finally, we conclude that the majority of triple-negative cancer may correspond to basal-like carcinoma, but the two entities are not identical. The use of combination immunohistochemistry including cytokeratins 5, 14, and 17 and p63 may contribute to the detection of basal-like carcinoma.
Med Mol Morphol. 2009 Jun;42(2):128-31. Epub 2009 Jun 18.
-
Med Mol Morphol. 2008 Jun;41(2):117-20. Epub 2008 Jul 1.
-
Basal-like carcinoma of the breast: further evidence of the possibility that most metaplastic carcinomas may be actually basal-like carcinomas.
Department of Diagnostic Pathology, Kochi Red Cross Hospital, 2-13-51 Shin-honmachi, Kochi, Japan. kurochankochi@yahoo.co.jp
Some investigators have previously suggested that basal-like carcinoma may consist of components of invasive ductal carcinoma, not otherwise specified, metaplastic carcinoma, and medullary carcinoma. We report here two cases of breast carcinoma showing basal cell/myoepithelial differentiation. The first case was a 58-year-old Japanese woman and the second case was a 39-year-old Japanese woman. The two tumors were composed of the proliferation of epithelial cells and/or spindle-or stellate-shaped cells on the background of mucinous materials. Additionally, chondroid matrix was observed in the metastatic lesion of the first case and the primary lesion of the second case. Immunohistochemically, epithelial neoplastic cells were positive for E-cadherin and cytokeratin CAM5.2, and epithelial and spindle-or stellate-shaped cells were positive for cytokeratins 5, 14, or 17, alpha-smooth muscle actin, S-100, and p63. Our results supply further evidence that most metaplastic carcinomas may be actually be basallike carcinomas.
-
J Clin Pathol. 2008 May;61(5):553-60. Epub 2008 Mar 6.
-
Basal carcinoma of the breast revisited: an old entity with new interpretations.
Institute of Pathology, University of Muenster, Germany.
The introduction of global gene expression analysis in breast cancer research has focused attention onto a repeatedly described subgroup of invasive breast cancer, the basal-like carcinomas. This subgroup is characterised by the expression of high-molecular weight cytokeratins 5, 14 and 17; using immunohistochemical diagnosis, it represents approximately 7-20% of invasive breast cancers. Some of these tumours fulfil the criteria of grade 3 invasive ductal carcinoma, the so-called triple negative carcinomas. However, other rare subgroups of metaplastic, medullary and myoepithelial carcinomas also belong to this entity. Even though the initial clinical prognostic relevance of basal-like breast cancers may have been overestimated, its distinctive biology generates many questions regarding the pathogenesis, chemosensitivity and optimal clinical management of this subgroup. Physiological progenitor cells within the normal female breast share essential immunohistochemical features with basal-like breast cancers. Although the exact relationship between subgroups of normal breast cells and their respective malignant counterparts is still under investigation, the major hallmarks of physiological progenitor cells are either maintained or reactivated by distinct genetic changes in basal breast cancer cells. This review will discuss the impact of these findings on our global understanding of breast cancer pathogenesis, especially from the perspective of its potential histogenesis. Clinical consequences and potential future research directions driven by the definition of basal breast cancers will also be discussed.
-
Am J Surg Pathol. 2008 Mar;32(3):345-53.
-
- Erratum in:
- Am J Surg Pathol. 2009 Feb;33(2):322.
Laminin 5 expression in metaplastic breast carcinomas.
