| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 一个病例引发的思考......
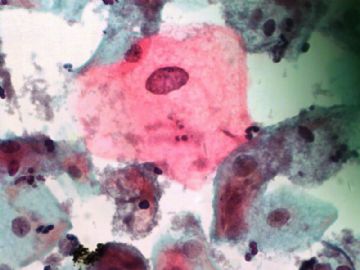
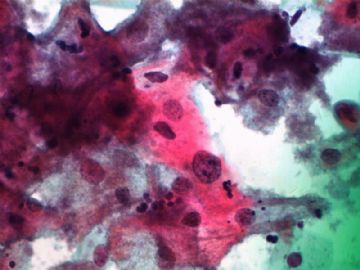
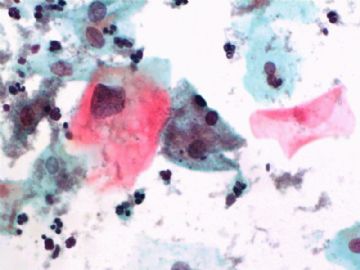
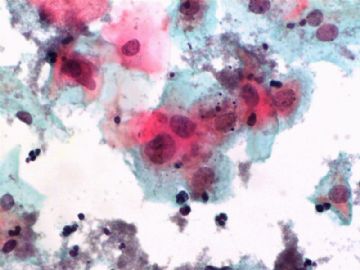
| 以下是引用wq_9603在2009-6-26 11:25:00的发言:
杨斌老师意见: 他的基础上我再增加点。对于细胞学诊断为LSIL但组织学诊断CIN1的比例较低的原因,可能和以下几 点有关,但不仅仅局限于以下这些原因: LSIL/ASC者会自发性恢复正常,原因可能与机体免疫机制有关。因此大部分ASC/LSIL女性其实是所谓 的“一过性HPV感染”。这种一过性感染的分子基础其实是HPV仅仅在感染上皮的阶段,尚没有整合到 宿主的基因组中。因此仅仅有很少的甚至没有病毒的癌蛋白(即E6和E7)产生。当前大部分女性患者 的CIN1被妇科或病理医生认为是HPV感染,但尚无新生物阶段。这就是为什么最新的ASCCP指南告诉临 床对于LSIL/CIN1者仅仅进行每年一次的液基检查即可的原因。 |
翻译的很好。 Colposcopy at the cross roads 可以直译为“十字路口的阴道镜”,其实可以意译为“阴道镜检查何去何从”。仅供参考。