The Department of Pathology and Laboratory Medicine, The University of California, Orange, CA 92868, USA. pmcarpen@uci.edu
Metaplastic carcinoma of the breast shows squamous, sarcomatous, or chondromatous differentiation and has a poor prognosis. Laminin 5 is a heterotrimer of alpha3, beta3, and gamma(2) [corrected] chains and induces aggressive properties in cancer cells including motility, invasion, and epithelial to mesenchymal transition. Twenty-five cases included 7 squamous, 4 sarcomatous, 8 chondroid, 1 fibromatosislike metaplastic carcinomas, and 5 cases with 2 metaplastic components. Tumors were stained with laminin 5-specific beta3 and gamma(2) [corrected] chain, p63, and cytokeratin 5/6 (CK 5/6) antibodies. All 4 antibodies stained normal myoepithelium. Both laminin 5 antibodies stained 24/25 (96%) of the tumors, with an identical distribution of the 2 chains in 87.5% of the positively staining cases. In contrast, p63 and CK 5/6 stained 68% and 64% of the tumors, respectively. By comparison, only 16% of high-grade carcinoma controls stained for laminin 5. Similar to the metaplastic carcinomas, all 12 triple negative tumors, those negative for estrogen receptor, progesterone receptor, and Her2/neu, expressed laminin 5. None of 4 breast sarcomas stained for either of the laminin 5 chains or CK 5/6, but 1 (25%) stained for p63. Laminin 5 expression in metaplastic and other basal-like carcinomas is of interest for several reasons. First, these data provide additional evidence of the myoepithelial and basal-like phenotype of these carcinomas. Second, these are the only breast carcinoma subtypes to demonstrate laminin 5 staining in a large proportion of cases. Third, expression of laminin 5 in metaplastic carcinomas may suggest a mechanism for their increased aggressiveness and epithelial to mesenchymal transition phenotype. Finally, compared with other myoepithelial markers, laminin 5 is more sensitive than those previously published. Thus laminin 5 may be helpful for making the diagnosis of metaplastic carcinomas in biopsies, allowing the potential for aggressive early treatment. Further study of other basal-like tumors for laminin 5 expression is warranted to determine the usefulness of laminin 5 in their diagnosis.
-
Anticancer Res. 2007 Jan-Feb;27(1B):547-55.
-
Differential immunohistochemical and biological profile of squamous cell carcinoma of the breast.
Department of Medical Oncology, Institut Gustave Roussy, 39 rue Camille Desmoulins, 94805 Villejuif. julien.grenier@hmn.aphp.fr
BACKGROUND: Pure or metaplastic squamous cell carcinoma (SCC) of the breast is a rare entity with an unclear pathogeny and aggressive clinical behaviour. An attempt was made to characterize its differential immunohistochemical and biological profile. PATIENTS AND METHODS: Twenty-seven cases of SCC (pure or not) of the breast were matched with 27 ductal invasive carcinomas (IDC) for age, tumour size, nodal involvement and year of diagnosis. The expression levels of oestrogen receptor (ER), progesterone receptor (PR), Ki-67, epidermal growth factor receptor (EGFR), HER2, Cyclin Bl, hTERT, cytokeratins (CK) 5/6 and p63 were determined immunohistochemically in both cohorts. The presence of the human papilloma virus (HPV) genome was investigated by polymerase chain reaction (PCR). RESULTS: Pure and metaplastic SCC displayed common profiles typifying a basal origin: they never expressed ER or PR, were HER2-negative in 93% of cases, exhibited positivity for CK5/6 or EGF-R in 75% and 85%, and for p63 in 70% of cases and were highly proliferative. These profiles were markedly different from those of matched controls (p<0.001 for five markers) except for HER2 and hTERT. The HPVgenome was detected in 2 out of 14 cases (14%) of SCC. CONCLUSION: The expression profile of SCC of the breast was markedly different from that of IDC. A typical "basal-like" phenotype was displayed that may explain part of their behaviour and justify specific therapeutic approaches. HPV infection was not a leading oncogenic event in SCC of the breast.
-
Hum Pathol. 2006 Sep;37(9):1217-26. Epub 2006 Jul 18.
-
Clinicopathologic significance of the basal-like subtype of breast cancer: a comparison with hormone receptor and Her2/neu-overexpressing phenotypes.
Deparment of Pathology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 138-736, South Korea.
DNA microarray profiling studies have led to the classification of invasive breast carcinoma into luminal/estrogen receptor-positive, normal breast-like, Her2/neu-overexpressing, and basal-like types. Among these groups, the basal-like subtype is associated with the poorest clinical outcome in Western countries. To date, the clinicopathologic characteristics of the basal-like carcinomas, compared with other subtypes, have not been described in the Korean population. In this study, we used tissue microarray to examine the expression of basal cytokeratins (CK) (CK5 and CK14) and luminal CK (CK8/18), epidermal growth factor receptor, c-kit, hormone receptors (HRs), p53, and Her2/neu in 776 consecutive patients diagnosed with invasive breast carcinoma from January 1993 to December 1998 and categorized these cases into 5 subgroups (basal-like, HR-expressing, Her2/neu-overexpressing, HR and Her2/neu-expressing, and null subtypes negative for all markers), based on the immunohistochemical data. We identified cases of 114 (14.7%) basal-like, 345 (44.5%) HR-expressing, 133 (17.1%) Her2/neu-overexpressing, 61 (7.8%) HR and Her2/neu-expressing, and 123 (15.9%) null subtypes. Histologically, most basal-like breast cancers were invasive ductal carcinoma, not otherwise specified (98 cases, 86.0%), with high nuclear and/or histologic grades, and most metaplastic carcinomas (6 [75.0%] of 8 cases) were the basal-like subtype. Both basal-like and Her2/neu-overexpressing subtypes were associated with larger tumor sizes (mean, 3.6 and 3.3 cm, respectively) than the HR-expressing group (mean, 2.8 cm) (P = .001 and P = .036, respectively). Nodal stage of Her2/neu-overexpressing subtype was higher than that of basal-like subtype; however, overall stage was not different between the 2 groups (P = .010 and .123, respectively). Distant metastasis was most frequently observed in the Her2/neu-overexpressing subtype (33.8%), which was prognostically the worst subgroup of breast cancers. In contrast to previous findings from Western countries, our analyses reveal that the Her2/neu status is the most important prognostic factor of breast cancers.
-
Am J Surg. 2006 May;191(5):657-64.
-
Metaplastic breast cancer: clinical significance.
Department of Surgery, Swedish Cancer Institute, Suite 400, 1221 Madison Street, Seattle, WA 98104, USA. david.beatty@swedish.org
BACKGROUND: Metaplastic breast carcinoma (MBC) is a rare poorly differentiated breast cancer characterized by coexistence of ductal carcinoma with areas of matrix producing, spindle-cell, sarcomatous, or squamous differentiation; ER/PR/HER2 negativity; and a reputation for poor outcome. METHODS: The Swedish Cancer Institute prospective breast cancer database (> 6500 patients; 1990-2005) has 24 MBC cases that were compared with typical breast cancer cases matched for age, date of diagnosis, stage, and ER/PR/HER2 status. RESULTS: The mean metaplastic primary tumor diameter was 2.5 cm. The histological/nuclear grade was high in 21 of 24 cases. No patient had distant metastasis. ER and/or PR receptor status was negative in all cases. HER2 was negative in 10 of 11 cases tested. EGFR (HER1) was positive in 7 of 7 cases tested. All patients had sentinel and/or axillary lymph node dissection and surgical resection; 18 received chemotherapy and 22 had radiation therapy. Four patients had distant recurrences 5 to 88 months from diagnosis. Five-year survival was 83% (95% confidence interval, 66-100%). Comparison with matched typical breast cancer cases revealed no major significant difference in multidisciplinary treatment patterns, recurrence, or survival. CONCLUSION: MBC is associated with poor prognostic indicators, but outcomes comparable with matched typical breast cancer cases can be achieved with routine aggressive multidisciplinary care. Increased, expression of EGFR (HER1) provides an opportunity for targeted tumor therapy.