- 不坠青云之志,长怀赤子之心
-
陈隆文博士意见:
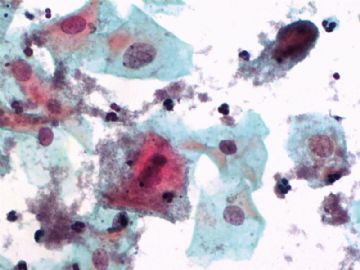
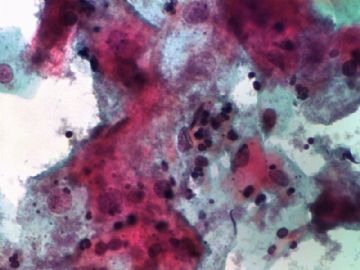
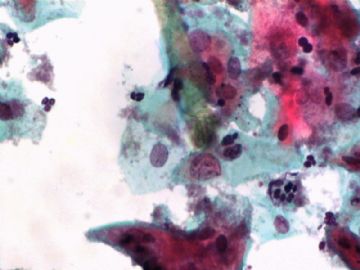
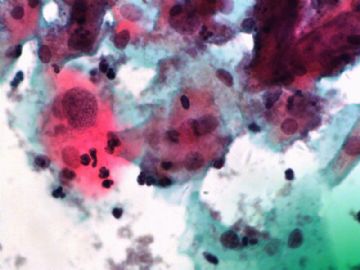
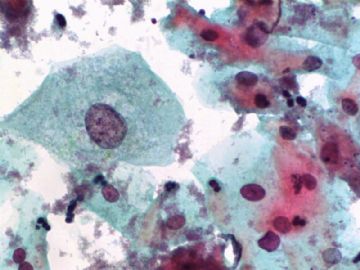
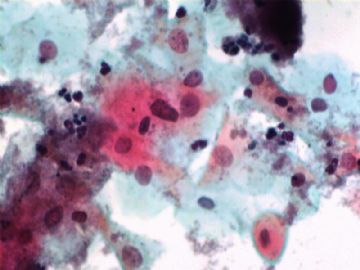
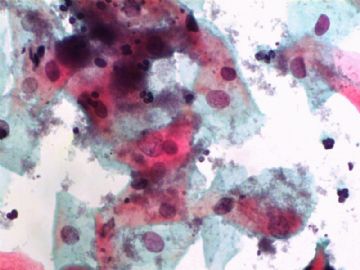
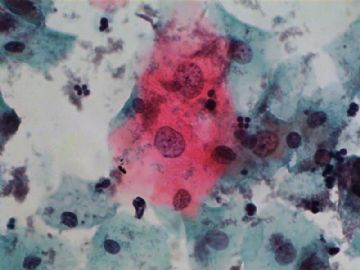
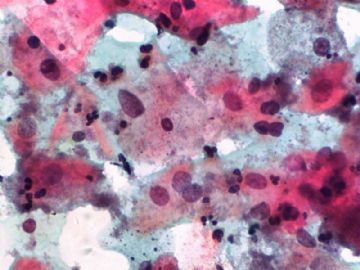
根据你所给的图片,我会毫不犹豫的签发LSIL。赵老师和杨老师已经对于液基检查为LSIL但是活检阴性病例给出了详细的科学依据。我再说点稍微“不太科学”的观点:
1)外科病理学家对CIN1尚不能达成完全一致的意见,但是这并不影响患者的治疗。因此在乎这个做什么?只要不漏诊CIN2的病例,患者仅仅是要接受每年一次的液基检查就是了。
2)在美国,液基报告也是会引起法律纠纷的。但是,正如Dr.Jack Frable常说的,在他所遇到的包括液基引起的法律纠纷中,大部分是因为漏掉了高级别病变,也就是说诊断力度小了。过诊断一般不会引起麻烦的。我还没听说过因为过诊断LSIL而引起麻烦的。
总而言之,我会签一个LSIL然后回家和我的孩子玩去,不会再考虑这个病例,也不会再因为这个病例而怀疑我自己。

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
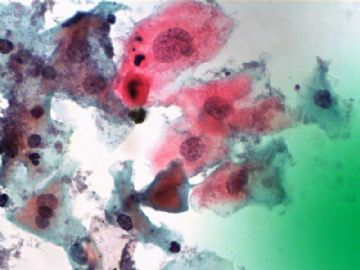
杨斌老师意见:
同意LSIL诊断。Dr.Zhao用他的第一手资料为我们提供了细胞学和组织学之间联系的最科学的依据。在
他的基础上我再增加点。对于细胞学诊断为LSIL但组织学诊断CIN1的比例较低的原因,可能和以下几
点有关,但不仅仅局限于以下这些原因:
1)由美国国立卫生研究院组织的最权威性的ALTS研究表明,超过91%的HPV阳性、细胞学检查为
LSIL/ASC者会自发性恢复正常,原因可能与机体免疫机制有关。因此大部分ASC/LSIL女性其实是所谓
的“一过性HPV感染”。这种一过性感染的分子基础其实是HPV仅仅在感染上皮的阶段,尚没有整合到
宿主的基因组中。因此仅仅有很少的甚至没有病毒的癌蛋白(即E6和E7)产生。当前大部分女性患者
的CIN1被妇科或病理医生认为是HPV感染,但尚无新生物阶段。这就是为什么最新的ASCCP指南告诉临
床对于LSIL/CIN1者仅仅进行每年一次的液基检查即可的原因。
2)我们国内及其他研究发现,CIN2患者中约50%阴道镜下取活检没有发现。我们还发现CIN2中超过37%的患者是在冰醋酸阴性区域检出的病变。最近Dr.Mark Schiffman发表的一篇名为“十字路口的阴道镜”的综述中提到,大约55%的CIN2病变被临床常规的活检所遗漏。因此,可以这样说:阴道镜下对醋酸涂抹变白的区域活检,与宫颈癌预防和治疗之间的关系是很微弱的。