-
J Clin Pathol. 2006 Oct;59(10):1079-83. Epub 2006 Feb 7.
-
Metaplastic carcinoma of the breast: a clinicopathological review.
Department of Anatomical and Cellular Pathology, Prince of Wales Hospital, Chinese University of Hong Kong, Hong Kong. garytse@cuhk.edu.hk
BACKGROUND: Mammary metaplastic carcinoma encompasses epithelial-only carcinoma (high-grade adenosquamous carcinoma or pure squamous cell carcinoma), biphasic epithelial and sarcomatoid carcinoma and monophasic spindle cell carcinoma. AIM: To evaluate the clinicopathological features of a large series of 34 metaplastic carcinomas. METHODS: 10 epithelial-only, 14 biphasic and 10 monophasic metaplastic carcinomas were assessed for nuclear grade, hormone receptor status, HER2/neu (cerbB2) oncogene expression, Ki-67 and p53, lymph node status and recurrence on follow-up. RESULTS: Intermediate to high nuclear grade were assessed in most (33/34) tumours. Oestrogen and progesterone receptors were negative in 8 of 10 epithelial-only, all 14 biphasic, and 9 of 10 monophasic tumours, cerbB2 was negative in 7 of 10 epithelial-only, all 14 biphasic and 8 of 10 monophasic tumours. Ki-67 was found to be positive in 6 of 10 epithelial-only, 6 of 14 biphasic, and 7 of 10 monophasic tumours, whereas p53 was positive in 6 of 10 epithelial-only, 7 of 14 biphasic, and 8 of 10 monophasic tumours. Lymph node metastases were seen in 7 of 7 epithelial-only, 7 of 11 biphasic, and 3 of 7 monophasic tumours. Recurrences were seen in 4 of 7 epithelial-only, 8 of 9 biphasic, and 4 of 9 monophasic tumours. CONCLUSIONS: All three subtypes of metaplastic carcinoma are known to behave aggressively, and should be differentiated from the low-grade fibromatosis-like metaplastic carcinoma, which does not metastasize. Oncological treatment options may be limited by the frequently negative status of hormonal receptor and cerbB2.
-
J Clin Pathol. 2005 Jul;58(7):700-4.
-
Metaplastic breast carcinomas are negative for Her-2 but frequently express EGFR (Her-1): potential relevance to adjuvant treatment with EGFR tyrosine kinase inhibitors?
Department of Pathology, Medical University of Graz, Auenbruggerplatz 25, A-8036 Graz, Austria. sebastian.leibl@klinikum-graz.at
BACKGROUND: Metaplastic carcinomas (MCs) of the breast rarely express steroid receptors and Her-2, which minimises the options for adjuvant treatment in patients with advanced disease. AIMS: To investigate the possible eligibility of patients with MCs for epidermal growth factor receptor (EGFR) targeted treatment. METHODS: Immunohistochemical assessment of the expression of steroid receptors and four members of the EGFR/Her family (EGFR/Her-1-4) in 20 MCs (eight with heterologous elements, seven spindle cell MCs, four carcinosarcomas, and one matrix producing carcinoma). Fourteen of the 20 MCs were positive for EGFR (Her-1). Among these cases, 1+, 2+, and 3+ reactivity were seen in two, four, and eight cases, respectively. Her-2 was only present in one MC with 1+ reactivity. Her-3 (1+ reactivity), Her-4 (2+ reactivity), and the androgen receptor (2+ reactivity) were also expressed by one tumour. Oestrogen and progesterone receptors (3+ reactivity each) were detected in the epithelial component only of two carcinosarcoma-type MCs. CONCLUSIONS: MCs express EGFR considerably more frequently than the types of breast carcinomas that have been investigated previously. Although molecular analyses for possible genetic alterations in the EGFR might be required, these results suggest that women suffering from this aggressive form of breast carcinoma might benefit from treatment with protein kinase inhibitors, such as gefitinib.