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
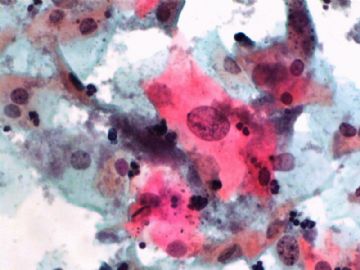
cqzhao老师意见:
同意LSIL的诊断。液基本身就是个筛查性的检查,在液基中检查出LSIL的患者很可能组织学检查是阴
性。原因:1)组织学取材没有到位;2)病变很小,自行恢复了(?);3)液基中不是LSIL。即使过
诊断导致你发了LSIL,问题也不大。对于上面一例我认为发LSIL还是可以的。对于LSIL患者进行活检
的目的是为了看有没有更高级别的病变,甚至是肿瘤。
从我的研究也可以看出,对719例液基诊断为LSIL的患者做的组织学活检表明,12.9%的患者为CIN2/3
,55.8%的患者为CIN1.换句话说,超过30%的液基检查为LSIL的患者在接下来的活检中没有发现CIN。
以上数据来自我的研究,文章已经投稿待发。尽我所能所查到的资料表明,这项研究是液基发现LSIL
后进行组织学活检和HPV检测的目前最大的研究

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
Based on the photos you provided, I would sign-out this case as LSIL without hesitation. Drs. Yang and Zhao have already provided detailed scientiific evidence to elaborate the reasons that LSIL Paps can have negative biopsy. I just want to add few not very "scientific" points:
1) Surgical pathologists can not always reach consensus on CIN1, but, this does not affect the patient management, so who cares. As long as you do not miss CIN2+, the patient will just get follow-up by Pap test;
2) Pap test is an area of getting law suit in the US. But, as Dr. Jack Frable always said in his lecture about law suits involving Pap, almost all the law suits are because the cytology lab "miss" a high-grade lesion, which means under-calling, over-calling a high-grade lesion rarely get you in trouble. I have never heard of "over-calling" LSIL can get you in trouble.
In summary, I will sign this case out as LSIL and go home playing with my kids, never think about it or second guess myself again on this case.
同意LSIL诊断。 Dr. Zhao has provided the best scientific evidence for cytologic-histologic correlation based his first hand experience. I would like to provide couple supplementary points following his comments. The reasons that lower rate CIN1 detection histologically for patients cytologically diagnosed as LSIL include, but not limited to, the followings:
1) Based on most powerful ALTS study conducted by NIH, up to 91% women with HPV-positive and cytologically LSIL/ASC will spontaneously regress back to normal, probablly due to the self-cleaning mechanism immunologically. Therefore, most of ASC/LSIL women have so-called "transient HPV infection". The molecular basis of this "transient infection" is that HPV is biologically in its "episomal stage" which is not integrated into the host genome. Thus, no or minimal amount of viral oncoproteins, E6 and E7, produced. Currently CIN1 is considered by most gynecologic doctors and pathologists as a "HPV infected, but non-neoplastic process" in most women. That is why currently the clinical management on LSIL/CIN1 has been loosen up with annual PAP test follow up only in recent ASCCP guideline.
2) Based on our study in China (SPOCCS) and others, we found that about 50% of CIN2+ lesions were missed by colposcopically guided biopsy. We also found that up to 37% of CIN2+ lesions were detected in those areas read as negative after 冰醋酸. These areas are not biopsied in normal clinical settings. In recent review article by Dr. Mark Schiffman with a title of " Colposcopy at the cross road", he stated that about 55% of CIN2 lesions were missed by routine biopsy by clinicians. It is reasonablly to say that colposcopy-guided biopsy based on acetic white changes is the weakest link in cervical cancer prevention and treatment paradigm.

- 不坠青云之志,长怀赤子之心